When your MS symptoms suddenly get worse, it’s natural to panic. Did your disease flare up again? Are you getting worse? But what if the spike in symptoms isn’t a relapse at all? What if it’s something called a pseudorelapse - a temporary glitch with no new damage, no inflammation, and no need for steroids?
Many people with MS go through this. One day, your vision blurs, your legs feel heavy, or you can’t hold a cup steady. You call your neurologist. You’re told to head to the hospital for IV steroids. But if you’re dealing with a pseudorelapse, those steroids won’t help. And worse - they might hurt you.
What’s the Real Difference?
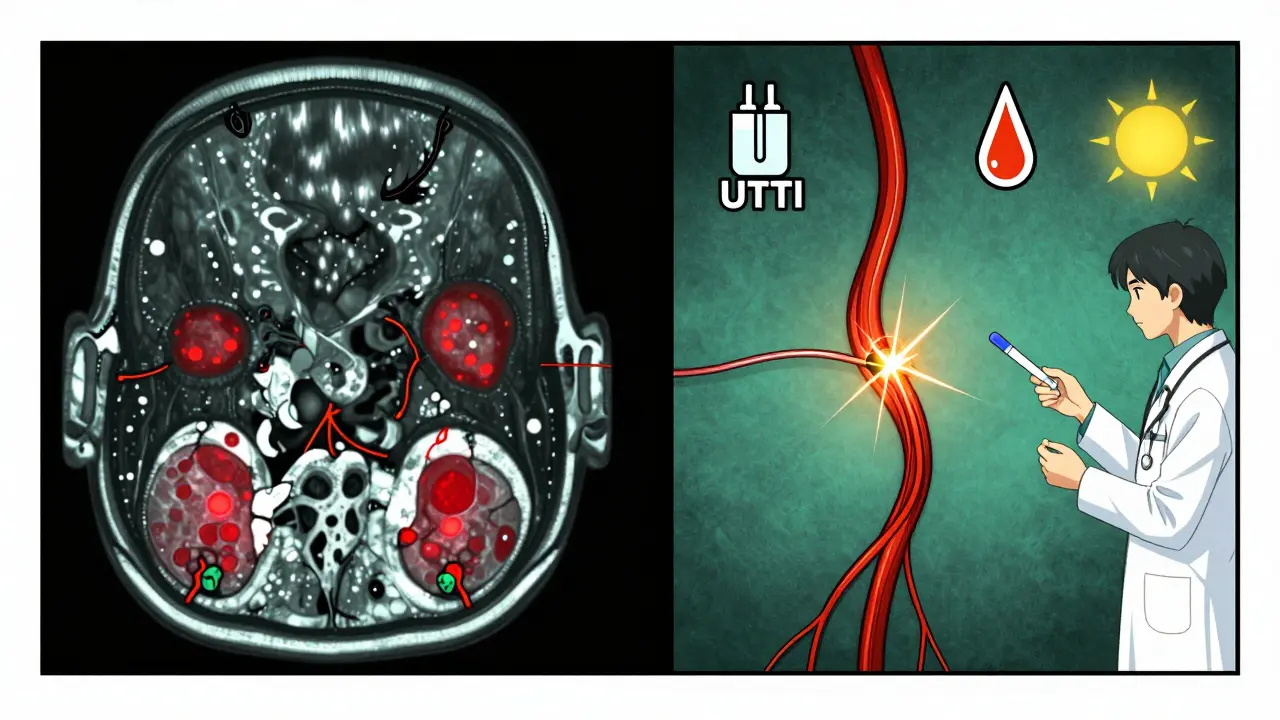
A true MS relapse happens because your immune system attacks your central nervous system. New inflammation damages the myelin sheath around your nerves. That’s what causes new symptoms or a major worsening of old ones. These symptoms last at least 24 to 48 hours - often longer - and show up without any obvious outside cause like a fever or heat exposure.
