When your child misses a dose of medicine, panic is normal. But reacting the wrong way-like doubling up to make up for it-can be dangerous. Kids aren’t small adults. Their bodies process drugs differently, and even a small overdose can cause serious harm. The good news? There are clear, science-backed rules to follow that keep your child safe without adding stress.
Don’t Double the Dose-Ever
This is the most important rule: never give two doses at once. Doubling a missed dose increases the risk of severe side effects by 278% in children under 12, according to pediatric safety experts. Kids’ livers and kidneys aren’t fully developed, so they can’t clear medications as quickly as adults. A double dose of antibiotics, pain relievers, or seizure meds can lead to vomiting, drowsiness, breathing trouble, or even organ damage.
One parent on a parenting forum said they doubled their child’s amoxicillin dose because they forgot it in the morning and didn’t want to miss the full 24-hour cycle. The child ended up in the ER with severe diarrhea and dehydration. That’s not rare. Studies show nearly 63% of caregivers admit to doubling doses at least once to ‘stay on schedule.’ Don’t be one of them.
Use the Time-Based Rule: It Depends on How Often the Medicine Is Given
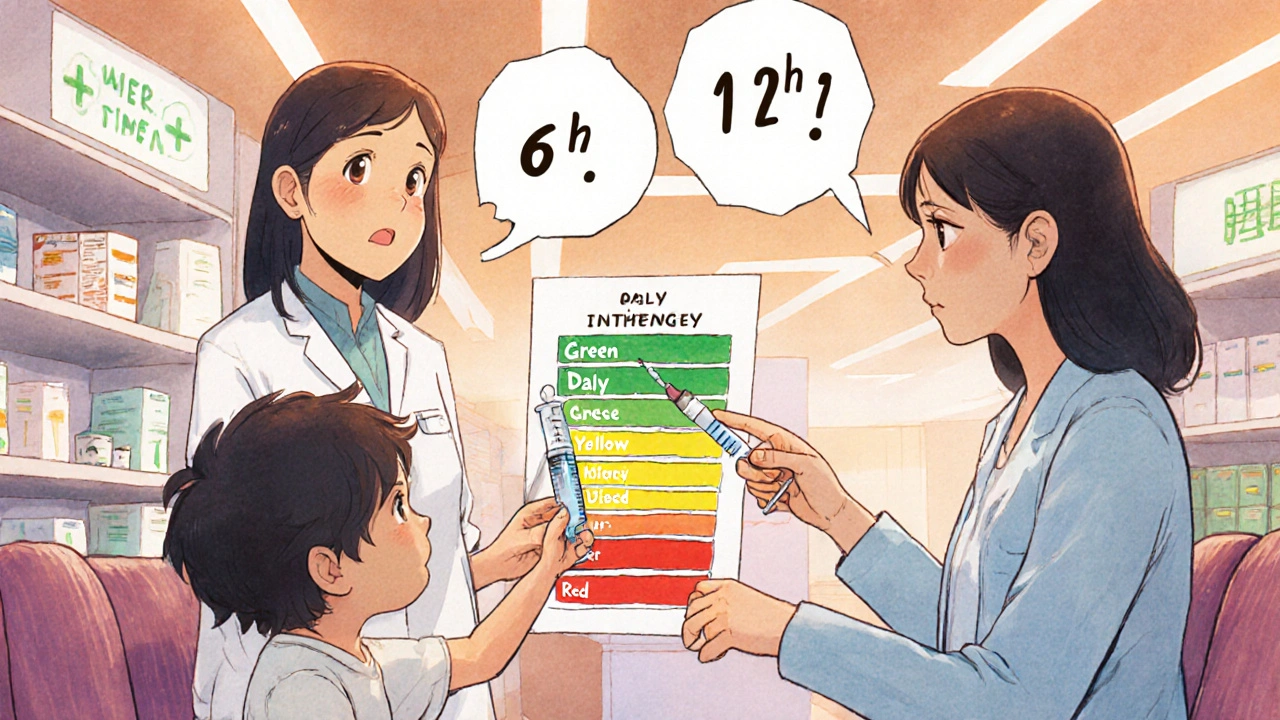
There’s no one-size-fits-all answer. What you do depends on how many times a day the medicine is supposed to be given. Here’s what major children’s hospitals recommend:
- Once daily: If you remember within 12 hours of the missed time, give it. If it’s been more than 12 hours, skip it. Wait until the next scheduled dose.
