What Really Causes Type 2 Diabetes?
Most people think type 2 diabetes is just about eating too much sugar. But that’s not the full story. The real problem starts long before blood sugar climbs into the diabetic range. It begins with something called insulin resistance - a silent, slow-burning fire inside your cells that no one talks about until it’s too late.
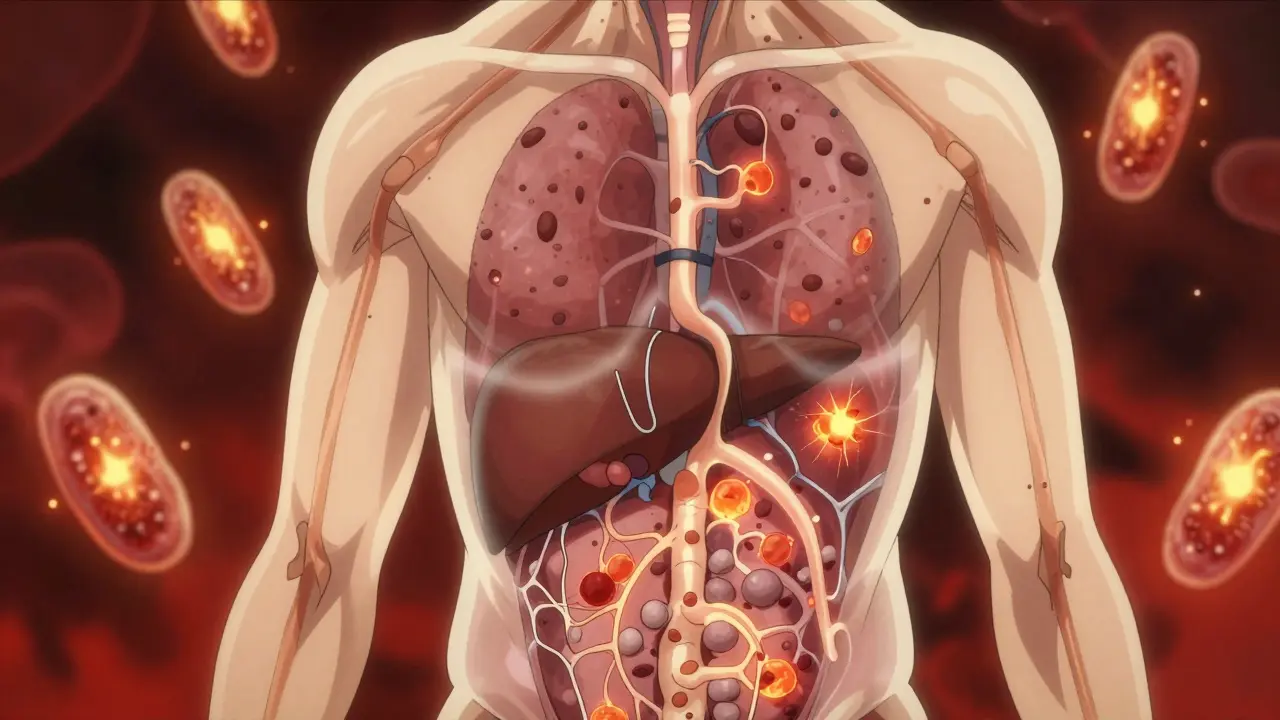
Insulin is the hormone your pancreas makes to tell your muscle, fat, and liver cells: "Take in glucose from the blood." When those cells stop listening - when they become resistant - your pancreas has to pump out more and more insulin just to keep things under control. This goes on for years. You feel fine. Your blood tests look normal. But behind the scenes, your body is working overtime, and your cells are drowning in fat and inflammation.
How Insulin Resistance Turns Into Diabetes
Insulin resistance doesn’t just make your blood sugar rise. It rewires your whole metabolism. High glucose and fatty acids from overeating start blocking the insulin signaling pathway - the same way a clogged pipe stops water from flowing. Your liver stops responding to insulin’s signal to stop making glucose. Your muscles stop taking in sugar. Your fat cells start leaking fatty acids into your bloodstream. All of this adds up to one thing: glucose piles up in your blood.
At first, your pancreas compensates. It churns out extra insulin. But beta cells - the insulin-producing factories in your pancreas - aren’t designed for this kind of long-term stress. Over time, they burn out. Studies show beta cell function declines by 4-5% per year in people with insulin resistance. By the time your fasting blood sugar hits 126 mg/dL (7.0 mmol/L), you’ve already lost 50-70% of your beta cell capacity. That’s why type 2 diabetes is irreversible for most people - not because of bad choices, but because the body’s backup system failed.
