Most people assume that if a drug is approved and on the shelf, it’s been thoroughly tested for safety. But here’s the truth: drug interactions - the dangerous, sometimes deadly, ways medications can clash with each other or with everyday foods - are often discovered after millions of people have already taken them.
This isn’t a flaw in the system. It’s how the system is designed to work. Clinical trials are powerful, but they’re not perfect. They involve a few thousand people over months, not millions over decades. That’s why the real test of a drug doesn’t begin until it’s in the hands of the public. And that’s when the hidden risks start to show up.
Why Clinical Trials Miss Dangerous Interactions
Clinical trials are tightly controlled. Participants are usually healthy adults, with one or two conditions, and they’re monitored closely for a short time - often less than a year. But real life doesn’t work like that.
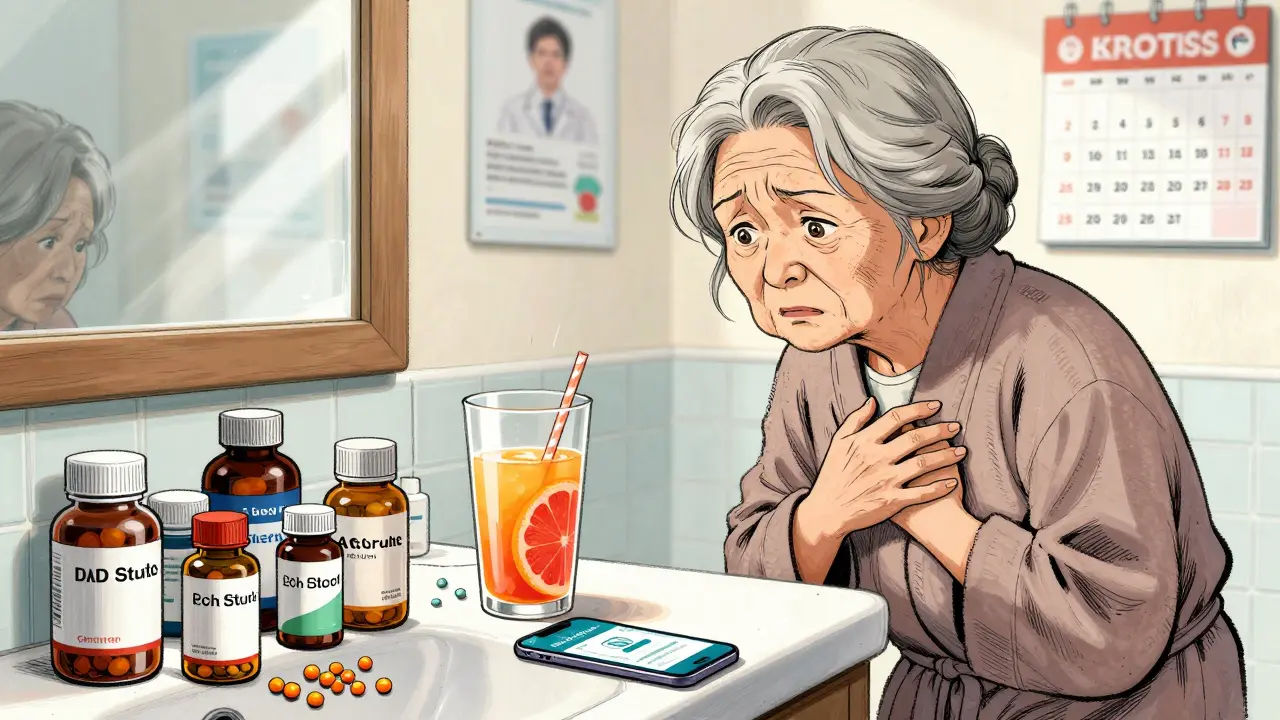
Imagine an 82-year-old woman with high blood pressure, diabetes, and arthritis. She’s on five different medications. She drinks grapefruit juice every morning. She takes St. John’s Wort for low mood. She forgets to tell her doctor about all of it. That’s the kind of person clinical trials rarely include. And yet, she’s the one most at risk.
Pre-market trials catch about half of common side effects. But serious, rare, or long-term interactions? Those often slip through. A 2020 study found that 70-80% of serious adverse drug reactions are only detected after a drug hits the market. Why? Because you need real-world exposure to see what happens when drugs mix in messy, complex human bodies over years.
