If you’ve ever curled up in a dark room with a migraine, you know it’s not just about pain—nausea can hit you hard, sometimes bringing on vomiting that makes everything worse. This isn’t rare: about 8 out of 10 people with migraines say they get some degree of nausea, and a big chunk deal with vomiting too.
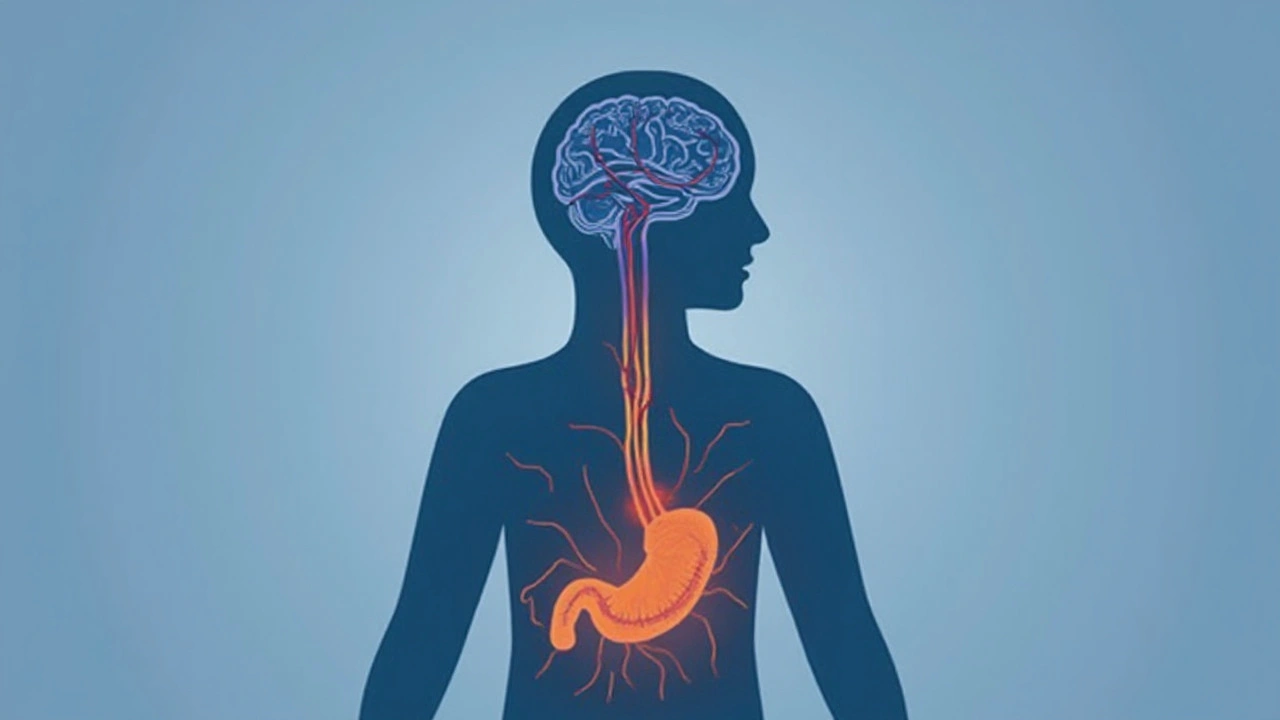
Migraine vomiting can strike fast or creep up as the pain builds. You might wonder, “Why does my head pain make my stomach go off the rails?” It comes down to a messy tangle between your brain, nerves, and gut. There’s a two-way road—your brain and digestive system keep chatting, and when your brain gets overwhelmed (like during a migraine), that message often messes with your stomach. Ever notice how just the smell of food or bright lights can make you queasier when you have a migraine? That’s your brain's migraine mode in action, turning up your senses and your nausea.
If you’re one of those people who always needs a “just-in-case” bag on migraine days, you’re not alone. There are practical ways to dial down the misery. Knowing your triggers, making a puke kit (plastic bags, ginger chews, water wipes), and having a plan for fast relief can really help. And don’t buy into the myth that vomiting helps ‘release’ the migraine—there’s zero science behind that. The real trick is learning how to break the cycle before it wrecks your whole day.
