It’s easy to assume that memory lapses, confusion, or sluggishness in an older adult are just part of getting older. But what if those signs aren’t aging at all? What if they’re caused by a pill someone is taking every day? Across Australia and beyond, thousands of seniors are being misdiagnosed with dementia or cognitive decline when the real culprit is a common medication. These side effects don’t just mimic aging-they can be reversed. And recognizing them early can change everything.
What Medications Are Hiding in Plain Sight?
Many drugs prescribed to seniors have side effects that look exactly like the signs of dementia: forgetfulness, trouble focusing, dizziness, or even personality changes. The most common offenders are anticholinergic medications. These drugs block a brain chemical called acetylcholine, which helps with memory, attention, and muscle control. When it’s blocked, the brain slows down-and that slowdown looks a lot like aging. You’ve probably heard of some of these:- Diphenhydramine (Benadryl) - used for allergies and sleep
- Oxybutynin (Ditropan) - for overactive bladder
- Tricyclic antidepressants like amitriptyline
- Quetiapine (Seroquel) - sometimes prescribed for sleep or agitation
- Promethazine - for nausea and motion sickness
How to Tell the Difference Between Aging and Medication Side Effects
True aging changes happen slowly. Dementia from Alzheimer’s or other neurodegenerative diseases doesn’t show up overnight. It creeps in over months or years. But medication side effects? They often appear suddenly. Ask yourself these questions:- Did the symptoms start within two weeks of starting a new drug or changing a dose?
- Do they get worse when the medication is taken and improve when it’s skipped?
- Is the person more confused after taking a pill, especially in the evening?
- Are there physical signs too-dry mouth, constipation, blurry vision, trouble urinating?
The Hidden Risk of Polypharmacy
Most seniors aren’t on just one medication. They’re on five, six, or more. This is called polypharmacy. And it’s not just about the drugs themselves-it’s about how they interact. When you take four or more medications, your risk of a bad reaction jumps dramatically. One drug might cause drowsiness. Another might slow your digestion. A third might blur your vision. Together, they create a perfect storm: dizziness, confusion, falls, and memory loss. The American Geriatrics Society’s Beers Criteria lists 30+ medications that are generally unsafe for people over 65. It’s not a suggestion-it’s a warning based on real-world outcomes. Yet, only 38% of primary care doctors regularly review all their senior patients’ medications. And here’s the kicker: many of these drugs were prescribed years ago for conditions that no longer exist. A sleep aid from 2015. A bladder pill from 2018. A painkiller that’s no longer needed. They just sit in the medicine cabinet, quietly doing damage.
What to Do: The 4-Step Plan