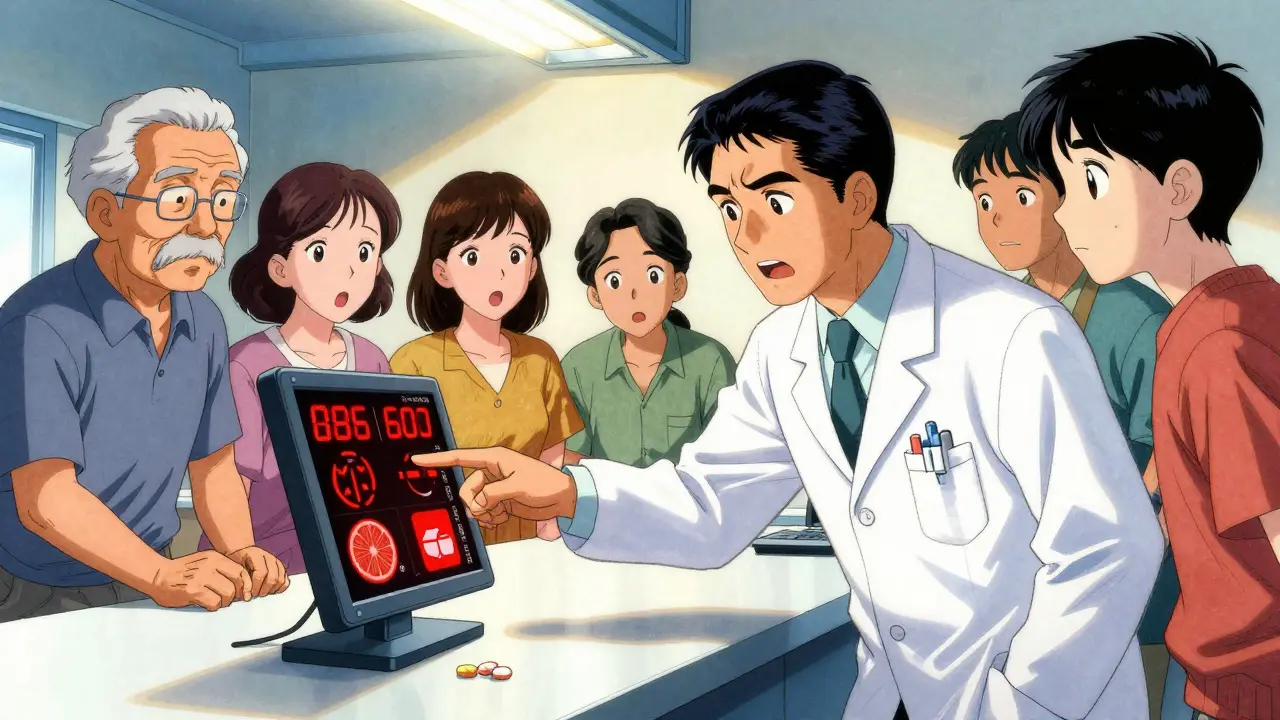
How Dangerous Interactions Get Found
Once a drug is approved, the real surveillance begins. Systems like the FDA’s FAERS (FDA Adverse Event Reporting System) and the EU’s EudraVigilance collect reports from doctors, pharmacists, and even patients. These aren’t just complaints - they’re data points.
One report of muscle pain after taking simvastatin and fluconazole? Maybe coincidence. But 500 reports? That’s a signal. That’s when regulators dig deeper. They look at patterns: Who took what? When did symptoms start? Did they get worse? Did stopping one drug help?
That’s how they found out that grapefruit juice can boost atorvastatin levels by up to 15 times - enough to cause rhabdomyolysis, a condition that destroys muscle and can wreck your kidneys. That interaction wasn’t flagged in trials. It was flagged because someone’s pharmacist noticed it. Someone’s ER doctor connected the dots. Someone reported it.
And it’s not just drugs. St. John’s Wort, a popular herbal supplement, can make blood thinners like apixaban useless - or dangerously strong. One FDA report from 2022 described a 78-year-old man who bled internally after starting St. John’s Wort while on Eliquis. His doctor never mentioned the risk. The label didn’t warn him clearly enough. He survived. Others didn’t.
Real Cases That Changed Medicine
Some discoveries forced drugs off the market entirely.
Terfenadine (Seldane), a once-popular allergy pill, was pulled in 1998 after it was found to cause fatal heart rhythms when taken with ketoconazole (an antifungal) or grapefruit juice. The interaction was rare - but deadly. One in 10,000 users could die. That’s not acceptable.
Benfluorex (Mediator), a weight-loss drug sold in France for 30 years, was withdrawn in 2009 after it was linked to heart valve damage in over 5 million patients. No one saw it in trials. It only showed up after decades of use.
And then there’s Exalgo, a long-acting painkiller. After 18 months on the market, reports poured in: people were overdosing after drinking alcohol. The drug was designed to release slowly - but alcohol caused it to dump all its dose at once. That’s a hidden interaction. One that killed people before anyone realized it was possible.
What You Can Do to Stay Safe
You can’t rely on your doctor to know every interaction. They’re human. They’re busy. New drugs come out all the time. Even top specialists miss things.