- Twice daily (every 12 hours): If you remember within 6 hours, give the missed dose. After 6 hours, skip it. Don’t wait for the next dose to be exactly 12 hours apart-just go back to the regular schedule.
- Three times daily (every 8 hours): If you remember within 3 hours, give the dose. After 3 hours, skip it.
- Four times daily (every 6 hours): If you remember within 2 hours, give it. After 2 hours, skip it.
- Every 2-4 hours (like some asthma or pain meds): If it’s been more than 2 hours since the last dose, skip the missed one. These are often high-risk medications, and giving too much too fast can be life-threatening.
These time windows aren’t arbitrary. They’re based on how long the drug stays active in the body. Giving a dose too close to the next one can cause drug levels to build up dangerously. Skipping it and returning to schedule keeps levels stable and safe.
High-Risk Medicines Need Special Care
Some medications are labeled ‘high-alert’ because even one missed or extra dose can change outcomes. These include:
- Chemotherapy drugs
- Antiseizure medications
- Insulin
- Strong painkillers like morphine or fentanyl
- Blood thinners
If you miss a dose of any of these, call your child’s doctor or pharmacist immediately. Don’t guess. For example, missing a single dose of chemotherapy can reduce treatment effectiveness by up to 30% in some cases. Your care team may adjust the next dose or schedule an early check-up. Never assume it’s fine.
And here’s something many parents don’t realize: even if the medicine bottle says nothing about missed doses, you still need a plan. A 2021 review found that 25% of high-risk pediatric medications had no missed-dose instructions in the patient leaflet. That’s a gap in the system-you have to ask.
Use Tools to Prevent Missed Doses
Prevention beats correction. Here’s how to cut down on missed doses before they happen:
- Use an oral syringe, not a spoon. Household teaspoons vary wildly in size. The FDA estimates that 22% of dosing errors come from using spoons instead of proper measuring tools. A syringe gives you exact milliliters.
- Set phone alarms. Label each alarm with the medicine name and dose. ‘Amoxicillin - 5 mL’ is better than just ‘Medicine Time.’
- Try a color-coded chart. Hospitals like Boston Children’s use color-coded daily sheets for kids on multiple meds. Green for morning, yellow for afternoon, red for night. Parents report a 44% drop in missed doses with this system.
- Use the AAP’s Pediatric Medication Safety Calculator app. It’s free. You pick the medicine, frequency, and time missed, and it tells you exactly what to do. Beta testers saw an 83% improvement in correct decisions.
For kids on four or more daily medications, the risk of error jumps 300%. That’s why simple tools matter. You’re not being lazy-you’re being smart.
Weight Matters More Than Age
Many dosing errors happen because caregivers guess a child’s weight based on age. But a 5-year-old can weigh anywhere from 35 to 60 pounds. That’s a huge difference in dose.
Studies show 74% of morphine dosing errors in emergency rooms came from using age instead of weight. The fix? Keep a recent weight on file-and use a length-based resuscitation tape (like the Broselow tape) if you’re unsure. These tapes give accurate dose estimates based on your child’s height. Hospitals use them for a reason: they reduce weight estimation errors by 42%.
If your child’s weight has changed significantly in the last few months, ask your doctor to recalculate all doses. Don’t wait for the next appointment.
Teach-Back: Make Sure You Really Understand
When your child’s doctor or nurse gives you instructions, don’t just nod and say ‘yes.’ Ask them to explain it again-and then explain it back to them in your own words.
This is called the ‘Teach-Back’ method. Cincinnati Children’s Hospital used it and cut missed-dose errors by 37%. Parents who could correctly say, ‘If I miss the 3 p.m. dose and it’s now 8 p.m., I skip it and wait until tomorrow,’ were far less likely to make mistakes later.
Don’t be shy. Say: ‘Can you check if I got this right?’ It’s not a sign you’re not smart-it’s a sign you care.
What If You’re Not Sure?
If you’re confused, don’t guess. Call someone. Here’s who to contact, in order:
- Your pediatrician’s office. Most have a nurse line open after hours.
- Your pharmacist. They’re trained in dosing and can explain what’s safe. Many offer free 24/7 advice lines.
- Telehealth services. If it’s late and your doctor’s closed, a virtual visit can give you answers in minutes.
- Emergency services only if your child shows signs of overdose: extreme drowsiness, trouble breathing, seizures, or unresponsiveness.
There’s no shame in calling. Better safe than sorry. And remember: if you’re ever unsure, skipping the dose is always safer than giving too much.

What About Liquid Medicines and Measurement Errors?