You don’t need a specialist to start fixing this. Here’s how to take action:- Make a full list of every pill, patch, cream, and supplement your loved one takes-including over-the-counter drugs and herbal remedies. Don’t rely on memory. Check the bottles.
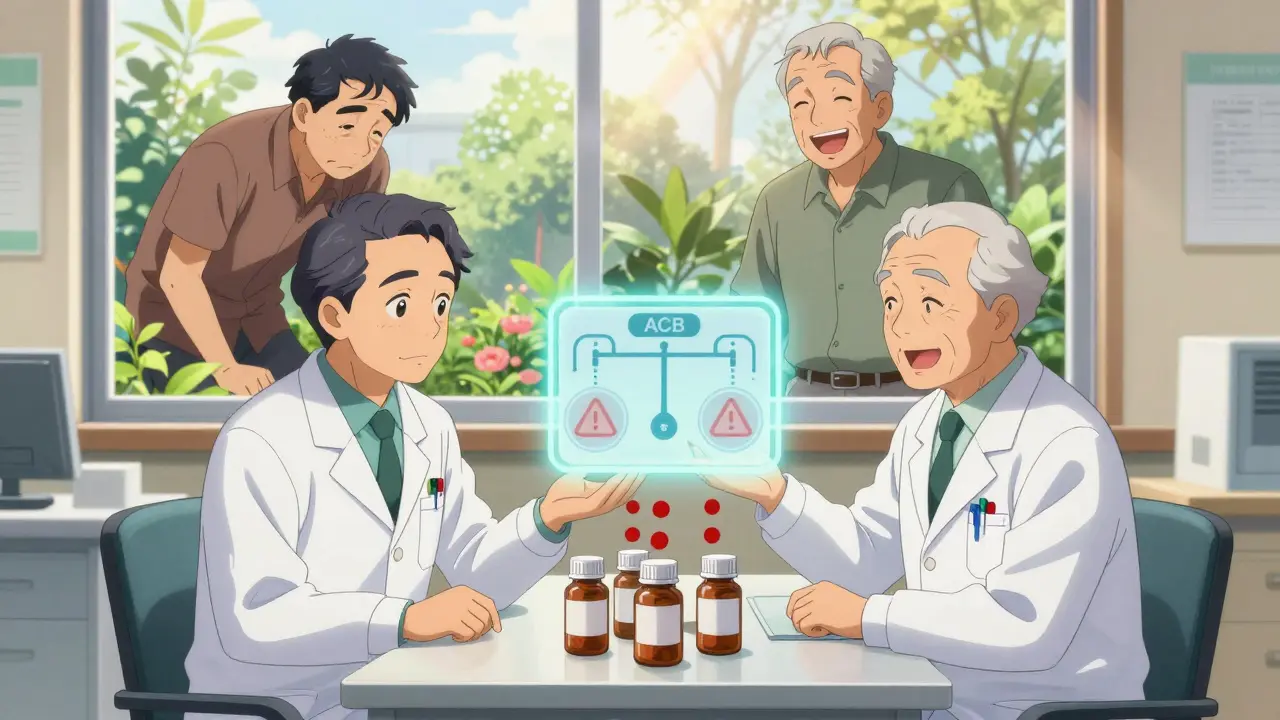
- Use the ACB scale (Anticholinergic Cognitive Burden). Each anticholinergic drug has a score: 1 (mild), 2 (moderate), or 3 (strong). Add them up. A total of 3 or higher means high risk. You can find free ACB calculators online or ask a pharmacist.
- Schedule a medication review with a geriatrician or pharmacist. Bring the list. Ask: “Which of these could be causing confusion or drowsiness?” Don’t be afraid to say, “We’re worried this might be mistaken for dementia.”
- Don’t quit cold turkey. Some drugs need to be tapered slowly. Work with a professional to reduce or replace them safely. Many side effects improve within weeks.
Other Culprits Beyond Anticholinergics
Anticholinergics are the biggest group, but they’re not the only ones:- Benzodiazepines (like Ativan or Xanax): Cause short-term memory loss in 65% of seniors. Often prescribed for anxiety or sleep, but the risk outweighs the benefit for long-term use.
- Corticosteroids (like prednisone): Can cause mood swings, confusion, and even hallucinations in older adults.
- Opioids (like oxycodone): Lead to memory fog in over half of seniors who take them regularly.
What’s Changing in 2025?
The tide is turning. The FDA now requires stronger warning labels on 17 high-risk drug classes. Medicare’s Annual Wellness Visit now legally requires a medication review. In Australia, the Pharmaceutical Benefits Scheme (PBS) is expanding pharmacist-led deprescribing programs. Researchers at Indiana University are testing a blood test that measures acetylcholine levels to spot medication-induced cognitive decline with 89% accuracy. AI tools are being trained to scan electronic health records and flag risky combinations before they’re even prescribed. But the biggest change isn’t in labs or laws-it’s in awareness. More families are asking the right questions. More pharmacists are speaking up. More doctors are listening.When to Worry: The Red Flags
Keep an eye out for these signs that point to medication side effects-not aging:- Sudden confusion or disorientation (not gradual)
- Forgetfulness that comes and goes with medication timing
- Increased drowsiness or slow movements
- New dizziness or falls (risk increases 200% with certain drugs)
- Unexplained weight loss (5+ pounds in a month)
- Dry mouth, constipation, or trouble peeing
Final Thought: It’s Not Normal-It’s Preventable
Aging doesn’t have to mean losing your mind. Many of the symptoms we blame on getting older are actually the result of outdated prescriptions, careless polypharmacy, and a system that doesn’t always check what’s in the medicine cabinet. The good news? You can fix this. You don’t need expensive tests or complicated treatments. Just a list, a question, and the courage to say: “This doesn’t feel right.” And sometimes, the most powerful medicine isn’t a pill-it’s the decision to stop one.Can medication side effects really reverse dementia-like symptoms?