A pseudorelapse is completely different. There’s no new damage. No fresh inflammation. No new lesions on your MRI. Instead, your nerves - already weakened by past MS damage - are temporarily overwhelmed by something else. Heat. Infection. Stress. Your body’s already running on borrowed time, and this extra pressure pushes it over the edge. Symptoms feel just as real, but they vanish once the trigger is gone.
Think of it like a frayed electrical wire. A true relapse is like a new short circuit. A pseudorelapse is like turning up the voltage on an old wire - it flickers, maybe even sparks, but the wire itself isn’t broken any further.
What Triggers a Pseudorelapse?
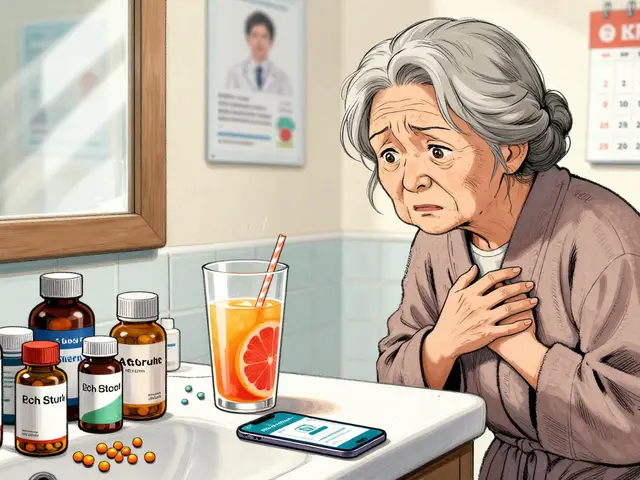
Pseudorelapses aren’t random. They’re tied to clear, avoidable triggers. The most common one? Infections - especially urinary tract infections (UTIs). Studies show UTIs trigger nearly two out of every three pseudorelapses. That’s why if you suddenly feel worse and you’ve had a burning sensation when peeing, a fever, or just felt generally off - don’t assume it’s MS acting up. Get a urine test first.
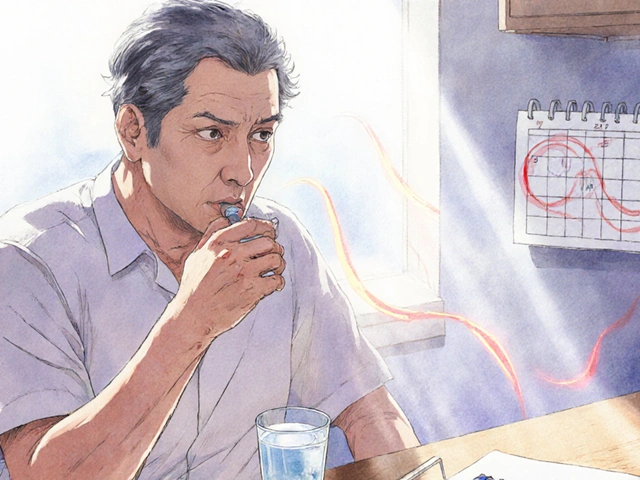
Heat is another big one. Around 41% of people with MS experience Uhthoff’s phenomenon - a temporary worsening of symptoms when body temperature rises. That means a hot shower, a sauna, a humid day, or even a fever from the flu can make your vision blurry, your legs weak, or your balance off. The moment you cool down, symptoms fade. No steroids needed.
Other common triggers:
- Fever (over 37.8°C / 100°F)
- Physical exhaustion or overexertion
- High stress levels
- Dehydration
- Low sodium or other metabolic imbalances
Here’s the catch: these triggers don’t cause new MS damage. They just make your existing nerve problems worse. That’s why cooling off, treating the infection, or resting often fixes everything in hours - not weeks.