What Is Metabolic Syndrome? (And Why It Matters)
Metabolic syndrome isn’t a single disease. It’s a cluster of warning signs that your metabolism is falling apart. The International Diabetes Federation says you have it if you have at least three of these five things:
- Waist size over 94 cm for men (European), 90 cm for South Asian and East Asian men, or 80 cm for women of any background
- Triglycerides above 150 mg/dL
- HDL (good cholesterol) below 40 mg/dL for men or 50 mg/dL for women
- Blood pressure at or above 130/85 mmHg
- Fasting blood sugar of 100 mg/dL or higher
Here’s the kicker: you don’t need to be overweight to have metabolic syndrome. About 30-40% of people with normal weight still have it - especially if their fat is stored deep inside their belly or liver. That’s the dangerous kind. Fat around your organs releases inflammatory chemicals that make insulin resistance worse. This is why two people with the same weight can have wildly different metabolic health.
And here’s what most doctors still don’t tell you: the term "metabolic syndrome" is outdated. Leading researchers now call it metabolic dysfunction syndrome - because it’s not just a list of symptoms. It’s an active disease process. Your body isn’t just out of balance - it’s breaking down.
Why This Isn’t Just About Weight
People assume if you’re thin, you’re safe. But that’s not true. A lean South Asian person with a waist of 85 cm and fatty liver has a higher risk of type 2 diabetes than a heavier person with fat stored under the skin. Genetics play a big role. Some people’s bodies store fat safely. Others store it in the liver, pancreas, and muscles - where it causes damage.
Studies show that people with nonalcoholic fatty liver disease (NAFLD) have more than double the risk of developing type 2 diabetes. If they have the more severe form, NASH, their risk triples. That’s because fat in the liver directly interferes with insulin signaling. Your liver starts making too much glucose, even when you haven’t eaten. That’s why some people wake up with high blood sugar - not because they ate sugar the night before, but because their liver is stuck in overdrive.
And here’s another surprise: not everyone with insulin resistance develops diabetes. Some people have severe resistance but their beta cells keep up. Others have mild resistance but their beta cells fail early. That’s why doctors are starting to see type 2 diabetes as multiple diseases - not one.
The Real Link Between Insulin Resistance and Heart Disease
Metabolic syndrome doesn’t just lead to diabetes. It leads to heart attacks, strokes, and kidney failure. Why? Because insulin resistance isn’t just about sugar. It messes with your blood vessels, your clotting system, and your inflammation levels.
High insulin levels cause your arteries to stiffen. They make your blood more likely to clot. They raise your blood pressure. They lower your good cholesterol and raise your bad cholesterol. The Mayo Clinic says having metabolic syndrome increases your risk of heart disease by 200-300%. That’s worse than smoking. Worse than high cholesterol alone.
And here’s the truth: most people with metabolic syndrome don’t know they’re at risk. Their cholesterol is "borderline." Their blood pressure is "a little high." Their fasting sugar is "just above normal." They’re told to "watch their diet" - but no one tells them this is the beginning of something serious.
Can You Reverse It?
Yes - but only if you act early. The Diabetes Prevention Program proved that losing 7% of your body weight and doing 150 minutes of walking per week cuts your risk of developing type 2 diabetes by 58%. That’s more effective than any drug.
Metformin, the first-line medication for prediabetes, reduces risk by 31%. But it doesn’t fix the root cause. Lifestyle changes do. The Look AHEAD trial showed that people who lost 10% of their body weight had a 51% chance of reversing prediabetes in one year. Twelve percent were still in remission after eight years.
What works? Not low-fat diets. Not calorie counting. Real change comes from:
- Reducing ultra-processed carbs and added sugars
- Eating more protein and healthy fats to stabilize blood sugar
- Walking 10,000 steps a day - not just gym sessions
- Getting 7-8 hours of sleep - poor sleep increases insulin resistance
- Managing stress - cortisol raises blood sugar
And if you’ve already been diagnosed with type 2 diabetes? New drugs like semaglutide and tirzepatide can help you lose up to 15% of your body weight and put diabetes into remission in two-thirds of cases. But they’re not magic pills. They work best when paired with real lifestyle changes.

What You Should Do Right Now
If you’ve been told you have prediabetes, metabolic syndrome, or insulin resistance - don’t wait. Don’t think, "I’ll start next month." This isn’t a future problem. It’s happening now.