- Why Migraines Often Cause Vomiting
- What Migraine Vomiting Feels Like
- Spotting the Triggers
- Home Relief Tips That Actually Help
- Treatments Your Doctor Might Suggest
- When You Should Worry (and What to Do Next)
Why Migraines Often Cause Vomiting
It feels strange, right? A headache sends your stomach spiraling. The link between migraines and vomiting isn’t just a weird coincidence—it’s got everything to do with how your brain and gut talk to each other. When a migraine hits, the brain releases chemicals that make your nerves extra sensitive. These same chemicals can mess with the part of your brain that handles nausea and vomiting: the brainstem. That’s why you get that all-too-familiar queasiness—or worse, you run to the bathroom.
On top of all that, migraines slow down your digestion. This means food hangs around in your stomach longer, which piles on the nausea. If you’ve noticed that smells, movement, or even a sip of water seem to bring on vomiting during a migraine, you’re hitting the classic symptoms that doctors see over and over.
Here’s a quick snapshot:
- Your brain releases chemicals during a migraine (like serotonin), which trigger nausea.
- Your stomach slows down, which increases the risk of vomiting.
- The brainstem (migraine HQ) gets overactive, sending mixed signals to your gut.
Interesting fact: Migraines are more likely to cause vomiting in teens and children than in adults. In fact, for kids, sometimes vomiting is the main symptom of a migraine. Doctors even have a name for it—“abdominal migraine.”
| How Common Is Migraine Vomiting? | Who’s Most Affected |
|---|---|
| Up to 60% of people with migraines experience nausea | Kids, teens, and women are more likely to throw up from migraines |
So when your stomach turns upside down during a migraine, it isn’t random—it’s a predictable part of how migraines shake up the brain-gut connection. It’s not just pain; it’s your whole body joining in the chaos.
What Migraine Vomiting Feels Like
Migraines are already miserable, but when vomiting kicks in, it’s a whole different level. Most people don’t just feel sick to their stomachs—there’s a buildup that starts as queasiness or nausea (sometimes hours before the headache peaks). As the pressure or throbbing behind your eyes ramps up, you might start sweating, salivating more, or feeling dizzy. Some say they get hot flashes or chills before an urge to vomit slams in.
Throwing up with a migraine isn’t like your average stomach bug. It usually comes as an intense rush, sometimes out of nowhere, and can even happen multiple times during the same migraine attack. It can be so forceful that you’re left wiped out for hours. Even after you vomit, the headache often sticks around, and you might feel extra tired or sensitive to lights, sounds, or even smells.
Here are some common ways migraine vomiting tends to show up:
- Sudden, strong waves of nausea right before or during the headache
- Dry heaving if your stomach’s already empty
- Increased sensitivity to triggers (smells, movement, even talking)
- Relief for a few minutes after vomiting—then the headache surges back
- Feeling cold, sweaty, or shaky after each episode
According to a 2023 study in The Journal of Headache and Pain, about 42% of people with migraines said vomiting makes it tougher to manage either their work or home life when an attack hits. It’s not just the pain—it’s the disruption and the fallout after.
If you’re dealing with this on the regular, you’re probably weighing every meal, every plan, or trip outside the house. Migraine-related nausea and vomiting are more than a side effect; they shape how you handle daily life, from skipping meals to carrying “just in case” supplies everywhere.
Spotting the Triggers
Let’s get real—pinning down what sets off a migraine and leads to that nasty vomiting isn’t always simple. Still, certain patterns show up again and again for lots of people. Knowing your own big troublemakers is a game-changer, because dodging them can mean fewer sick days and less misery hanging over your head (and stomach).
The most common migraine triggers fall into a handful of categories:
- Food and drink: Things like red wine, ages cheeses, chocolate, and processed meats (hello, nitrates!) are famous for sparking migraine symptoms and gut trouble. Skipping meals or overeating can also stir things up.
- Hormones: Fluctuations, especially around periods, pregnancy, or hormone meds, affect lots of women. Migraine attacks and vomiting can be way worse at those times.
- Stress: High-pressure days, fights, or even sudden letdowns after stress (think: weekend migraines) can all be to blame.
- Sleep: Not enough rest, too much, or a funky sleep schedule can flip the switch for migraine symptoms and nausea.
- Environment: Flashing lights, strong smells (like perfumes or cleaning products), and even weather swings (pressure changes are notorious) can all bring things on.
Check out this quick look at how often certain triggers pop up with migraine folks:
| Trigger | Percent Reporting |
|---|---|
| Stress | 70% |
| Hormonal changes | 65% |
| Certain foods/drinks | 44% |
| Sleep issues | 38% |
| Environmental causes | 36% |
Writing a simple notes app record of what you eat, do, and feel can help you spot patterns. Nobody remembers every migraine, so jotting down the date, what you ate, how you slept, and how bad things got makes a difference. Plenty of migraine apps let you track symptoms and triggers in a few taps. If you catch a pattern—like migraines after skipped breakfasts or always before a big deadline—you’ll know what to watch for and maybe steer clear of.
