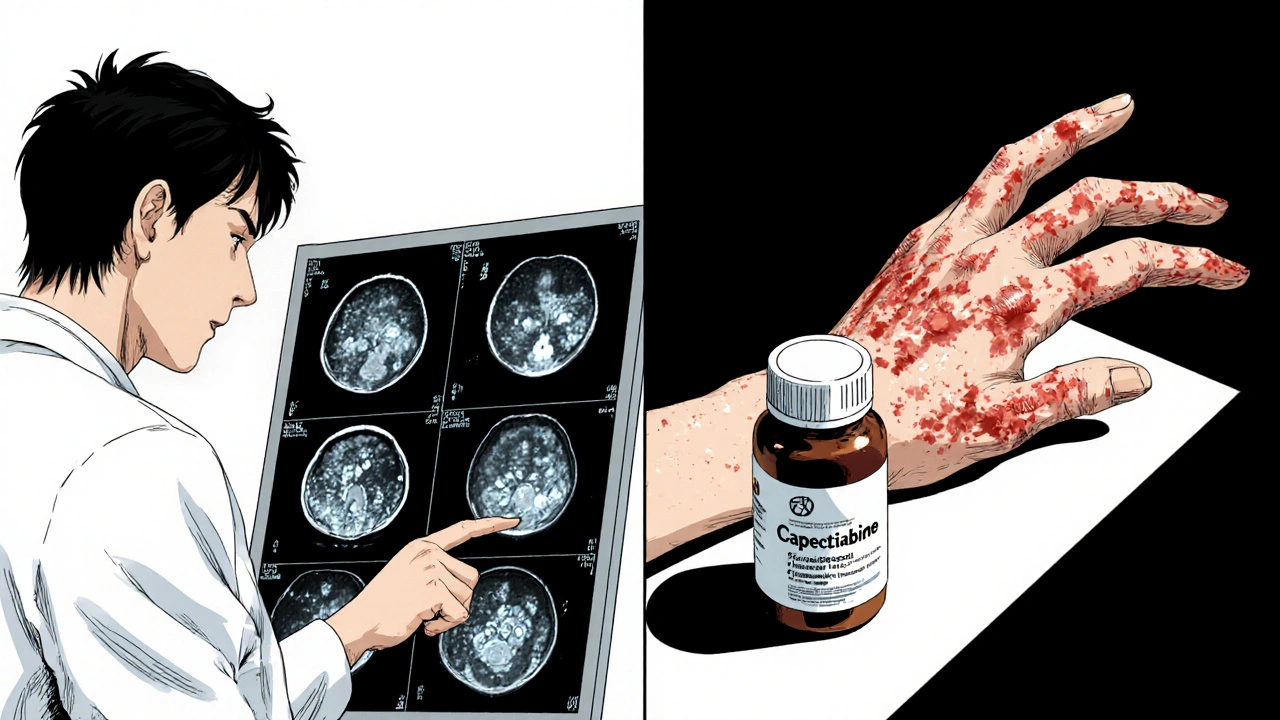
When most people think of chemotherapy, they picture IV drips and hospital visits. But for some types of skin cancer, a simple pill taken at home can be just as powerful. That’s where capecitabine comes in. It’s not the first drug that comes to mind for skin cancer, but for certain cases-especially when surgery or radiation isn’t an option-it’s become a critical tool in oncology.
What is capecitabine, really?
Capecitabine is an oral chemotherapy drug. It’s a prodrug, meaning it doesn’t work until your body converts it into its active form: 5-fluorouracil (5-FU). This conversion happens mostly in tumor cells, which helps target the cancer while sparing healthy tissue a bit more than traditional IV chemo. It’s been used for over 20 years, mainly for breast and colorectal cancers. But in the last decade, doctors have started using it off-label for advanced skin cancers that don’t respond to other treatments.
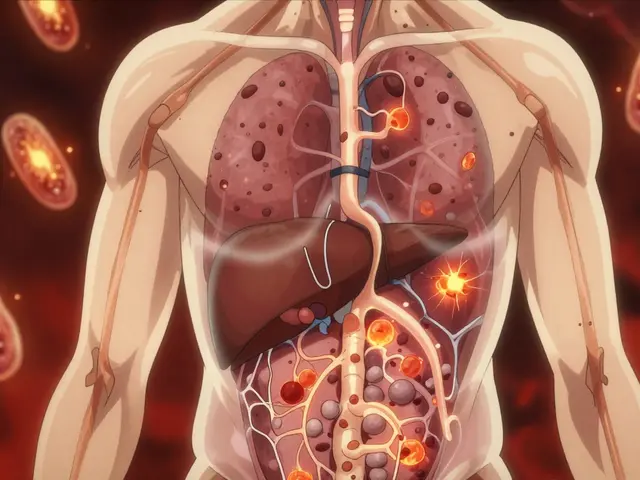
Unlike surgery or radiation, which are local treatments, capecitabine works systemically. That makes it useful when cancer has spread beyond the skin-like to lymph nodes or internal organs. It’s especially helpful for patients with advanced squamous cell carcinoma or Merkel cell carcinoma that’s no longer responding to immunotherapy or targeted drugs.