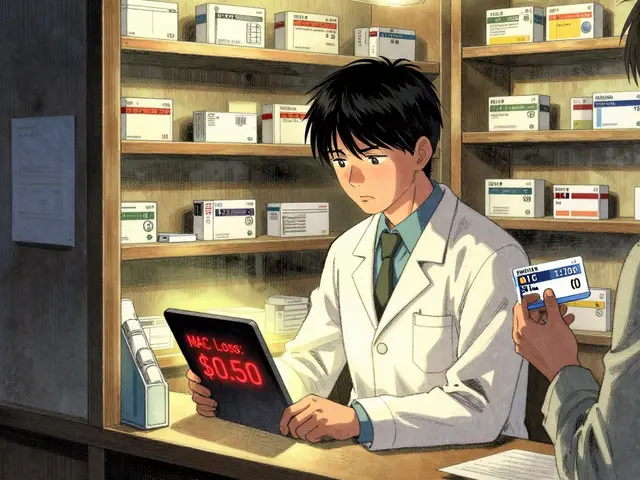
Why Steroids Don’t Work for Pseudorelapses
Steroids like IV methylprednisolone are powerful anti-inflammatories. They work great for true relapses because they calm the immune system’s attack on your nerves. But if there’s no attack - no inflammation - steroids have nothing to fight.
Studies show that 30 to 40% of people with MS get unnecessary steroid treatment because their pseudorelapse was misdiagnosed as a true relapse. And the side effects? They’re real and risky:
- High blood sugar - happens in 25% of patients
- Insomnia - affects 40%
- Mood swings, anxiety, even steroid-induced psychosis
- Weakened immune system - increasing your risk of other infections
One nurse with MS shared on Reddit that she’d seen five patients in a year get IV steroids for UTI-triggered pseudorelapses. One ended up in the hospital with steroid psychosis. That’s not just unnecessary - it’s dangerous.
For pseudorelapses, the treatment isn’t steroids. It’s identifying and removing the trigger. Antibiotics for a UTI. Cooling vests for heat. Rest for exhaustion. Hydration for dehydration. Simple, safe, and effective.
How to Know Which One You’re Facing
There’s no single test, but there’s a clear process doctors follow:
- Check the timeline. Did symptoms last more than 24 hours? If they faded in a few hours after you cooled down or took antibiotics, it’s likely a pseudorelapse.
- Rule out triggers. Get a temperature check. Do a urine test. Check your blood sodium levels. If you’ve had a fever, infection, or heat exposure in the last 48 hours, that’s your likely cause.
- Look at your history. If you’ve had the same symptom before - like vision trouble in hot weather - and it always goes away with cooling, it’s probably Uhthoff’s phenomenon.
- Consider an MRI. If you’re still unsure, an MRI can show if there are new lesions. No new lesions? Likely a pseudorelapse.
Experts recommend keeping a symptom diary. Note when symptoms start, how long they last, what you were doing, your temperature, if you were sick, or if you were stressed. This helps your neurologist spot patterns. One patient in Melbourne told me she started tracking her daily temperature and noticed her leg weakness always spiked when she took hot baths after work. She switched to lukewarm showers - and the problem vanished.
Who’s Most at Risk for Pseudorelapses?
Pseudorelapses are more common in people who’ve had MS for a long time. Why? Because their nervous system has more damaged pathways. Even a small extra stressor - like a mild cold - can overload those weak signals.
Older patients, especially over 55, are also more vulnerable. After a pseudorelapse, 15% of them don’t fully bounce back to their previous level of function - not because of new damage, but because they’ve become deconditioned during the episode. That’s why staying active, even during flare-ups, matters.
And while true relapses become less frequent over time, pseudorelapses become more common. That’s why knowing the difference isn’t just helpful - it’s essential for long-term management.

What You Can Do Today
You don’t need to wait for a neurologist to figure this out. Here’s what you can do right now:
- If you feel worse, check your temperature. If it’s above 37.8°C, assume it’s a trigger - not a relapse.
