Complementary Therapy Matchmaker
Find Your Best Fit
Answer these questions to get personalized recommendations for complementary therapies that work with your current asthma management.
Recommended Therapies
Important: Always discuss complementary therapies with your healthcare provider before starting. These recommendations are educational only.
Bronchial Asthma is a chronic inflammatory disease of the airways that causes wheezing, shortness of breath, and coughing. It affects roughly 339 million people worldwide, according to the World Health Organization’s 2023 report. While inhaled corticosteroids and bronchodilators remain the backbone of treatment, many patients look for alternative therapies asthma to reduce flare‑ups, lower medication doses, or simply feel more in control of their health.
Why Consider Alternative Therapies?
Modern medicine has an impressive track record, but it’s not a one‑size‑fits‑all solution. Side‑effects, adherence challenges, and the desire for a more holistic approach push people toward complementary options. When used responsibly, these therapies can address triggers, improve lung function, and boost overall wellbeing-provided they don’t replace prescribed medication without a doctor’s approval.
Key Conventional Pillars (A Quick Refresher)
Before diving into alternatives, it’s useful to recall the main drug classes that keep asthma under control.
- Inhaled Corticosteroids - reduce airway inflammation and are the first‑line controller therapy.
- Short‑acting beta‑agonists (SABAs) - rescue inhalers for sudden symptoms.
- Long‑acting beta‑agonists (LABAs) - used alongside steroids for better control.
- Leukotriene modifiers - oral agents that block inflammatory pathways.
Understanding these helps you see where complementary methods can fit in without causing conflicts.
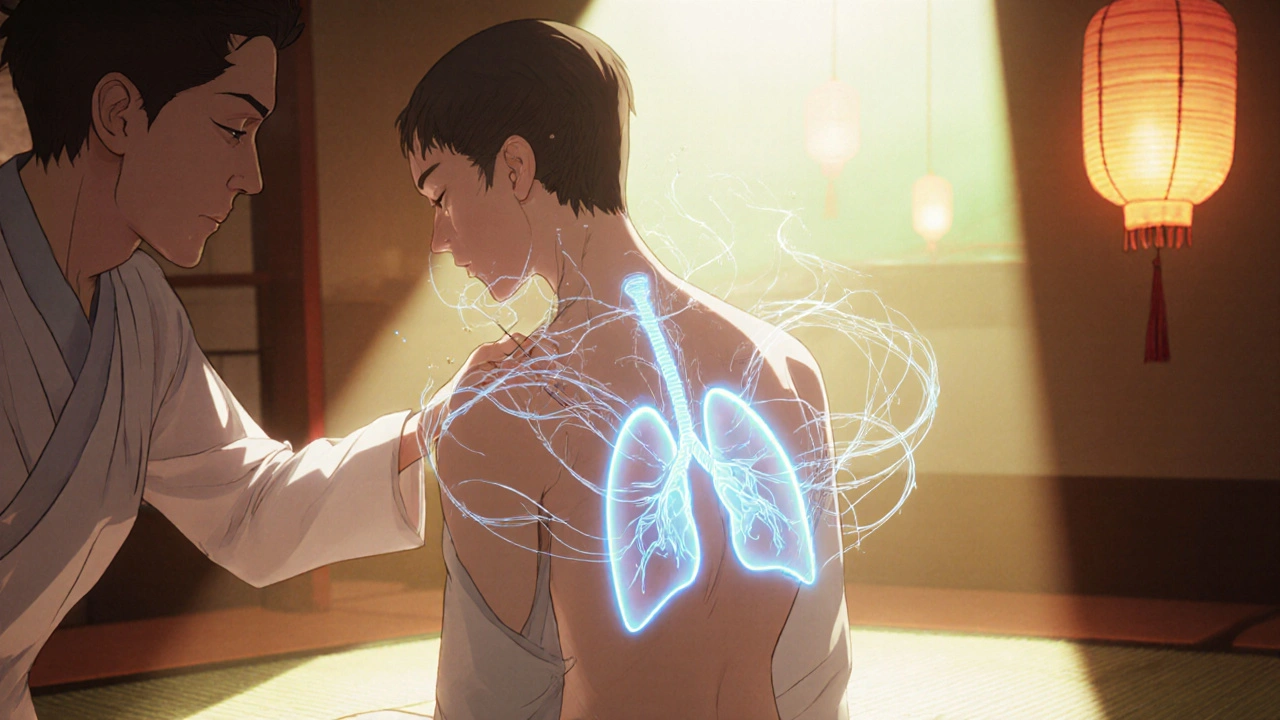
Acupuncture - Needle‑Based Modulation
Acupuncture involves inserting fine needles at specific points to balance the body’s energy flow, or "Qi." A 2022 meta‑analysis of 15 randomized trials (over 1,200 participants) found modest improvements in FEV1 (forced expiratory volume) and a reduction in rescue inhaler use. The most commonly targeted points are LU1 (Zhongfu) and ST36 (Zusanli), which are believed to influence lung function and immune response.