Here’s what you can do:
- Keep a full list of everything you take. That includes prescriptions, over-the-counter meds, vitamins, herbs, and supplements. Don’t forget your daily aspirin or your turmeric capsules.
- Ask your pharmacist every time. Pharmacists are trained to catch interactions. They see hundreds of prescriptions a day. They know what combos are risky. Don’t just pick up your script - ask, “Could this interact with anything else I’m taking?”
- Use trusted tools. Apps like GoodRx and Medscape have interaction checkers that flag dangers in seconds. One user on Reddit said, “The warning stopped me from taking ciprofloxacin with my blood pressure pill. My pharmacist said it could have caused a dangerous heart rhythm.” That’s the power of a quick check.
- Know your red flags. Unexplained muscle pain, extreme fatigue, dizziness, irregular heartbeat, or sudden bleeding? If you started a new drug or changed your routine, consider an interaction. Don’t wait. Call your doctor.
The System Is Improving - But It’s Not Perfect
There’s good news. The tools are getting smarter.
The FDA’s Sentinel Initiative now tracks over 300 million patient records across hospitals and insurers. AI systems can scan millions of reports and spot patterns humans miss. In 2023, the FDA approved its first AI-powered pharmacovigilance tool that can process 10,000 reports a day with 92.7% accuracy. The EU cut detection time for dangerous signals from 18 months to just 45 days.
But here’s the catch: underreporting is still massive. Experts estimate that 90-95% of adverse events never get reported. Why? People don’t know what to report. Doctors are overwhelmed. Patients think it’s “just a side effect.”
And labeling? Still messy. Many drug inserts don’t clearly warn about interactions. A 2021 Duke University study found that even when interactions are known, the information is buried in tiny print or left out entirely.
That’s why your role matters. You’re not just a patient. You’re a safety net.
The Bigger Picture: Why This Costs Billions - and Lives
Adverse drug events cost the U.S. healthcare system over $1 billion a year - and drug interactions make up about a third of that. That’s not just money. It’s hospital stays. Emergency rooms. Lost work. Families shattered.
Pharmaceutical companies now spend billions on post-market safety. The global pharmacovigilance market grew from $5.8 billion in 2020 to $7.3 billion in 2022. Big firms hire specialists. They run long-term studies. They update labels. But it’s still reactive. We’re still catching problems after people get hurt.
Future tools - like genetic testing for drug metabolism - could change that. The NIH’s Pharmacogenomics Research Network is already studying how your DNA affects how you process medications. In five years, your doctor might test your genes before prescribing statins or blood thinners. That could prevent most interactions before they start.
But until then? The safest thing you can do is stay informed. Stay vigilant. Speak up.
Medications save lives. But they can also harm - especially when we don’t know how they’ll behave in the real world. The system works better than it used to. But it still needs you to be part of the solution.
How common are drug interactions discovered after a drug is on the market?
About one in three new drugs approved by the FDA between 2001 and 2010 had a major safety event - like a black box warning, recall, or safety alert - after approval, according to FDA data. Around 20% of new drugs received a black box warning only after being used by millions of patients. These are not rare exceptions. They’re a normal part of how drugs are monitored.
Can over-the-counter drugs and supplements cause dangerous interactions?
Absolutely. St. John’s Wort, garlic supplements, and even high-dose vitamin E can interfere with blood thinners, antidepressants, and cancer drugs. Grapefruit juice is one of the most dangerous - it can boost levels of statins, blood pressure meds, and immunosuppressants by up to 15 times. Just because something is sold without a prescription doesn’t mean it’s safe with your other meds.
Why don’t drug labels warn about all known interactions?
Labeling is often delayed, incomplete, or buried in technical language. Regulatory agencies prioritize the most serious risks first. Smaller interactions, or those affecting rare populations, may not be included until more evidence is gathered. Also, drug companies sometimes delay updates due to legal concerns. That’s why you can’t rely on the label alone - always check with a pharmacist.
What should I do if I think I’m having a drug interaction?
Stop taking the medication if you’re having severe symptoms like chest pain, difficulty breathing, uncontrolled bleeding, or sudden muscle weakness. Call your doctor or go to the ER. Then report the event to your country’s adverse event reporting system - in the U.S., that’s the FDA’s MedWatch program. Your report helps protect others.
Are newer drugs safer than older ones when it comes to interactions?
Not necessarily. Newer drugs are tested on smaller, more homogenous groups, so they may miss interactions that only appear in older patients or those on multiple medications. Older drugs have been studied longer, so many of their risks are well-documented. But both can be dangerous if used incorrectly. Age doesn’t guarantee safety - awareness does.
What Comes Next
The future of drug safety is in data - not just from clinical trials, but from real people. AI, genetic testing, and global reporting networks are making it easier to spot dangers faster. But until those systems are universal and foolproof, your actions matter most.
Keep your medication list updated. Ask questions. Use free tools. Report suspicious side effects. You’re not just protecting yourself - you’re helping to make the system better for everyone else.