- Drink water. Dehydration can mimic or worsen MS symptoms.
- Check for signs of infection: burning pee, cough, sore throat, fever.
- Use cooling tools: damp towels, cooling vests, air conditioning. Even sitting in front of a fan can help.
- Don’t rush to the hospital for steroids. Call your neurologist first. Ask: “Could this be a pseudorelapse?”
There’s a tool called the MS-Relapse Assessment Tool (MS-RAT) that’s now being used in clinics. It asks about symptom duration, temperature, and functional impact to give a probability score. It’s 92% accurate. You can ask your doctor if they use it - or even look for patient versions online.
The Bigger Picture
Misdiagnosing a pseudorelapse as a true relapse doesn’t just waste time. It costs the U.S. healthcare system over $12 million a year in unnecessary treatments and complications. But beyond money, it’s about quality of life.
When you’re told you need steroids, you feel like your disease is getting worse. That’s terrifying. But if you’re told, “This is heat, not progression,” it’s empowering. You learn to manage it. You take control. You avoid side effects. You keep living.
One woman I spoke to, who’s had MS for 18 years, said: “I used to dread every symptom change. Now I know - if I’m hot or tired or have a UTI, I fix that first. I don’t reach for the steroids. My body’s been through enough.”
Understanding the difference between relapse and pseudorelapse isn’t just medical knowledge. It’s your best tool for staying in control - without unnecessary drugs, hospital visits, or fear.
How do I know if my symptoms are a true MS relapse or a pseudorelapse?
Start by checking for triggers: fever, infection (especially UTI), heat exposure, or stress. If symptoms started after one of these and improve within hours of removing the trigger, it’s likely a pseudorelapse. True relapses last at least 24-48 hours without a clear trigger and often involve new neurological changes. An MRI showing new lesions confirms a true relapse.
Can pseudorelapses cause permanent damage?
No. Pseudorelapses do not cause new inflammation or nerve damage. They’re temporary disruptions in nerve signaling due to stress on already damaged pathways. Once the trigger is removed, symptoms resolve. However, prolonged weakness or deconditioning during a pseudorelapse can temporarily reduce function - especially in older adults - but this isn’t permanent MS progression.
Why are steroids sometimes given for pseudorelapses?
Because the symptoms feel identical to a true relapse. Many patients and even some doctors don’t recognize the difference. Studies show 30-40% of pseudorelapses are incorrectly treated with steroids. This exposes patients to serious side effects - like high blood sugar, insomnia, mood swings, and increased infection risk - without any benefit.
What is Uhthoff’s phenomenon?
Uhthoff’s phenomenon is a type of pseudorelapse where symptoms - especially vision problems, weakness, or fatigue - worsen when body temperature rises. It affects 60-80% of MS patients who’ve had optic neuritis. Cooling down reverses the symptoms within minutes to hours. It’s not a relapse - it’s a heat-sensitive nerve response.
Should I get an MRI every time my symptoms worsen?
Not always. If a clear trigger like fever or heat is present and symptoms improve quickly, an MRI isn’t needed. But if symptoms are new, severe, last more than 48 hours, and no trigger is found - an MRI helps confirm whether new lesions have formed. Your neurologist will decide based on your history and symptom pattern.
Can I prevent pseudorelapses?
Yes. Stay cool - use cooling vests, avoid hot showers, and keep your home air-conditioned. Prevent infections by drinking water, practicing good hygiene, and getting annual flu and pneumonia shots. Manage stress with rest and mindfulness. Keep a symptom diary to spot your personal triggers. Prevention is more effective than treatment.



Lynsey Tyson
December 20, 2025 AT 10:36I used to panic every time my legs went numb until I learned about pseudorelapses. Last winter, I got a UTI and couldn’t walk straight for 12 hours - thought it was a relapse, called my neurologist at 2 a.m. Turned out, antibiotics and a cold shower fixed it. No steroids. No drama. Just common sense.