Yes. Studies show that up to 30-40% of seniors diagnosed with dementia actually have medication-induced cognitive impairment. When anticholinergic drugs or other problematic medications are stopped or reduced under medical supervision, memory, focus, and alertness often improve significantly within weeks. In some cases, people return to their previous level of function entirely.
What are the most dangerous medications for seniors?
The most dangerous include first-generation antihistamines like diphenhydramine (Benadryl), bladder medications like oxybutynin, tricyclic antidepressants, antipsychotics like quetiapine, and benzodiazepines like lorazepam. These are listed in the 2019 Beers Criteria as generally inappropriate for adults over 65. Even over-the-counter sleep aids and cold medicines often contain these ingredients.
How do I know if my parent is on too many medications?
If they take four or more prescription drugs daily, they’re at risk for polypharmacy. Signs include new confusion, dizziness, falls, or memory issues after starting a new drug. Ask their pharmacist to run an ACB (Anticholinergic Cognitive Burden) score. A score of 3 or higher means high risk. Also check if any medications were prescribed years ago for issues that no longer exist-those are prime candidates for review.
Can a pharmacist help with medication reviews?
Absolutely. Pharmacists are trained to spot dangerous interactions and outdated prescriptions. Many offer free medication reviews, especially for seniors on multiple drugs. Bring a full list of everything they take-including vitamins, supplements, and OTC meds. Ask: “Which of these could be causing memory problems or drowsiness?” Pharmacists can also help create a tapering plan if a drug needs to be stopped slowly.
Is it safe to stop these medications on my own?
No. Stopping some medications suddenly can be dangerous. Benzodiazepines, antidepressants, and blood pressure drugs can cause withdrawal symptoms, seizures, or rebound effects. Always work with a doctor or pharmacist to create a safe tapering schedule. Most side effects improve over 4-12 weeks of gradual reduction, with close monitoring.
Are there any new tools to help detect these side effects?
Yes. The Anticholinergic Cognitive Burden (ACB) scale is widely used by clinicians to measure risk. New blood tests are being tested to measure acetylcholine levels, with 89% accuracy in identifying medication-induced cognitive issues. AI tools are also being developed to scan electronic health records and flag high-risk drug combinations before they’re prescribed. Medicare’s Annual Wellness Visit now legally requires a medication review, helping catch these issues early.






William Liu
December 17, 2025 AT 22:02This is the kind of post that should be shared with every family with an older relative. I didn’t realize how many OTC meds were quietly wrecking my dad’s brain until his pharmacist flagged three anticholinergics he’d been on for years. He’s been back to his crossword puzzles in six weeks. No magic pill-just stopping the wrong ones.
It’s not aging. It’s negligence.
Nicole Rutherford
December 19, 2025 AT 06:57Of course it’s aging. People just don’t want to accept that their parents are slipping. These ‘medication fog’ stories are cherry-picked anecdotes. If it were that easy, doctors would’ve caught it decades ago. You think your grandma’s forgetfulness is because of Benadryl? It’s dementia. And no amount of pharmacist reviews changes that.
Stop pushing false hope.
Chris Clark
December 19, 2025 AT 22:21Man, I just had this exact thing happen with my aunt in Ohio. She was on oxybutynin for 7 years, diphenhydramine for sleep, and amitriptyline for ‘nerves.’ Total ACB score of 8. She was calling me three times a day asking who I was. We took her to a geriatric pharmacist-boom, stopped all three. Two months later she was baking pies again and remembered my dog’s name. I didn’t even know you could check ACB scores online. Saved her from a nursing home.
Also, side note: don’t trust your doctor to catch this. They’re overworked. Go straight to the pharmacist. They’re the real MVPs.
And yeah, I know Benadryl’s in like 70 cold meds. Read the labels. It’s wild.
Carolyn Benson
December 19, 2025 AT 23:10Let’s not romanticize this. The system is broken, yes-but the real issue is the commodification of elder care. We treat aging as a medical problem to be managed, not a human experience to be honored. We’re so obsessed with reversing ‘symptoms’ that we forget the dignity of decline. Maybe some of these ‘reversals’ are just chemical illusions. Maybe the real medicine is acceptance, not deprescribing.