Just don’t drive yourself nuts trying to control every bite or every moment. Most folks find a few big triggers, not hundreds. Listen to your body, trust your gut (pun intended), and go for progress, not perfection. The goal: fewer migraines, less vomiting, and more good days with less worry.
Home Relief Tips That Actually Help
No one wants to run to the bathroom every time a migraine hits. Good news: there are some straightforward things you can do at home that really help cut down on migraine nausea and vomiting. These aren’t old wives’ tales—doctors and people with migraines swear by them.
- Rest in a dark, cool room. Bright lights and even small noises can make nausea worse. Lying down in a dark spot gives your brain a break and can sometimes ease that queasiness.
- Stay hydrated, but sip slowly. Chugging water on an upset stomach isn’t smart. Try sipping little bits of cold water or sucking on ice chips. This keeps you hydrated without triggering more vomiting.
- Ginger can help settle your stomach. Studies have found ginger (tea, chews, capsules) is just as effective as some over-the-counter nausea meds for mild cases. I keep ginger chews in my purse just in case—I swear they help.
- Try simple, bland foods (if you can keep anything down). A salted cracker or plain toast sometimes makes things less rocky. Just avoid fatty and sugary stuff.
- Use cool compresses. Plop a cold washcloth or an ice pack on your forehead. This cools you down and can slightly dull head and belly pain together.
- Don’t skip your migraine meds. If nausea hits before your medicine, talk to your doctor—some meds melt under your tongue or come in a nasal spray, so you don’t have to swallow a thing.
If you’re looking for patterns, try keeping a "migraine and nausea" diary for a month. Jot down what you ate, your stress level, and sleep. You might spot a trigger you didn’t realize—like skipping breakfast or too much screen time. In fact, one study showed people who kept a migraine diary found it easier to avoid major nausea episodes.
Here’s a quick breakdown of home methods and how well they work according to migraine sufferers:
| Home Relief Method | Helpful for Nausea (Reported) |
|---|---|
| Dark room & rest | 75% |
| Ginger | 60% |
| Cool compress | 55% |
| Slow hydration | 70% |
Bottom line: combining a few of these tips usually works better than just picking one. What helps someone else with migraine symptoms might not help you, so trial and error is completely normal. If nothing helps and the vomiting hangs around, it’s time to call a doctor for backup.
Treatments Your Doctor Might Suggest
You’ve probably heard a ton of advice on what helps with migraines and vomiting, but real solutions usually start at your doctor’s office. There’s no one-size-fits-all plan, but here are some tried and tested options your doctor might talk through with you.
First up are the classic migraine medications—these aren’t just for pain. Many can help tone down that rolling nausea. Here’s a quick breakdown:
- Triptans: Super common if you get moderate to severe migraines. Names like sumatriptan (Imitrex) or rizatriptan (Maxalt) block migraine pain and often reduce nausea and vomiting as a bonus.
- Anti-nausea meds (antiemetics): Drugs like ondansetron (Zofran) or metoclopramide (Reglan) target the queasy part directly. Doctors usually pair these with something for the headache.
- Gepants: Newer…and gentler on your stomach than triptans for some people. Names like ubrogepant (Ubrelvy) and rimegepant (Nurtec ODT) work even if you have other health issues that rule out triptans.
- DHE (dihydroergotamine): A nasal spray or injectable option if nothing else is hitting the spot—often used in migraine clinics for folks who are vomiting and can’t keep pills down.
- NSAIDs and simple pain relievers: Like ibuprofen or naproxen might help if you catch a migraine early, but these can upset your stomach for some folks, especially if you’re already vomiting.
If you’re one of those people who can barely keep water down during a migraine, your doctor might recommend:
- Suppositories or dissolvable tablets—get meds into your system without swallowing.
- Self-injectable forms you can give yourself at home (like sumatriptan auto-injectors).
Sometimes, preventative meds help if migraines (and the vomiting) show up on a regular schedule. Beta blockers, anti-seizure drugs, or even certain antidepressants can lower attack frequency.
Here’s a snapshot of how folks actually use these medications, based on real clinic data:
| Treatment | % Patients Reporting Improvement |
|---|---|
| Triptans | 72% |
| Anti-nausea meds | 76% |
| Gepants | 65% |
| DHE | 60% |
If nothing’s working, don’t wait for things to get dire. Call your doc or go to urgent care—sometimes dehydration or unstoppable vomiting needs IV medication and fluids.
