When you're on warfarin, even a simple antibiotic can throw your blood clotting off balance-sometimes dangerously so. It’s not just about taking pills. It’s about how those pills talk to each other inside your body. Warfarin is a powerful drug. It keeps your blood from clotting too much, which helps prevent strokes, heart attacks, and dangerous clots in your legs or lungs. But it doesn’t take much to push it too far. And one of the most common triggers? Antibiotics.
Why Warfarin Is So Sensitive
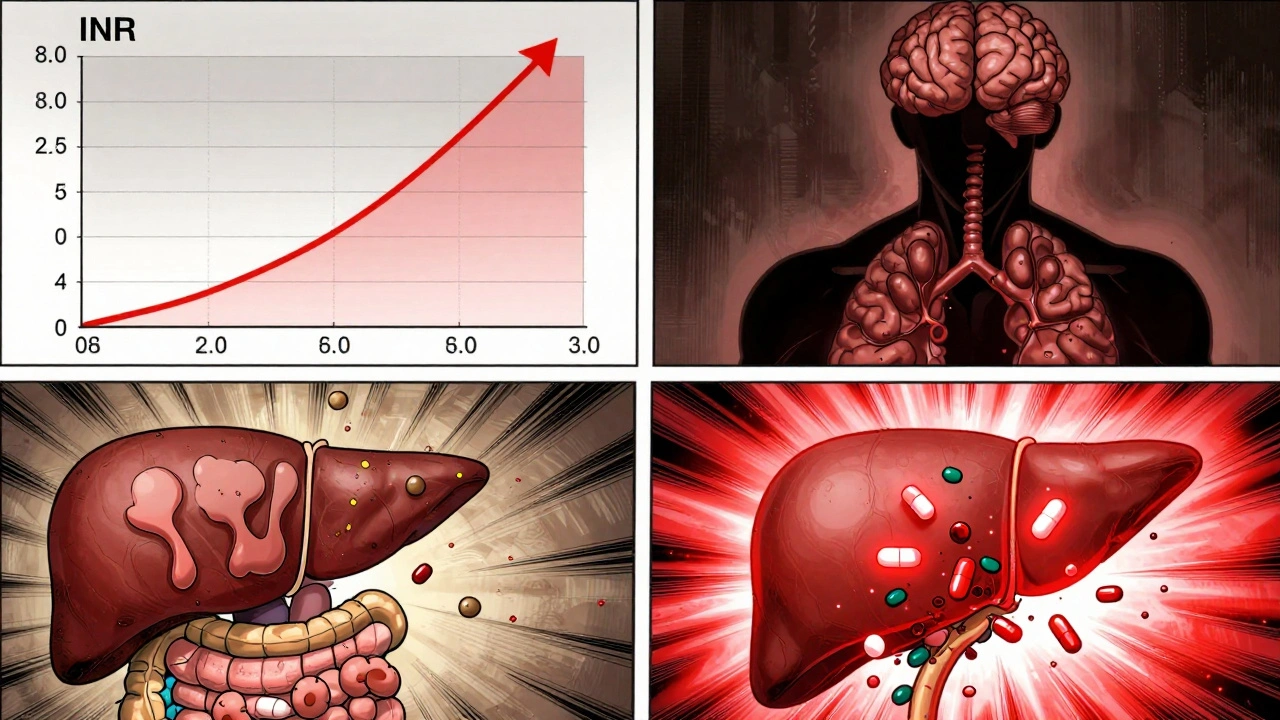
Warfarin works by blocking vitamin K, which your body needs to make clotting factors. Too little vitamin K? Your blood thins out. Too much? You risk clots. The sweet spot is an INR between 2.0 and 3.0. That’s the number doctors use to measure how long it takes your blood to clot. If your INR hits 5.0 or higher, your bleeding risk jumps sharply. And antibiotics? They can push your INR into that danger zone.