Which skin cancers respond to capecitabine?
Not all skin cancers are the same. Melanoma, the deadliest form, usually doesn’t respond well to capecitabine. But two other types do: cutaneous squamous cell carcinoma (cSCC) and Merkel cell carcinoma (MCC).
For cSCC, surgery is the gold standard. But when the tumor is too large, has invaded nerves, or has spread, options shrink. In a 2021 study published in the Journal of the American Academy of Dermatology, 37 patients with advanced cSCC who had failed other treatments were given capecitabine. Nearly 40% saw their tumors shrink, and about 20% had stable disease for over six months. That’s meaningful when you’ve run out of other choices.
Merkel cell carcinoma is rarer but more aggressive. When it spreads, it’s often deadly. Immunotherapy like pembrolizumab is first-line, but not everyone responds. For those who don’t, or can’t tolerate immunotherapy, capecitabine has shown promise. A 2023 case series from Memorial Sloan Kettering found that 5 out of 12 patients with metastatic MCC had partial responses after starting capecitabine, with some living over a year without disease progression.
How do you take it?
Capecitabine comes in tablet form. The standard dose is 1,250 mg per square meter of body surface area, taken twice a day-morning and evening-for two weeks, then a one-week break. This three-week cycle repeats. It’s taken with food and a full glass of water to reduce stomach upset.
Patients usually start feeling side effects within the first week: fatigue, nausea, hand-foot syndrome (redness, peeling, pain in palms and soles), and diarrhea. Hand-foot syndrome is the most common reason people need to lower their dose or pause treatment. But most side effects improve after stopping the drug or adjusting the schedule.
Unlike IV chemo, you don’t need to go to a clinic every week. You pick up your pills at the pharmacy. That’s a huge advantage for people living far from cancer centers or those who need to keep working or caring for family.
Who benefits most from capecitabine?
It’s not for everyone. Capecitabine works best in patients with:
- Advanced or metastatic cutaneous squamous cell carcinoma
- Merkel cell carcinoma that’s resistant to immunotherapy
- Good liver and kidney function (the drug is processed through both)
- No history of severe diarrhea or hand-foot syndrome from other drugs
- Ability to take pills reliably at home
It’s rarely used as a first-line treatment. Doctors usually try surgery, radiation, or immunotherapy first. But when those fail-or aren’t possible-capecitabine becomes a lifeline. It’s especially valuable for older patients who can’t handle aggressive treatments or those with multiple health problems.
How does it compare to other options?
Here’s how capecitabine stacks up against other treatments for advanced skin cancer:
| Treatment | Delivery | Response Rate | Common Side Effects | Best For |
|---|---|---|---|---|
| Capecitabine | Oral pill | 30-40% | Hand-foot syndrome, diarrhea, fatigue | Patients who can’t tolerate IV chemo or immunotherapy |
| Pembrolizumab (Keytruda) | IV infusion | 50-60% | Immune-related reactions, fatigue | First-line for MCC and cSCC |
| Cisplatin + 5-FU | IV infusion | 40-50% | Nausea, kidney damage, hearing loss | Younger, healthier patients |
| Topical 5-FU | Applied to skin | 70-80% for early lesions | Redness, burning, blistering | Superficial, non-invasive tumors |
Capecitabine isn’t as effective as immunotherapy for most patients, but it’s easier to manage and often cheaper. It’s also an option when immunotherapy isn’t available or covered by insurance. In rural Australia, where access to specialty oncology is limited, oral drugs like capecitabine make a real difference.

What are the risks and limitations?
Capecitabine can cause serious side effects. About 1 in 10 patients develop severe hand-foot syndrome that requires dose reduction. Diarrhea can lead to dehydration if not managed early. Some people develop low white blood cell counts, increasing infection risk.
It’s not safe during pregnancy. If you’re thinking of having children, talk to your doctor before starting. Also, avoid alcohol and certain painkillers like ibuprofen during treatment-they can worsen side effects.
Another limitation: it doesn’t work for everyone. Some tumors simply don’t respond, and there’s no reliable test to predict who will benefit. Doctors rely on trial and error. If there’s no sign of improvement after two cycles (six weeks), they usually switch to another option.
What’s next for capecitabine in skin cancer?
Researchers are now testing capecitabine in combination with other drugs. Early trials are combining it with immunotherapy or targeted agents like EGFR inhibitors. The goal is to make it more effective and reduce resistance.
In Australia, clinical guidelines from the Therapeutic Goods Administration don’t yet list capecitabine as a standard treatment for skin cancer. But many oncologists use it off-label based on real-world evidence. As more data comes in, it could become a formal recommendation.
For now, it’s a quiet hero. No flashy ads. No viral TikTok videos. But for patients with no other options, it’s giving them months-sometimes years-of better quality life.
