What Exactly Is a TIA?
A Transient Ischemic Attack, or TIA, isn’t a mild stroke. It’s not even a "mini-stroke"-that term is misleading and dangerous. A TIA happens when blood flow to part of the brain is blocked briefly, causing stroke-like symptoms that go away quickly. But here’s the catch: even though the symptoms disappear, your brain may have been in serious danger. The American Heart Association updated its definition in 2023 to focus on tissue damage, not how long symptoms lasted. If there’s no permanent brain injury seen on an MRI, it’s a TIA. If there is-even if you felt fine after 20 minutes-it’s a stroke. That’s why calling it a "mini-stroke" is wrong. You didn’t have a small stroke. You had a warning shot across your bow.
How Do You Know It’s a TIA and Not Just a Passing Dizziness?
The symptoms of a TIA are identical to those of a stroke. They come on suddenly. No warning. No gradual buildup. You might notice one side of your face drooping when you try to smile. Your arm might drop when you try to raise it. Words come out jumbled or you can’t find them at all. Vision blurs in one eye. You feel off-balance, like the floor is tilting. A headache hits-severe, unlike any you’ve had before.
What makes a TIA different? It fades. Usually within 10 to 60 minutes. About 56% of cases resolve in under an hour. But here’s what most people don’t realize: just because the symptoms vanished doesn’t mean the threat is gone. In fact, the opposite is true. The moment symptoms disappear, the clock starts ticking. The highest risk of a full-blown stroke happens in the next 48 hours. One in five people who have a TIA will have a stroke within 90 days. Half of those strokes happen within the first two days.
Why Time Is the Most Critical Factor
There’s no waiting. No "I’ll see how I feel tomorrow." If you or someone else has sudden neurological symptoms-even if they’re gone now-you call 911. Not your doctor. Not your spouse. 911. Emergency responders are trained to recognize these signs and get you to a hospital with the right imaging and stroke team already on standby.
Why so urgent? Because treatment begins the moment you walk in the door. Doctors use a tool called the ABCD2 score to quickly assess your risk. It looks at your age (60 or older = 1 point), blood pressure (140/90 or higher = 1 point), whether you had weakness on one side (2 points) or just speech trouble (1 point), how long symptoms lasted (60+ minutes = 2 points, 10-59 minutes = 1 point), and if you have diabetes (1 point). A score of 4 or higher means you have an 8% chance of having a stroke in the next two days. That’s not a risk you gamble with.
Studies show that getting evaluated within 60 minutes cuts your stroke risk by 80%. At Massachusetts General Hospital, their SOS-TIA program got 95% of patients seen the same day. Their 90-day stroke rate dropped to 1.2%. Compare that to the national average of 10.3% for people who waited. That’s not a difference. That’s a life saved.
What Happens in the Emergency Room?
First, they rule out bleeding in the brain with a non-contrast CT scan. That’s quick. Then they move to MRI with diffusion-weighted imaging-the gold standard. This scan can spot tiny areas of brain damage that a regular CT misses. About 35% of people who think they had a TIA actually have a small stroke. The damage was there all along; they just didn’t feel it long enough to notice.
If it’s confirmed as a TIA, treatment starts immediately. Aspirin (325 mg) is given within 24 hours. That alone reduces your next stroke risk by 60%. For higher-risk patients, doctors add clopidogrel for 21 to 30 days. That dual therapy cuts stroke risk even further. You’ll also get a high-dose statin-atorvastatin 80 mg daily-to stabilize plaque in your arteries. Blood pressure is brought under control, ideally below 140/90. If you have atrial fibrillation, you’ll likely start on a blood thinner.
It’s not just about drugs. You’ll get screened for carotid artery narrowing. If there’s a major blockage, you might need surgery or a stent. Lifestyle changes aren’t optional. Quit smoking. Start moving. Eat real food-not processed junk. These aren’t "nice to haves." They’re survival tools.
The Big Misconception: "It Went Away, So It’s Not a Big Deal"
Thirty-one percent of people with TIA wait more than 24 hours to get help. Why? Because they think, "It’s gone. I’m fine." That’s the deadliest myth in neurology. A TIA isn’t a brush with danger. It’s a full-on alarm system going off. Your body is screaming that your brain is one clot away from permanent damage.
And here’s something even scarier: new research from the University of California shows that nearly half of people diagnosed with TIA have subtle brain injuries detectable only with advanced MRI. That means even if you feel 100% better, your brain may already be damaged. The symptoms disappeared-but the injury didn’t. That’s why calling it a "transient" attack is misleading. The damage might be invisible, but it’s real.
What Comes After the Emergency?
Getting through the ER is just step one. The real work starts after you’re discharged. You need follow-up within a week. A neurologist will review your imaging, check your medications, and make sure you’re on the right path. You’ll need regular blood pressure checks, cholesterol monitoring, and possibly a sleep study if sleep apnea is suspected-because it’s a hidden stroke risk.
Insurance and hospitals are now being held accountable. The Centers for Medicare & Medicaid Services penalize hospitals if more than 20% of TIA patients have a stroke within 30 days. That’s why most major hospitals now have dedicated TIA clinics. Some even use telemedicine to connect you with specialists the same day. AI tools are now predicting stroke risk with 92% accuracy by analyzing MRI patterns and patient history. These aren’t sci-fi gadgets-they’re in use right now.