Here’s the catch: warfarin is metabolized by enzymes in your liver-mainly CYP2C9. Many antibiotics interfere with these enzymes. When they do, warfarin sticks around longer in your bloodstream. That means more anticoagulant effect, even if you haven’t changed your dose. On top of that, antibiotics kill off the good bacteria in your gut. Those bacteria make about 10-15% of your daily vitamin K. No bacteria? Less vitamin K. That makes warfarin even more effective. Two mechanisms. One outcome: a rising INR.
Not All Antibiotics Are the Same
Some antibiotics barely touch your INR. Others? They’re like a lit match near gasoline.
- High-risk antibiotics: Fluoroquinolones (ciprofloxacin, levofloxacin), macrolides (clarithromycin), sulfonamides (trimethoprim-sulfamethoxazole), and metronidazole. These can raise your INR by 1.5 to 3 points in just a few days. In some cases, INR spikes from 2.5 to over 8.0.
- Low-risk antibiotics: Penicillins (like amoxicillin) and most cephalosporins (like ceftriaxone). These usually cause little to no change-less than 0.5 INR point in most people.
- Special case: Azithromycin: Unlike other macrolides, it doesn’t block liver enzymes. It’s often the go-to alternative when you need an antibiotic but are on warfarin.
A 2014 study in JAMA Internal Medicine found that people on warfarin who took high-risk antibiotics were more than twice as likely to have an INR above 5.0 compared to those who didn’t take antibiotics. And that’s not just a number. That’s a real risk of bleeding inside your brain, gut, or joints.
When Does the INR Start to Rise?
It’s not immediate. You might take an antibiotic on Monday and feel fine. Then on Thursday, you notice a bruise you didn’t get. By Saturday, your INR is 6.2. That delay trips up even experienced patients and doctors.
The reason? Gut bacteria take time to die off. Vitamin K production drops slowly. That’s why the INR spike often peaks between days 5 and 10. But here’s the twist: when you stop the antibiotic, your INR can crash just as fast. The bacteria bounce back. Vitamin K comes back online. Warfarin suddenly isn’t as strong. Your INR might drop from 2.8 to 1.1 in a few days. That’s not just risky-it’s dangerous. You could develop a clot or even have a stroke.
Who’s Most at Risk?
It’s not just about the antibiotic. Your personal risk matters too.
- Age over 75: Your liver slows down. Warfarin clears slower. Even small changes can be dangerous.
- Cancer patients: Cancer itself affects clotting. Add antibiotics? INR instability skyrockets.
- Women: Studies show women on warfarin are 40% more likely to have a dangerous INR spike with antibiotics than men.
- Baseline INR above 2.5: If you’re already near the top of your therapeutic range, even a small nudge can push you over the edge.
One study found that 68% of doctors had seen at least one major bleeding event linked to warfarin-antibiotic interactions in the past year. Many of those cases were preventable.
What You Should Do
If you’re on warfarin and your doctor prescribes an antibiotic, here’s what you need to do-right away.
- Ask: Is this antibiotic necessary? Many sinus infections and bronchitis cases are viral. Antibiotics won’t help-and they could hurt you.
- Ask: Which antibiotic are you prescribing? If it’s ciprofloxacin, levofloxacin, clarithromycin, or trimethoprim-sulfamethoxazole, push back. Ask if azithromycin or amoxicillin could work instead.
- Get an INR test before you start. Know your baseline.
- Get another INR test 3 to 5 days after starting the antibiotic. Don’t wait for symptoms. Don’t wait for your next scheduled check-up.
- Get another test 7 to 10 days after stopping the antibiotic. Your INR can drop fast once the drug is gone.
Some patients now use home INR monitors-devices like the Roche CoaguChek INRange-that connect to your phone. These let you test daily during antibiotic therapy. That’s a game-changer. One 2022 trial showed that patients using home testing had 37% fewer INR swings during antibiotic use.