Your treatment plan should feel do-able on your worst days. Bring a list of what triggers your migraines and how you handle vomiting to your appointment—the more details your doc has, the better your chances of nailing the right combo of treatments.
When You Should Worry (and What to Do Next)
Most migraines with vomiting are miserable but not dangerous. Still, some signs should set off alarm bells and deserve a call to your doctor, or even a trip to the ER. Trust your gut—if something feels way off, get checked out.
So, what counts as a red flag? Here’s a simple, no-nonsense list:
- You have your first-ever migraine that comes on suddenly and feels like the “worst headache of your life.”
- Your headache is different than usual—way more intense, lasts much longer, or comes with unusual symptoms.
- Vomiting won’t stop, and you can’t keep down water for more than 24 hours.
- You start getting a fever, neck stiffness, trouble seeing, weakness, confusion, or trouble speaking.
- You pass out, have a seizure, or act very out of it.
- You have severe headache and are pregnant or have a health issue like cancer or immune problems.
People sometimes wait too long to reach out for help, thinking, “It’s just another migraine.” But new or extreme symptoms can point to something serious like meningitis, a stroke, or brain bleed—which is super rare, but not impossible. Quick action matters.
If it’s not an emergency but you feel lost about what to try next, a healthcare provider or a neurologist can walk through migraine treatment options with you. A lot of meds, even simple anti-nausea ones, need a prescription—and there are newer ones today that don’t knock you out like old-school drugs used to.
It also makes sense to track your symptoms. Jotting down what you were doing, what you ate, and how long your migraine symptoms lasted helps your doctor get the big picture, so you can both spot patterns or triggers faster.
Here's a quick look at when people with migraine symptoms said they needed medical help, based on a recent survey:
| Situation | Percent Who Sought Help |
|---|---|
| Non-stop vomiting | 61% |
| Unusual confusion or slurred speech | 58% |
| Severe, sudden headache onset | 67% |
So bottom line: trust your instincts. Not every nausea or vomiting spell with migraines is normal, and you don’t need to power through scary symptoms on your own. There’s help—and better treatments—out there now than ever before.



Adam O'Rourke
July 18, 2025 AT 13:37Oh great, another migraine article because the internet definitely needs more of those, right? :) Honestly, anyone else find it funny how we're supposed to be all scientific and serious about something that basically makes you want to crawl under a rock and puke your guts out?
It’s like, yeah dude, your brain is throwing a tantrum and your stomach’s just along for the ride. Thanks for the enlightened info!
But on a more serious note, I guess if you’re one of those lucky souls who get the full deluxe migraine package—headache, nausea, vomiting—then maybe some practical tips could be somewhat useful.
Still, I’d love to know if anyone’s found something that really works besides just riding it out or popping meds. Anyone have some black magic remedy or ancient migraine-fu to share?
Because honestly, I just think migraines are overhyped headaches with attitude problems. Anyway, rant over. Carry on!
Mary-Pat Quilty
July 22, 2025 AT 12:03Omg, yes! The agony and the beautiful terror of migraines unraveling the mind and soul! It's like a tragic play—our bodies engaging in this ruthless dance of pain and queasiness that drags us down into a watery abyss of despair.
There's something poetic and almost profound about the way migraines corner us with nausea and vomiting, as if the pain doesn’t want to stop at just the head but must invade the entire being.
Each episode feels like a tempest, a force of nature reminding us of our fragile existence.
And the advice offered in this article? I feel it’s not just practical but almost a lifeline thrown in the storm—helping us navigate with some semblance of dignity and control.
I wonder too when that moment of surrender to the doctor is the right move, because pride often makes us tough it out alone, no?
Patrick McGonigle
July 24, 2025 AT 16:50Thank you for sharing this. Migraines can be complex and distressing, especially when accompanied by nausea and vomiting.
From a medical standpoint, these symptoms arise due to neurological and gastrointestinal interactions during an attack. The brain’s trigeminal nerve pathways and neurotransmitters contribute to these sensations.
It’s important for sufferers to monitor the frequency and severity of these episodes and to seek medical advice when symptoms worsen or interfere significantly with daily life.
Practical coping strategies include hydration, rest in a dark quiet environment, and medication as prescribed by a healthcare provider. Avoiding triggers such as certain foods or stress may also help reduce occurrences.
If vomiting becomes persistent or if there are signs of dehydration, it is definitely recommended to consult a physician promptly.