Safety note: Use only licensed practitioners; avoid needling near infection sites or if you have a bleeding disorder.
Yoga and Breathing Exercises - Mind‑Body Integration
Yoga Breathing (Pranayama) focuses on controlled inhalation and exhalation, strengthening respiratory muscles and calming the autonomic nervous system. Studies from the Indian Journal of Physiology and Pharmacology (2023) show that a 12‑week program of diaphragmatic breathing and alternate nostril breathing decreased asthma symptom scores by 30 %.
Practical tip: Start with 5‑minute sessions twice a day, gradually extending to 15 minutes. Pair with gentle postures like Cat‑Cow and Child’s Pose to open the thoracic cavity.
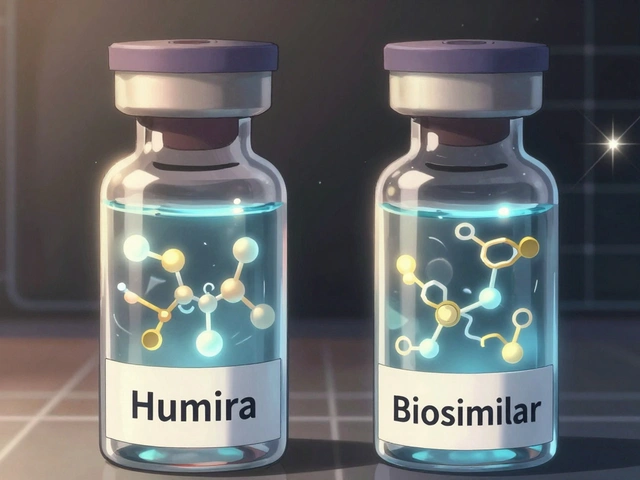
Herbal Medicine - Plant‑Based Agents
Herbal Medicine covers a wide range of botanicals used traditionally for respiratory health. Two that have solid research backing are:
- Boswellia serrata (Indian frankincense) - contains boswellic acids that inhibit 5‑LOX, an enzyme involved in leukotriene production. A double‑blind trial in 2021 showed a 22 % reduction in nocturnal cough.
- Butterbur (Petasites hybridus) - acts as a mast cell stabilizer. An Australian cohort (2022) reported fewer exacerbations when butterbur extract (75 mg twice daily) was added to standard therapy.
Always check for potential interactions, especially with warfarin or corticosteroids.
Vitamin D - The Sunshine Vitamin
Vitamin D deficiency is common in people with asthma, particularly in higher latitudes like Melbourne. A 2024 systematic review linked serum 25‑OH‑D levels above 30 ng/mL with a 15 % lower risk of severe exacerbations. Supplementation (1,000-2,000 IU daily) is generally safe, but overdosing can cause hypercalcemia.
Probiotics - Gut‑Lung Axis Support
Probiotics such as Lactobacillus rhamnosus GG and Bifidobacterium lactis may modulate immune responses through the gut‑lung axis. A 2023 pediatric study showed a 10 % reduction in emergency visits when children received a daily probiotic for six months.
Best practice: Choose a product with at least 10 billion CFU and store it in a cool, dry place.
Environmental Modifications - Air Purifiers and Allergen Control
Air Purifier use HEPA filters to capture pollen, dust mites, and pet dander. Real‑world data from a 2023 Melbourne housing study indicated a 12 % decrease in peak flow variability after six weeks of continuous purifier use in bedrooms.
Other measures include: regularly washing bedding in hot water, using dust‑mite‑proof covers, and keeping indoor humidity below 50 % to deter mold.