What You Can Do Today
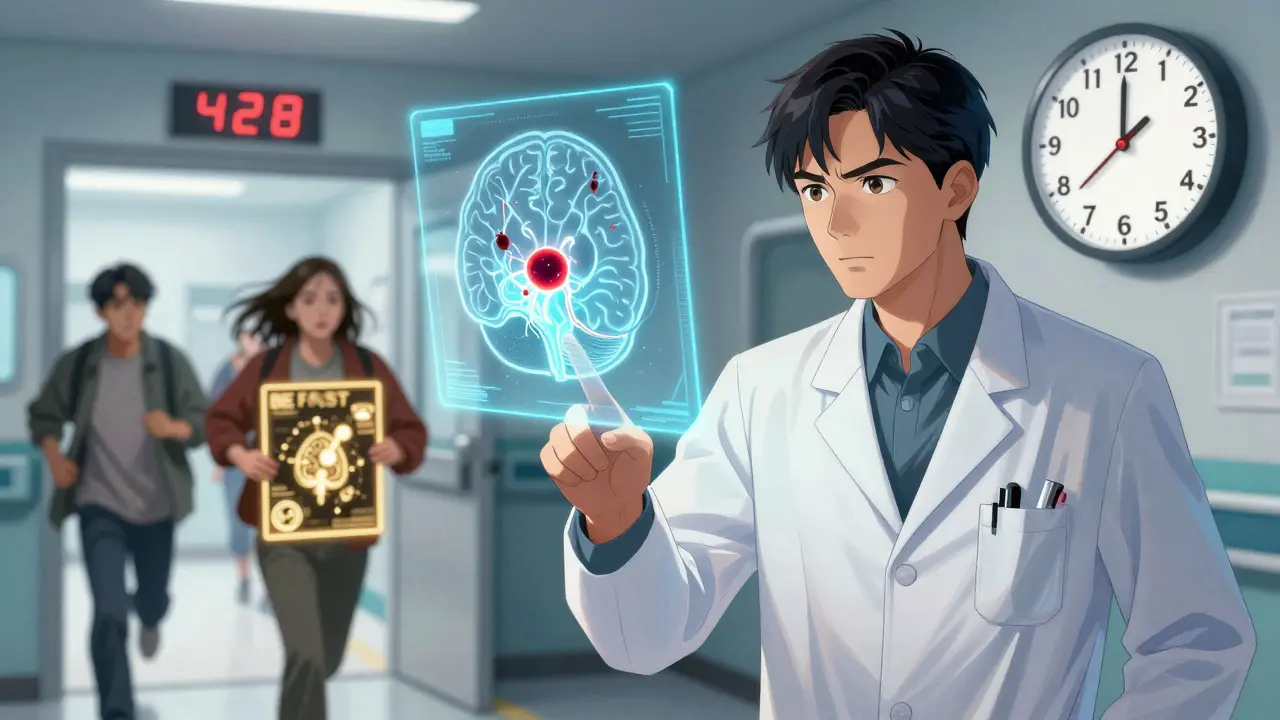
Learn BE FAST. It’s simple:
- Balance: Sudden dizziness or loss of balance
- Eyes: Blurred or double vision
- Face: One side drooping
- Arm: Weakness or numbness on one side
- Speech: Slurred, strange, or hard to understand
- Time: Call 911 immediately
Don’t wait. Don’t call your doctor first. Don’t try to sleep it off. Don’t assume it’s just stress or fatigue. If any of these signs appear-even for a minute-call 911. Every second counts.
And if you’ve had a TIA before? Make sure your medications are up to date. Don’t skip your statin. Don’t ignore your blood pressure. Your next stroke might not be preventable if you don’t treat this one like the emergency it is.
It’s Not a Warning. It’s Already Happening.
Dr. Steven Levine from Northwell Health says it best: "TIA is not a warning. It’s an actual stroke event that resolved spontaneously." That’s the truth. Your brain had a stroke. The clot dissolved. The blood flow returned. But the event still happened. The damage might be invisible, but the risk isn’t. You’re not lucky to have survived. You’re at high risk-and you need to act like it.
Final Thought: Your Brain Can’t Afford to Wait
One in three people who have a TIA will have a stroke. That’s not a small chance. That’s a coin flip. And unlike a coin, you can’t just flip again. The next stroke could be worse. It could leave you paralyzed. Unable to speak. Dependent on others for everything. It doesn’t have to happen. But only if you treat the TIA like the emergency it is.
Can a TIA happen without symptoms?
No, a TIA by definition involves noticeable neurological symptoms-like weakness, speech trouble, or vision loss-that come on suddenly. However, some people may mistake the symptoms for something else, like a migraine or vertigo, and not realize what happened. If you suddenly felt off for a few minutes and can’t explain why, it’s worth getting checked.
Is a TIA less serious than a stroke?
No. A TIA is not less serious-it’s more urgent. While a stroke causes permanent brain damage, a TIA is a clear signal that a stroke is likely to follow. Up to 20% of people who have a TIA will have a stroke within 90 days, and half of those happen within the first two days. Ignoring a TIA is like ignoring a smoke alarm because the fire hasn’t spread yet.
Do I need imaging if my symptoms are gone?
Yes. Even if you feel fine, you need an MRI with diffusion-weighted imaging. About 35% of people who think they had a TIA actually have a small stroke visible on MRI. Without imaging, you might be misdiagnosed and miss critical treatment. Symptoms disappearing doesn’t mean the event didn’t happen.
Can I just take aspirin and skip the hospital?
No. Aspirin helps reduce future stroke risk-but only after you’ve been properly evaluated. You need to rule out bleeding in the brain, check for carotid artery blockages, and assess your overall risk profile. Taking aspirin alone without medical evaluation could delay life-saving treatment.
How soon after a TIA should I see a neurologist?
Within 7 days, but sooner is better. High-risk patients (ABCD2 score ≥4) should be seen within 24-48 hours. Your neurologist will adjust your medications, order follow-up tests, and create a long-term prevention plan. Delaying specialist care increases your stroke risk significantly.