What Happens If Your INR Gets Too High?
If your INR is above 5.0, your doctor will likely:
- Hold your next warfarin dose
- Give you vitamin K (by mouth or IV) to reverse the effect
- Monitor you closely-sometimes in the hospital
Don’t try to fix it yourself. Taking extra vitamin K without medical supervision can make your INR crash later. And if your INR is above 10, you might need fresh frozen plasma to stop bleeding immediately.
Why This Still Matters in 2025
You might think warfarin is outdated. After all, newer drugs like apixaban and rivaroxaban don’t need INR checks. But here’s the truth: 3.2 million Americans still take warfarin. In Medicare populations, it’s the most common anticoagulant because it costs about $4 a month-versus over $500 for the newer drugs.
That’s why this interaction isn’t going away. And it’s why so many people still end up in the ER because of it. A 2021 study found that nearly 24% of warfarin-related emergency visits involved recent antibiotic use. More than half of those patients had an INR over 5.0.
Technology is helping. AI systems can now predict how your INR will react to specific antibiotics based on your genetics, age, and history. But none of that matters if you don’t get tested.
Bottom Line
Warfarin and antibiotics don’t mix safely unless you’re watching your INR like a hawk. It’s not about avoiding antibiotics-it’s about choosing the right one and checking your blood at the right times. If you’re on warfarin, treat every antibiotic as a potential red flag. Ask questions. Get tested. Don’t assume it’s safe just because your doctor didn’t warn you. Too many people have learned the hard way that a simple infection treatment can turn into a life-threatening bleed.
Can I take amoxicillin while on warfarin?
Yes, amoxicillin is generally safe with warfarin. Most studies show it causes little to no change in INR-usually less than 0.5 points. But even with low-risk antibiotics, it’s still wise to check your INR 3 to 5 days after starting the antibiotic, especially if you’re older, have cancer, or your INR is already near the top of your target range.
Why does clarithromycin raise INR so much?
Clarithromycin strongly inhibits the CYP3A4 liver enzyme, which helps break down warfarin. This causes warfarin to build up in your blood. At the same time, it kills gut bacteria that make vitamin K. This dual effect can push INR up by 2 to 3 points within a week. That’s why many doctors avoid clarithromycin in patients on warfarin and choose azithromycin instead.
What should I do if I forget to check my INR after starting an antibiotic?
Check it as soon as possible-even if you feel fine. A rising INR doesn’t always cause symptoms until it’s too late. Bruising, nosebleeds, dark stools, or headaches could be signs of internal bleeding. If you can’t get to a lab, use a home monitor if you have one. If you don’t have access to testing, contact your doctor immediately. Don’t wait for symptoms.
Can I take over-the-counter antibiotics with warfarin?
There are no true over-the-counter antibiotics in the U.S. and Australia. But some people use herbal supplements like garlic, ginger, or turmeric thinking they’re harmless. These can also thin the blood and raise INR. Always tell your doctor about every supplement you take-even if you think it’s natural. Many interactions happen because patients don’t mention what they’re taking.
How long should I wait to restart warfarin after stopping a high-risk antibiotic?
Don’t restart warfarin on your own. Your INR will likely drop after stopping the antibiotic because your gut bacteria recover and start making vitamin K again. You might need to restart at a lower dose than before. Always get your INR tested 7 to 10 days after stopping the antibiotic, then adjust your warfarin dose under your doctor’s guidance. Restarting too soon or at your old dose can lead to dangerous over-anticoagulation.
Antibiotics save lives. But when you’re on warfarin, they can also put you in the hospital. The key isn’t fear-it’s awareness. Know which ones are risky. Know when to test. And never assume your doctor has already thought of it. You’re the most important part of your own care.




Shannara Jenkins
December 2, 2025 AT 09:51Just had to comment because my dad almost bled out last year from this exact thing. Doc prescribed cipro for a UTI, didn’t tell him to check INR. He got home, started bruising like a cartoon. We rushed him in-INR was 8.4. Now he uses a home monitor and only takes azithromycin. Life-saving info, honestly.