Comparing Popular Alternative Options
| Therapy | Primary Mechanism | Evidence Level (2020‑2024) | Typical Use | Safety / Precautions |
|---|---|---|---|---|
| Acupuncture | Neuro‑immune modulation via specific meridian points | Moderate - 15 RCTs, meta‑analysis shows modest FEV1 gain | Weekly sessions for 8-12 weeks | Use certified practitioner; avoid if bleeding disorder |
| Yoga / Pranayama | Improved diaphragmatic strength, vagal tone enhancement | Strong - multiple controlled trials, 30 % symptom score reduction | 5‑15 min daily breathing exercises + gentle posture | Watch for hyperventilation; modify if joint pain |
| Herbal (Boswellia, Butterbur) | Anti‑inflammatory via COX/LOX inhibition, mast cell stabilization | Low‑moderate - limited RCTs, promising but need larger studies | Standardized extracts 1-2 times daily | Potential drug interactions; monitor liver enzymes |
| Vitamin D Supplement | Immune regulation, reduces Th2‑mediated inflammation | Strong - systematic reviews link adequate levels to reduced exacerbations | 1,000-2,000 IU daily, adjust based on serum test | Risk of hypercalcemia if >4,000 IU without monitoring |
| Probiotics | Modulates gut microbiota → lung immune response | Emerging - pediatric RCTs show modest benefit | 10 billion CFU daily, preferably with meals | Rare GI upset; avoid in immunocompromised patients |
Integrating Alternatives with Standard Care
The safest route is to treat alternative methods as adjuncts, not replacements. Here’s a practical checklist to discuss with your asthma specialist:
- List every complementary therapy you’re considering.
- Ask for potential drug‑herb interactions (e.g., butterbur with corticosteroids).
- Request baseline tests: lung function (spirometry), vitamin D level, and, if relevant, a stool analysis for gut health.
- Set measurable goals: e.g., reduce SABA use from 3×/day to ≤1×/day within 4 weeks.
- Schedule a follow‑up after 8-12 weeks to assess effect and adjust treatment.
Documenting outcomes in a simple diary (symptom score, night awakenings, rescue inhaler puffs) helps both you and your clinician see real progress.
Potential Pitfalls & How to Avoid Them
- Self‑diagnosing. Never stop inhaled steroids based solely on feeling better.
- Unregulated supplements. Choose products with third‑party testing (e.g., USP, NSF).
- Over‑reliance on a single therapy. Combine breathing exercises with environmental control for best results.
- Ignoring triggers. Keep a trigger diary; allergens, cold air, exercise, and stress often stay the biggest culprits.
Mini‑FAQ - Your Most Common Questions
Can I replace inhaled steroids with herbal remedies?
No. Herbs may lower inflammation, but they don’t provide the consistent, dose‑controlled effect of inhaled corticosteroids. Use them only as supplemental support after doctor approval.
Is acupuncture safe for children with asthma?
Most studies involve adults, but a few pediatric trials report safety when performed by licensed pediatric acupuncturists. Always verify credentials and discuss with your pediatrician.
How long does it take to see benefits from yoga breathing?
People often notice reduced shortness of breath after 2-3 weeks of daily practice, with larger lung‑function gains emerging around 8-12 weeks.
Do air purifiers really help asthma control?
HEPA‑based units can lower indoor allergen counts, which translates to modest improvements in peak flow variability for many users. They work best when paired with regular cleaning and humidity control.
What dosage of vitamin D is safe for adults with asthma?
Most guidelines suggest 1,000-2,000 IU daily for adults with low serum levels, after checking blood work. Doses above 4,000 IU should only be taken under medical supervision.
Next Steps for Readers
1. Schedule a review appointment with your asthma physician. Bring this article and a list of the alternatives you’re curious about.
2. Choose one therapy to test for 8 weeks - don’t juggle three new things at once. Track symptoms daily.
3. Re‑evaluate after the trial period. Keep what works, discard what doesn’t, and adjust your plan with professional guidance.
Remember, the goal isn’t to abandon proven medication but to weave a supportive lifestyle that keeps flare‑ups at bay and lets you breathe easier.




Matthew Hall
October 20, 2025 AT 20:40I swear the big pharma cartel wants us glued to inhalers so they can keep their bottom line soaring. Every new "alternative" gets a sneaky label that says "just a supplement" while they hide the real data. It's like they hired a PR firm to tell us that needles and yoga are just trendy fluff. Anyway, if you’re gonna try something, make sure the practitioner isn’t on their payroll.
Kate McKay
October 22, 2025 AT 06:00Hey, you’ve already got the basics down, so why not pick one thing to start with? Try a 5‑minute breathing routine every morning – consistency beats intensity any day. Keep a simple log of how many puffs you use; watching that number drop is pure motivation. And remember, the goal isn’t to ditch your meds, it's to give them a little breathing room.
Kirsten Youtsey
October 23, 2025 AT 15:20One might consider the aforementioned modalities, though evidence remains tenuous.