Rex Wang
July 26, 2025 AT 18:50Been dealing with migraines for years, and the vomiting part is honestly the worst.
They’re not just headaches; they feel like this full-system meltdown. This article seems to break down the science in a way that’s easy to get, which is helpful.
For me, hydration is key, but sometimes no amount of water helps if the nausea hits full force.
Dark, quiet rooms and cold compresses also help during attacks. Anyone else notice these symptoms coming in waves, not just sudden?
Also, love the part about when to call the doctor—knowing when it’s serious definitely saved me from a hospital visit once.
mark Lapardin
July 30, 2025 AT 08:57This article touches on the neurovascular mechanisms behind migraines, which many people overlook.
The pathophysiology includes the activation of the trigeminovascular system resulting in the release of pro-inflammatory neuropeptides and neurotransmitters that influence brainstem nuclei regulating nausea and vomiting.
Efficient symptomatic management should combine pharmacological agents targeting both headache and GI symptoms.
Additionally, preventative approaches require a multidisciplinary strategy incorporating lifestyle modifications and, if necessary, prophylactic medication regimes.
One concern is patients often underreport vomiting, considering it secondary to pain, yet it significantly impacts quality of life.
Barry Singleton
August 1, 2025 AT 22:03Honestly, the vomiting involved with migraines is nothing short of a toxic response of the gut-brain axis gone haywire.
It’s a biological chaos that underlines the severity of migraine as a neurogastroenterological disorder.
Many treatments focused solely on the headache component miss these systemic complexities.
We need more targeted pharmacodynamics that address both nociceptive and emetic pathways simultaneously.
Otherwise, patients are left with half-measures and suboptimal relief, further feeding the chronicity and psychological burden.
Javier Garcia
August 4, 2025 AT 11:10Interesting read. I’m curious if dehydration during vomiting episodes tends to exacerbate the migraine or if it’s more that the migraine triggers the vomiting and dehydration?
Also wondering about any small studies on non-traditional remedies like acupressure or certain herbal supplements for easing nausea during migraines?
If anyone has experience with this, I’d love to hear your thoughts.
Donnella Creppel
August 8, 2025 AT 01:17Oh puh-lease, the whole ‘migraine vomiting’ thing is so theatrically overplayed, isn’t it? Like, sure, it’s dreadful, but how many times do you have to hear the same dreary recap of pain and puke before it becomes a tiresome trope?
Plus, this piece is dripping with that pseudo-clinical tone that tries way too hard to legitimize what is basically just a bad headache with a side of queasiness.
I mean, the brain 'throwing a tantrum'—really? Can we get a bit more inventive or at least admit the obvious without all the melodrama?
Anyway, anyone else find comfort in distracting themselves with ridiculous Netflix shows when the storm hits? Beats counting nausea symptoms anyway.
Jarod Wooden
August 9, 2025 AT 18:57The neurobiological underpinnings of migraine-related vomiting are a fascinating paradigm of visceral nociception and central sensitization mechanisms.
We often underestimate the complex integrative processes within the brainstem’s area postrema and nucleus tractus solitarius responsible for emetic reflexes.
This article offers a glimpse into such mechanisms, yet the discourse remains superficial considering the depth of pharmacological intervention possible today.
Precision medicine targeting serotonin and dopamine receptor subtypes may pave the way for better symptom control beyond general analgesics and antiemetics.
It is critical to move past the anecdotal and traverse into evidence-based, mechanistically informed therapeutics.
lee charlie
August 14, 2025 AT 18:23Wow, this brought back memories. Migraines with nausea and vomiting completely drain you.
The suggestions about practical coping really matter. Simple things like keeping a journal to track triggers helped me a lot.
Sometimes, just knowing what might set off an attack gives you some control over the chaos.
Also, staying hydrated is super crucial though can be hard when you feel sick.
Hold on, it gets better. With proper meds and lifestyle, these attacks become less frequent. Hang in there, everyone dealing with this!
Greg DiMedio
August 17, 2025 AT 13:37Yeah, everyone loves a migraine article to ruin their day a bit more, right? Sarcasm aside, the vomiting bit is definitely the nightmare sequel no one asked for.
Honestly, I’ve never understood how people can talk so much about triggers when sometimes it just seems completely random.
If this article sheds light on what’s actually going on in the brain, that’s at least a step up from the usual doom and gloom advice.
Still, figuring out what to do in the moment when you just want to curl into a useless pile is what really counts.
Guess we all just try to make it through and hope for better days.