Most pediatric meds come as liquids. That’s good-easier to adjust doses. But measuring them wrong is the #1 reason for dosing errors.
Never use a kitchen spoon. Even a tablespoon can hold 15 mL-or 20 mL, depending on the spoon. Oral syringes (the kind with a plunger) are the only reliable tool. They’re cheap, often free from pharmacies, and come in 1 mL, 5 mL, and 10 mL sizes.
Also, check the concentration. Some liquid antibiotics come as 125 mg/5 mL or 250 mg/5 mL. If you give the wrong volume thinking it’s the same strength, you could under- or overdose. Always read the label and confirm with your pharmacist.
When to Worry: Signs of a Problem
If you gave an extra dose or are unsure what happened, watch for these red flags:
- Unusual sleepiness or trouble waking up
- Vomiting that won’t stop
- Fast or shallow breathing
- Seizures or twitching
- Blue lips or fingertips
- Unresponsiveness
If any of these happen, call emergency services immediately. Don’t wait. Even if you think it’s ‘probably fine,’ it’s not worth the risk.
And if your child is on a chronic condition like epilepsy or asthma, keep a log of every dose and time. That helps doctors spot patterns if things go wrong.
What if I forget my child’s medicine for a whole day?
Skip the missed day and resume the next day at the regular time. Do not give two doses the next day to make up for it. For most routine medications like antibiotics or allergy pills, one missed day won’t ruin treatment. For high-risk meds like seizure drugs or insulin, call your doctor right away.
Can I give the missed dose if it’s almost time for the next one?
No. If it’s within the time window for skipping (like 6 hours for twice-daily meds), skip it. Giving it anyway risks overlapping doses and overdose. The goal isn’t to hit exact hours-it’s to keep drug levels safe and steady.
Do I need to wake my child up to give a missed dose at night?
Only if the medicine is critical and the missed dose was recent. For most once- or twice-daily meds, if your child is asleep and it’s past the 12- or 6-hour window, don’t wake them. Let them sleep. You can give the next dose when they wake up. Interrupting sleep can do more harm than missing one dose.
My child vomited right after taking the medicine. Should I give another dose?
If your child vomited within 15-20 minutes of taking the medicine, it’s likely the dose didn’t absorb. Call your doctor or pharmacist before giving another. If it’s been more than 30 minutes, the medicine was probably absorbed, and you should not give another dose.
Are there apps that help track pediatric doses?
Yes. The American Academy of Pediatrics has a free Medication Safety Calculator app that tells you what to do if a dose is missed. Other apps like Medisafe and MyTherapy let you set reminders and track doses. Some smart pill dispensers even send alerts to your phone if a dose isn’t taken. These tools reduce missed doses by up to 68% in clinical trials.
Final Thought: You’re Doing Better Than You Think
Parenting a child on medication is hard. You’re juggling schedules, side effects, doctor visits, and fear. It’s okay to mess up. What matters is what you do next. Learn the rules, use the tools, ask questions, and don’t let guilt push you into dangerous choices. The goal isn’t perfection-it’s safety. And with the right approach, you can give your child the care they need without risking their health.




Nathan Hsu
November 13, 2025 AT 15:51Oh my god, this is so needed! I literally doubled my son's amoxicillin last week because I was panicking-he was coughing so bad, I thought I was failing as a parent. Turns out, he ended up with a rash and a 3-hour ER visit. Now I use the AAP app religiously. Also, never use a spoon. Never. I keep three oral syringes in my diaper bag. One for each time of day. Color-coded. I’m not even joking. This saved us.
Ashley Durance
November 15, 2025 AT 07:42Let’s be real-most parents don’t even know what ‘pharmacokinetics’ means. You think your kid’s 40 pounds? Maybe they’re 55. That’s a 37% overdose risk right there. And no, ‘I just eyeballed it’ is not a valid dosing strategy. The fact that 25% of high-risk meds have no instructions? That’s a systemic failure. Someone should sue the manufacturers.
Scott Saleska
November 16, 2025 AT 04:42I appreciate the guide, but I have to say-why are we making this so complicated? My kid takes four meds a day, and I just set four alarms on my phone labeled ‘AMOX,’ ‘ALBUTEROL,’ ‘INSULIN,’ and ‘SEIZURE.’ I don’t overthink it. If I miss one, I skip it. If I’m unsure, I call the pharmacist. Done. You don’t need charts or apps. Just be consistent and ask. Simple.