Allison Pannabekcer
December 20, 2025 AT 18:09Heat is the silent saboteur. I used to take hot baths after work - felt amazing, until my vision started swimming. Didn’t connect it to MS until I read about Uhthoff’s. Now I keep a cooling towel in the fridge and a fan by my desk. Simple changes, huge difference. No one talks about this enough.
And dehydration? I used to think ‘just drink water’ was generic advice. Turns out, my brain fog cleared within an hour of hydrating after a long drive. It’s not magic - it’s physics. Nerves need balance.
My neurologist finally admitted they misdiagnosed two of my ‘relapses’ as flare-ups. Steroids made me crash for weeks. Now I track my temp, pee habits, and stress levels like a detective. It’s not paranoia - it’s survival.
anthony funes gomez
December 21, 2025 AT 20:23The distinction between relapse and pseudorelapse is ontologically critical: one involves demyelinating inflammation (a neuroimmunological event), the other is a transient conduction block in axons compromised by prior injury - a biomechanical failure under thermal or metabolic load. Steroids target cytokine cascades; they do nothing for sodium channel dysfunction induced by hyperthermia. The clinical confusion arises from phenomenological overlap - identical symptomatology, divergent etiologies. Yet, the therapeutic implications are diametrically opposed. Misapplication of immunosuppressants in the absence of active inflammation constitutes iatrogenic harm. Empirical validation via MRI is not always necessary - temporal dynamics and trigger correlation are sufficient for differential diagnosis in 87% of cases. We need standardized protocols, not guesswork.
Dikshita Mehta
December 23, 2025 AT 05:50As someone who’s had MS for 12 years, I can confirm: UTIs are the #1 trigger. I’ve had three pseudorelapses in the last year - all from silent UTIs. No burning, no fever, just weird fatigue and leg heaviness. Urine test showed infection. Antibiotics - 24 hours later, back to normal. No steroids. No hospital. My advice? If you feel off, test your urine before you panic. It’s cheap, fast, and saves you from side effects you didn’t ask for.
Also, cooling vests are a game-changer. I wear mine in summer. My balance improved just by keeping my core temp down. No magic, just science.
Gloria Parraz
December 24, 2025 AT 06:39I used to cry every time my symptoms flared - terrified I was getting worse. Then I learned about pseudorelapses. I started keeping a journal: temperature, stress level, what I ate, if I’d been sitting too long. Within two weeks, I spotted a pattern - my hands went numb every time I skipped breakfast and worked 10 hours. Low sodium. Dehydration. I started eating protein with my coffee and drinking a liter before work. The numbness? Gone. Not because MS got better - because I stopped setting my body on fire.
Stop waiting for the hospital. Start watching yourself. You’re not broken. You’re just running on a system that needs better maintenance.
Sahil jassy
December 25, 2025 AT 22:38Carolyn Benson
December 27, 2025 AT 08:31You think this is about MS? It’s about control. The system wants you scared. Wants you dependent on drugs, on hospitals, on the idea that your body is failing. But what if your body isn’t failing - it’s just overloaded? What if the real enemy isn’t inflammation, but ignorance? Steroids are a band-aid on a broken system. They make you feel like you’re being ‘treated’ - while the real solution - rest, hydration, cooling - is dismissed as ‘lifestyle advice.’ Don’t be fooled. This isn’t medicine. It’s a performance. And you’re the audience.
Chris porto
December 28, 2025 AT 16:07I’ve had MS for 15 years. I’ve had three true relapses. I’ve had maybe 12 pseudorelapses. The difference? One felt like my body was breaking. The others felt like my body was tired. Once I learned to listen - not just to my neurologist, but to my own rhythm - everything changed. I stopped rushing to the ER. I started checking my temp, drinking more water, and saying no to extra work when I was drained. It’s not about being ‘strong.’ It’s about being smart. And honestly? It’s the most powerful thing I’ve done for my MS.