Rajesh Myadam
October 25, 2025 AT 00:40That table was really helpful – seeing the mechanisms side‑by‑side makes the choices clearer. If you’re nervous about interactions, a quick chat with your pharmacist can save a lot of hassle. Also, keep an eye on how you feel after each new supplement; your body will tell you if it’s working.
Natalie Morgan
October 26, 2025 AT 09:00Curious on how fast the lung function improves with yoga it seems like a few weeks can make a noticeable difference.
Demetri Huyler
October 27, 2025 AT 18:20Honestly, if you’re an American who cares about personal freedom, you should be proud to explore these holistic routes. Our ancestors didn’t rely on synthetic pills – they trusted nature and mindfulness. So go ahead, give that acupuncture a try; just make sure the practitioner knows the difference between a good needle and a political agenda.
Israel Emory
October 29, 2025 AT 03:40Wow-great summary!; I especially love the bit about combining HEPA filters with regular cleaning; it’s a practical step that anyone can take; keep sharing these actionable tips; the community thrives on this kind of positivity!
laura wood
October 30, 2025 AT 13:00Reading through the guide felt like a warm hug for my lungs. The reminder to keep a symptom diary really resonated with me – it’s the simplest way to see progress.
Sebastian Green
October 31, 2025 AT 22:20Totally agree with Kate – consistency is key.
Wesley Humble
November 2, 2025 AT 07:40Allow me to elucidate the underlying pharmacodynamic implications of integrating alternative therapies with conventional asthma management. Firstly, the modulation of the NF‑κB pathway by Boswellia serrata presents a plausible adjunctive anti‑inflammatory effect, yet the magnitude of cytokine attenuation remains modest when juxtaposed with inhaled corticosteroids. Secondly, the psychophysiological benefits conferred by pranayama hinge upon autonomic rebalancing, which can attenuate bronchoconstriction via enhanced vagal tone; however, empirical quantification of these effects is limited to small cohorts with heterogeneous protocols. Thirdly, the purported mast‑cell stabilizing properties of butterbur are theoretically sound, given its inhibition of calcium influx, but the risk of hepatotoxicity mandates rigorous hepatic monitoring. Fourth, vitamin D supplementation's immunomodulatory capacity, particularly the down‑regulation of Th2 cytokines, is supported by meta‑analyses, yet the optimal serum threshold for clinical benefit remains contested. Fifth, probiotics may recalibrate the gut‑lung axis, but strain‑specific efficacy data are still emerging, rendering blanket recommendations premature. Sixth, air purification strategies effectively reduce indoor particulate load, thereby diminishing allergen‑triggered exacerbations, yet the cost‑benefit ratio must be weighed against behavioral interventions such as dust‑mite avoidance. Seventh, the safety profile of acupuncture is acceptable when performed by credentialed practitioners, though the neuroimmune mechanisms hypothesized lack robust validation. Eighth, while yoga and structured breathing exercises can improve diaphragmatic strength, the incremental gain in forced expiratory volume is typically marginal and should not be misconstrued as a substitute for bronchodilator therapy. Ninth, interaction potential between herbal extracts and corticosteroids, especially regarding cytochrome P450 metabolism, necessitates vigilant therapeutic drug monitoring. Tenth, the psychosocial dimension of patient‑empowered self‑management cannot be overstated; adherence improves when patients perceive agency over their treatment plan. Eleventh, a systematic approach involving baseline spirometry, serum 25‑OH‑D assessment, and allergen sensitization profiling provides a quantitative framework for evaluating adjunctive therapy efficacy. Twelfth, clinicians should adopt a shared decision‑making model, integrating patient preferences with evidence‑based recommendations to optimize outcomes. Thirteenth, longitudinal data collection via digital health platforms may facilitate real‑world evidence generation for these complementary modalities. Fourteenth, health policy implications include the need for reimbursement pathways that recognize validated integrative interventions. Finally, it is incumbent upon the medical community to continue rigorous investigation, ensuring that enthusiasm for alternative therapies is tempered by scientific rigor.
Mahesh Upadhyay
November 3, 2025 AT 17:00Look, if you’re not 100% on board with these "natural" fixes, you’re basically endorsing the status quo. The drama of calling them “alternative” is just a marketing ploy.
barnabas jacob
November 5, 2025 AT 02:20Honestly, the pharma‑centric paradigm is a classic case of theyo overextrapolate the data while ignoring real‑world outcomes; you need to scrutinize the clinical endpoints before you subscribe to any so‑called miracle cure.
Deja Scott
November 6, 2025 AT 11:40Great compilation – thanks for pulling together the science and the practical steps. I’ll definitely try the breathing exercises first.