Is capecitabine used for melanoma?
No, capecitabine is not effective for melanoma. Melanoma responds better to immunotherapy (like pembrolizumab) or targeted therapies (like BRAF/MEK inhibitors). Capecitabine is mainly used for squamous cell carcinoma and Merkel cell carcinoma.
Can you take capecitabine if you have kidney problems?
Capecitabine is cleared by the kidneys, so it’s not recommended for people with severe kidney impairment. Doctors check kidney function with blood tests before starting. If kidney function is mildly reduced, the dose may be lowered. But if it’s significantly impaired, alternatives are used.
How long does it take for capecitabine to work?
It usually takes 6 to 12 weeks to see a response. Doctors typically wait until after two treatment cycles (six weeks) before doing a scan to check if the tumor is shrinking. Some patients see improvement sooner, but patience is key.
Does capecitabine cause hair loss?
Unlike many chemotherapy drugs, capecitabine rarely causes complete hair loss. Some people notice thinning or increased shedding, but it’s usually mild. Most patients keep their hair, which is one reason it’s preferred for quality-of-life reasons.
Can you drink alcohol while taking capecitabine?
It’s best to avoid alcohol. Alcohol can increase the risk of liver toxicity and worsen side effects like nausea and dehydration. Even moderate drinking can interfere with how your body processes the drug. Always check with your oncologist before having any alcohol.
Final thoughts
Capecitabine isn’t a miracle drug. But for patients with advanced skin cancer who’ve run out of options, it’s one of the few tools left that’s both effective and manageable. It doesn’t require daily clinic visits. It doesn’t always cause hair loss. And for many, it means more time at home-with family, with routine, with dignity.
The science behind it is still evolving. But right now, in clinics across Australia and beyond, it’s helping people live longer-and better-than they thought possible.





Bob Martin
October 29, 2025 AT 10:43Capecitabine is basically chemo you can buy at CVS. No IVs, no needles, just pop a pill and hope your liver doesn’t quit on you. Works better than people think for squamous cell when everything else fails.
Sage Druce
October 30, 2025 AT 02:08This is the kind of treatment that changes lives without making you look like you’re in a war zone. No wig needed. No hospital chair for weeks. Just pills and patience. For older folks or people with jobs and kids, this is gold.
Bart Capoen
October 31, 2025 AT 01:50hand foot syndrome is the real MVP of side effects. i got it on my first cycle and thought i was gonna lose my fingers. turned out it just meant i had to stop using my phone for a week. weird tradeoff but i’ll take it over losing hair
Linda Patterson
October 31, 2025 AT 15:36Of course the Americans are the only ones using this off-label. In Europe they have real protocols. This is why our healthcare system is better. You can't just throw pills at cancer and call it science
Jen Taylor
October 31, 2025 AT 17:00Just wanted to say-this post was so clear and kind. I’m a nurse in rural Kansas, and I’ve seen patients cry because they could finally take their meds at home instead of driving three hours for an IV. Capecitabine isn’t glamorous, but it’s dignified. Thank you for writing this.
Cecil Mays
November 2, 2025 AT 08:26Yessss this is the kind of treatment that deserves more attention 🙌 No hair loss? Oral? Can be taken while working? Sign me up for the capecitabine fan club 💪🫶
Natalie Eippert
November 2, 2025 AT 19:52They say it's for advanced cases but honestly if you're not willing to fight with immunotherapy first you're just giving up. This is the lazy man's chemo. If you can't handle a clinic visit you shouldn't be getting treatment at all
Sarah Schmidt
November 3, 2025 AT 10:10There’s a deeper metaphysical truth here. Capecitabine doesn’t cure cancer-it reveals the quiet resilience of those who refuse to be defined by their diagnosis. The pill is not the hero. The person taking it, day after day, with no fanfare, that’s the real miracle. We’ve lost sight of that in our obsession with flashy cures
Tyler Mofield
November 4, 2025 AT 00:24Capecitabine is a prodrug metabolized via thymidine phosphorylase into 5-FU with preferential intratumoral activation. Efficacy in cSCC and MCC is supported by phase II data with ORR ranging 30-40% per JAMA Dermatology 2021. Renal clearance necessitates eGFR >30. Hand-foot syndrome incidence exceeds 60% grade 1-2. No controlled trials versus platinum regimens exist
Patrick Dwyer
November 6, 2025 AT 00:14As someone who works with veterans in rural clinics, I’ve seen how this drug keeps people connected to their lives. They’re not just patients. They’re parents, teachers, mechanics. Capecitabine lets them show up-not just survive, but be present. That’s not just medicine. That’s humanity.
luna dream
November 7, 2025 AT 02:51They’re hiding the truth. Capecitabine was designed by Big Pharma to keep people dependent on pills instead of curing them. The hand-foot syndrome? That’s not a side effect-it’s a control mechanism. Look up the patents. They don’t want you to heal. They want you to keep buying.