Ryan Anderson
November 18, 2025 AT 04:06Thank you for this. 🙏 I used to feel so guilty when I missed a dose. Like I was a bad mom. But this article? It’s like a weight lifted. I didn’t know about the time windows for different frequencies. I thought ‘twice daily’ meant exactly 12 hours apart-no wonder I was stressing. Now I use the color chart. Green = morning, yellow = afternoon, red = night. My toddler even points to the right color now. 😊
Eleanora Keene
November 19, 2025 AT 11:00As someone who works in pediatric nursing, I can’t tell you how many times I’ve seen parents double doses because they were ‘trying to stay on schedule.’ It’s heartbreaking. The Teach-Back method? It’s not just a buzzword-it’s life-saving. I make every parent repeat the instructions back to me in their own words. If they say ‘I just give it when I remember,’ I know we’ve got work to do. You’re not dumb-you’re overwhelmed. And that’s okay. Ask. Repeat. Write it down. You’ve got this.
Joe Goodrow
November 20, 2025 AT 16:05This is why America’s healthcare is broken. You need an app to know when to give your kid medicine? In my day, we just gave it when we remembered. No fuss. No charts. No ‘time windows.’ My kids grew up fine. You’re over-medicalizing parenting. Just trust your gut. And stop buying into corporate apps. Real parents don’t need smartphones to raise kids.
Don Ablett
November 21, 2025 AT 00:11The time-based guidelines presented here are empirically sound and align with the pharmacodynamic profiles of most pediatric medications. However, the absence of reference to clearance half-lives and renal maturation curves in children under two years of age represents a significant limitation in the clinical applicability of these recommendations. A more granular stratification by postnatal age and weight percentile would enhance precision.
Kevin Wagner
November 22, 2025 AT 14:15Let me tell you something-I was the guy who doubled the dose. Twice. My daughter had a fever and I was so scared I thought I was killing her by not giving more. Then I found out she had a mild allergic reaction because of it. I cried in the pharmacy aisle. But now? I’ve got a sticky note on the fridge with the AAP app QR code. I tell every new parent I meet: ‘Don’t be like me.’ You’re not weak for asking. You’re strong for learning. And yes, your kid will be fine if you skip one dose. Seriously. Breathe.
gent wood
November 24, 2025 AT 06:01Excellent, thoughtful piece. I’ve worked in a pediatric ward for 17 years, and I’ve seen too many preventable admissions due to dosing errors. The tools mentioned-oral syringes, color charts, the AAP app-are not luxuries, they’re necessities. And the Teach-Back method? That’s gold. I use it every single shift. If a parent can’t explain it back, we don’t send them home. Not because we don’t trust them, but because we love them too much to let them guess.
Dilip Patel
November 25, 2025 AT 11:25u think this is hard? try raising a kid in india with no access to oral syringes or apps. we use kitchen spoons because thats all we got. my son got sick because i gave him too much paracetamol. i didnt even know what ml meant. now i just use the cap. its close enough. dont judge us. we do our best with nothing.
Jane Johnson
November 26, 2025 AT 19:12Interesting. But why is there no mention of the FDA’s 2023 warning regarding liquid antibiotic concentration misinterpretation in households? Or the fact that 87% of caregivers cannot correctly identify the difference between mg and mL? This guide is surface-level. It avoids the real systemic issues.
Sean Hwang
November 27, 2025 AT 10:08Been there. Did that. Missed a dose of my son's seizure med. Panicked. Called the pharmacist. They said skip it. I did. He slept fine. Next day, back on schedule. No drama. Seriously, just call someone. Don't google. Don't guess. Pharmacist is your friend. And yeah, use a syringe. I bought a pack of 5 for $3 at CVS. Worth every penny.
Barry Sanders
November 29, 2025 AT 08:48Wow. Another ‘parenting fear porn’ article. You scared people into buying apps so you can sell ads. Doubling a dose? Maybe it’s not always dangerous. Maybe some kids can handle it. Not every kid is a fragile porcelain doll. You’re creating anxiety where there shouldn’t be any.
Chris Ashley
November 30, 2025 AT 07:32bro i just use my watch. if i forget, i give it when i remember. if its close to next one, i skip. done. no apps no charts. my kid is fine. stop overcomplicating life.
kshitij pandey
December 1, 2025 AT 13:58As a dad from India, I want to say this guide is a gift. In our community, many think ‘more medicine = faster cure.’ I’ve seen grandparents give 3 doses at once. This article helps me explain why that’s dangerous without sounding like I’m attacking them. I share it with my family. We now use a whiteboard with colored markers. My daughter draws a sun for morning, moon for night. Simple. Human. And it works.