Arun kumar
December 3, 2025 AT 16:12bro i was on warfarin for afib and took cefdinir for a cold… thought it was safe… turned out my INR went from 2.3 to 4.1 in 4 days. no symptoms till i spat blood in the sink one morning. 911 ride. now i ask every doc: ‘is this one of the bad ones?’
Zed theMartian
December 5, 2025 AT 01:36Oh wow. A whole article about something that’s been in every pharmacology textbook since 1998. Truly groundbreaking. I’m sure the 3.2 million warfarin users were just sitting around waiting for a Reddit post to tell them antibiotics interact with their meds. How quaint. The real tragedy? People still don’t read their discharge papers.
Ella van Rij
December 6, 2025 AT 08:50So… you’re telling me that if I take antibiotics, I might need to… *checks blood*? Like… a human? Wow. That’s wild. I always thought doctors just waved a magic wand and everything stayed balanced. My bad for assuming medicine was science and not guesswork.
ATUL BHARDWAJ
December 6, 2025 AT 09:43In India, many take amoxicillin without testing. Many survive. But also many die. Simple truth. Check INR. Not hard. Not expensive. Just care.
Rebecca M.
December 7, 2025 AT 12:55Oh sweet mercy. Another ‘your doctor didn’t warn you’ guilt trip. Maybe if your doctor had time to explain every single interaction between every drug you’ve ever taken, you wouldn’t need to read 2000-word Reddit essays to survive. But no. Let’s just make everyone feel dumb for not being pharmacists.
Paul Keller
December 7, 2025 AT 20:38As someone who’s been on warfarin for 12 years and has managed over 15 antibiotic courses, I can say this: the key isn’t fear-it’s consistency. I test before, during, and after every antibiotic. I log everything in a spreadsheet. I track my vitamin K intake (yes, kale matters). I’ve never had an INR above 5.0. It’s not magic. It’s discipline. And if you think this is too much work, ask yourself: how much is your life worth? The newer anticoagulants? Great. But if you’re on warfarin because you can’t afford $500/month, you owe it to yourself to be proactive. Don’t wait for the ER to teach you.
Elizabeth Grace
December 8, 2025 AT 11:09I cried reading this. My mom passed last year from a brain bleed after taking Bactrim. She didn’t know. The doctor didn’t say. I’ve been blaming myself ever since. Thank you for writing this. I’m sharing it with everyone I know on warfarin. You saved lives today.
Steve Enck
December 10, 2025 AT 01:43The fundamental flaw in this narrative is the assumption that patient agency is the primary vector of safety in anticoagulant management. This is a systemic failure of clinical governance, not individual negligence. The onus should not rest on patients to become pharmacokinetic analysts. The medical infrastructure must embed real-time CYP450 and microbiome interaction alerts into EHRs. Until then, we are merely rearranging deck chairs on the Titanic while prescribing INR checks as palliative care.
Jay Everett
December 11, 2025 AT 16:14Big shoutout to the guy who mentioned home INR monitors! 🙌 I got my CoaguChek last year and it changed everything. Now I test every other day when I’m on antibiotics. I even made a little chart on my fridge: ‘Cipro? 🚫 Test Day 3. Azithro? 👍 Still test, but chill.’ My wife says I’m obsessed. I say I’m alive. And hey-if you’re on warfarin and don’t have a home monitor, ask your doc about Medicare coverage. It’s often covered. You’re worth the hassle. 💪🩸
मनोज कुमार
December 12, 2025 AT 01:36Warfarin interactions are well known. Why are you still using it? Switch to DOACs. No INR. No hassle. If you cant afford it, your healthcare system is broken. Not your fault. But your choice to stay on warfarin is. Stop pretending this is a patient education problem. Its a policy failure.