Here’s what to do:
- Get your waist measured. If it’s over the thresholds above, you’re at risk - even if your weight is normal.
- Ask for an HbA1c test. If it’s above 5.7%, you’re in the danger zone.
- Get a liver ultrasound if you’re overweight or have high triglycerides. Fatty liver is a red flag.
- Start walking 30 minutes a day, five days a week. No gym needed.
- Swap sugary drinks for water. Cut out candy, pastries, and white bread.
- Ask your doctor about metformin if you’re at high risk. It’s cheap, safe, and proven.
You don’t need to be perfect. You just need to start. Every day you delay, your beta cells lose more function. Every day you move, your cells become more sensitive to insulin.
Why This Matters More Than Ever
By 2050, one in three Americans will have diabetes. Globally, 537 million adults already do. The cost? Over $327 billion in the U.S. alone. But here’s the hopeful part: research shows that coordinated public health efforts - better food policies, urban design that encourages walking, access to affordable healthy food - could reduce type 2 diabetes by 40-60% by 2035.
This isn’t just about individual choices. It’s about systems. But it starts with you. If you understand insulin resistance, you’re no longer just a patient. You’re someone who can stop the cycle - for yourself, and maybe for others too.
Is insulin resistance the same as type 2 diabetes?
No. Insulin resistance is the underlying cause of most type 2 diabetes cases, but it’s not the same thing. You can have insulin resistance for years without having diabetes. It’s when your pancreas can no longer produce enough insulin to overcome the resistance that blood sugar rises into the diabetic range. Think of it like this: insulin resistance is the engine problem. Type 2 diabetes is the car breaking down.
Can you have metabolic syndrome without being overweight?
Yes. About 30-40% of people with metabolic syndrome have a normal BMI. What matters more is where your fat is stored. If you carry fat around your belly or inside your liver, you’re at high risk - even if you’re "skinny." Genetics play a big role here, especially in South Asian and East Asian populations.
Does metformin cure insulin resistance?
No. Metformin helps your body use insulin better and lowers blood sugar, but it doesn’t fix the root cause. It’s a tool - not a cure. The only proven way to reverse insulin resistance is through sustained weight loss, movement, and reducing processed carbs. Metformin supports those efforts, especially in high-risk people.
How long does it take to reverse insulin resistance?
Some people see improvements in insulin sensitivity within 2-4 weeks of cutting sugar and starting daily walks. But lasting change takes time. The Diabetes Prevention Program showed that people who maintained 7% weight loss for three years cut their diabetes risk by over half. Reversal isn’t a sprint - it’s a lifestyle shift.
Are GLP-1 drugs like Ozempic the future of diabetes treatment?
They’re a major breakthrough. Drugs like semaglutide and tirzepatide help people lose weight, lower blood sugar, and even reverse type 2 diabetes in many cases. But they’re expensive, not available to everyone, and don’t work if you go back to old habits. They’re powerful tools - but lifestyle changes remain the foundation of long-term health.
What Comes Next?
If you’re reading this and thinking, "I’ve got some of these signs," you’re not alone. Millions are in the same place - unaware, overwhelmed, or told it’s "just a little high." But now you know: insulin resistance isn’t a minor glitch. It’s the silent engine of a global health crisis.
You don’t need to fix everything at once. Start with one thing: measure your waist. Walk for 20 minutes today. Swap your morning juice for water and eggs. That’s enough to start turning things around.
The science is clear. The tools exist. The time to act is now - before your pancreas gives up, before your liver fills with fat, before your heart pays the price.




Sazzy De
January 31, 2026 AT 06:40Start small. Keep going.
Adarsh Uttral
February 1, 2026 AT 02:05Gaurav Meena
February 2, 2026 AT 18:30Carolyn Whitehead
February 3, 2026 AT 16:41Jodi Olson
February 4, 2026 AT 10:25Kathleen Riley
February 4, 2026 AT 23:39Amy Insalaco
February 6, 2026 AT 12:36kate jones
February 8, 2026 AT 06:56April Allen
February 9, 2026 AT 12:40Sheila Garfield
February 10, 2026 AT 23:22Shawn Peck
February 12, 2026 AT 16:22Yanaton Whittaker
February 14, 2026 AT 09:54Eliana Botelho
February 15, 2026 AT 16:38Katie and Nathan Milburn
February 15, 2026 AT 20:33