And yet… I still made my mother’s list. And I still took it to the pharmacist. Because even if it’s an illusion, it’s a kind one.
Chris porto
December 20, 2025 AT 17:14I’ve seen this too. My uncle was diagnosed with early Alzheimer’s. Family was crying. We got his meds reviewed-turned out he was on three things that should’ve been pulled years ago. Within a month, he was telling stories again, even remembered his wedding date. It wasn’t a miracle. It was just someone finally looking at the whole picture.
Doctors don’t have time. Pharmacies do. Take the list. Go. Don’t wait for permission.
Frank Drewery
December 20, 2025 AT 18:59Thank you for this. My mom’s been on quetiapine for ‘sleep’ since 2019. She’s been zoning out, forgetting meals, walking into walls. I thought it was just… getting old. Now I know it’s the meds. I’m calling her pharmacist tomorrow. I’m scared, but I’m doing it.
You’re right-it’s not normal. And it’s not inevitable.
shivam seo
December 22, 2025 AT 15:22Australia’s PBS is finally doing something right? Funny. We’ve been doing this since 2010. Meanwhile, the US still lets pharmacies sell Benadryl like candy. You think your grandma’s confused? Try living in a country where every second person is on antidepressants and opioids. This isn’t medicine. It’s pharmaceutical colonialism.
Andrew Kelly
December 23, 2025 AT 23:16Wake up. This is all part of the ‘anti-pharma’ agenda. The FDA doesn’t care about seniors. They care about liability. The ‘ACB scale’? Made up by people who hate Big Pharma. The ‘reversal’ stories? Placebo effect. The real cause of dementia? Vaccines. 5G. Glyphosate. You think it’s a pill? It’s the chemicals in your water. Read the studies-none of this is peer-reviewed. They’re just selling fear to push ‘natural’ supplements.
Don’t fall for it.
Ashley Bliss
December 24, 2025 AT 14:18I’m not saying this isn’t important-but why is it always the woman’s job to fix this? My mother’s meds were reviewed by me, her daughter, because her doctor didn’t even ask if she was taking NyQuil. Why is it left to daughters to become amateur pharmacists? Why isn’t this built into the system? Why do we have to beg for basic care?
And now I’m crying because I realized I’ve been doing this for three years and no one thanked me. No one even noticed.
Dev Sawner
December 25, 2025 AT 05:01It is an established fact that polypharmacy among geriatric populations constitutes a significant public health concern. The anticholinergic burden scale, as validated by the American Geriatrics Society, demonstrates a clear dose-response relationship between cumulative anticholinergic exposure and cognitive decline. Furthermore, the Beers Criteria, updated in 2019, explicitly contraindicates the use of first-generation antihistamines in patients over 65 due to their high risk-benefit ratio. The onus lies upon healthcare providers to conduct systematic medication reconciliation at every visit. Failure to do so constitutes a breach of the standard of care.
Moses Odumbe
December 25, 2025 AT 09:11Bro. I just checked my dad’s meds. He’s on Benadryl, oxybutynin, and trazodone. ACB score: 6. 😱
He’s been acting like a zombie since 2021. I thought he was just tired. Turns out he’s been on a chemical leash.
Going to the pharmacy tomorrow. Fingers crossed.
PS: If you’re reading this and your grandpa takes NyQuil… stop. Just stop. 💀
bhushan telavane
December 26, 2025 AT 12:03I’m from India. We don’t have geriatric pharmacists. Elders take whatever the doctor gives, and the doctor gives whatever the rep pushes. My grandfather was on three sleeping pills and a muscle relaxant. He forgot my name for six months. We stopped them all-no tapering, just quit. He got better. Not perfect. But better. This isn’t just a Western problem. It’s everywhere.
Connie Zehner
December 27, 2025 AT 15:06You think this is bad? My mom’s on 11 meds. She’s 82. She’s been on 8 of them since 2008. I found a bottle of lorazepam from 2012 in her drawer. She didn’t even know it was there. I cried. I yelled. I called her doctor. He said ‘It’s fine.’ I told him to look at her eyes. She’s not sleeping. She’s sedated. And now I’m the villain for ‘trying to control her.’
Why does no one listen?