Payson Mattes
December 25, 2025 AT 04:06So let me get this straight - the FDA lets Big Pharma dump drugs on us like candy, then acts shocked when people start dropping dead? 🤡 I’ve seen it with my own eyes. My uncle took that one blood pressure med and ended up in the ICU because the label didn’t say grapefruit juice would turn his heart into a ticking bomb. They knew. They ALWAYS knew. They just don’t care until the lawsuits start rolling in. And don’t even get me started on the AI ‘solutions’ - that’s just more data mining to sell you more pills. Wake up people.
Steven Mayer
December 26, 2025 AT 14:00The pharmacovigilance infrastructure remains fundamentally reactive due to the epistemological constraints of post-marketing surveillance systems. Adverse event reporting is subject to significant underreporting bias, with non-random sampling distributions skewing signal detection. The FAERS database, while voluminous, lacks granular temporal and comorbidity stratification, rendering causal inference statistically untenable without probabilistic modeling. Consequently, the current paradigm is structurally incapable of preemptive risk mitigation.
Charles Barry
December 28, 2025 AT 06:36Oh please. You think this is about safety? This is about PROFITS. The FDA is a revolving door for Big Pharma execs. Every single ‘new discovery’ of an interaction? Came AFTER the drug made billions. They don’t test properly because they don’t WANT to - if they did, half the drugs on the shelf would vanish. And now they’re pushing ‘AI tools’ like it’s magic? Ha! That’s just a PR stunt to make you feel safe while they keep selling poison wrapped in a white coat. I’ve seen the internal emails. They laugh about it.
Rosemary O'Shea
December 29, 2025 AT 07:33How utterly pedestrian. You reduce the entire pharmacovigilance ecosystem to a morality play when it’s clearly a complex, multi-layered system of risk-benefit calculus. The notion that patients are ‘safety nets’ is not just romanticized - it’s dangerously simplistic. We’re talking about a global network of regulatory bodies, real-world evidence platforms, and pharmacogenomic databases that have evolved over decades. To reduce this to ‘ask your pharmacist’ is the intellectual equivalent of blaming the victim for not checking the weather before stepping into a hurricane.
Bartholomew Henry Allen
December 31, 2025 AT 02:16Government is broken. Drugs are dangerous. You think they care about you? They care about lawsuits and stock prices. I’ve been in the system. They bury the bad data. They delay warnings. You want safety? Stop taking everything. Take nothing. That’s the only real protection. No more pills. No more supplements. No more ‘natural remedies’. Just survive. That’s the only real advice.
Jeffrey Frye
January 1, 2026 AT 21:44so like… i took that st johns wort thing for like 3 months and my blood thinners got all weird and i started bleeding out my nose for no reason. i thought it was just dry air. then my pharmacist was like ‘uhhh you know that stuff cancels out your med right?’ and i was like… wait what? the label didnt say that. and now im scared to take anything. like… how many other things are out there that i dont know about? i feel like my body is a minefield.
Raja P
January 3, 2026 AT 01:37I really appreciate this post. In India, many people take Ayurvedic herbs with their prescriptions without knowing the risks. My aunt took ashwagandha with her thyroid med and ended up in the hospital. We didn’t know it could interact. I’ve started sharing this info with my family now - even just writing down everything on a piece of paper and showing it to the pharmacist makes a huge difference. Small steps, but they matter.
Joseph Manuel
January 3, 2026 AT 04:47While the anecdotal evidence presented is compelling, the generalization of systemic failure is unwarranted. The post-market surveillance framework operates under strict statutory guidelines and has demonstrably improved outcomes since the 1990s. The FDA’s Sentinel Initiative, for instance, has reduced the time-to-detection for Class I recalls by 40%. To imply that all regulatory bodies are negligent is both inaccurate and counterproductive to public trust in evidence-based medicine.
Harsh Khandelwal
January 3, 2026 AT 16:13lol so the ‘system’ is just a giant game of russian roulette with your meds? no wonder my grandma’s fridge is full of pills and her brain is fried. they don’t test for old people? or people who actually live? i mean, i get it - the trials are for ‘healthy adults’ - but who the hell is that? i’m 68 and i take 7 things and drink grapefruit juice like it’s water. if i die, at least i died with flavor. but seriously, why does the label say ‘may interact’ like it’s a weather warning? it should say ‘this combo will turn you into a human meatloaf’.
Andy Grace
January 5, 2026 AT 02:38I’ve been a pharmacist for 22 years. I’ve seen people die from interactions that were never flagged in trials. I’ve also seen people live because they asked me about their supplements. It’s not perfect. But if you take the time to write down every pill, every herb, every tea - and bring it to the pharmacy - you’re already ahead of 90% of people. Don’t wait for the system to save you. Just be the person who asks.