Drug Temperature Risk Calculator
Calculate Temperature Risk
Enter drug type and exposure details to determine effectiveness loss and safety risk.
When you pick up a prescription, you assume the medicine inside is safe, effective, and exactly what your doctor ordered. But what if the path it took to get there was broken? The pharmaceutical supply chain isn’t just about shipping boxes-it’s the invisible line between life and death for millions. A single temperature spike during transport, a counterfeit pill slipped into a batch, or a delayed shipment of insulin can mean the difference between recovery and irreversible harm.
How a Broken Chain Directly Harms Patients
It’s easy to think of drug shortages as an administrative headache. But for patients, it’s personal. In 2023, over 68% of U.S. hospitals reported having to substitute one medication for another due to supply issues. For a diabetic patient, switching insulin brands mid-treatment can cause dangerous blood sugar swings. One Reddit user from Ohio described rationing epinephrine auto-injectors for three straight months because the supply kept running out. That’s not a policy problem-it’s a survival issue.
Then there’s the case of the multiple sclerosis patient whose Tysabri infusions were delayed by 17 days. When she got her next MRI, two new brain lesions showed up. Her doctor confirmed the delay was the likely cause. This isn’t rare. A 2024 American Hospital Association survey found that 29% of hospitals saw direct adverse reactions from last-minute drug substitutions. These aren’t statistical outliers. They’re daily realities in emergency rooms, oncology clinics, and home care settings.
The Technical Demands No One Talks About
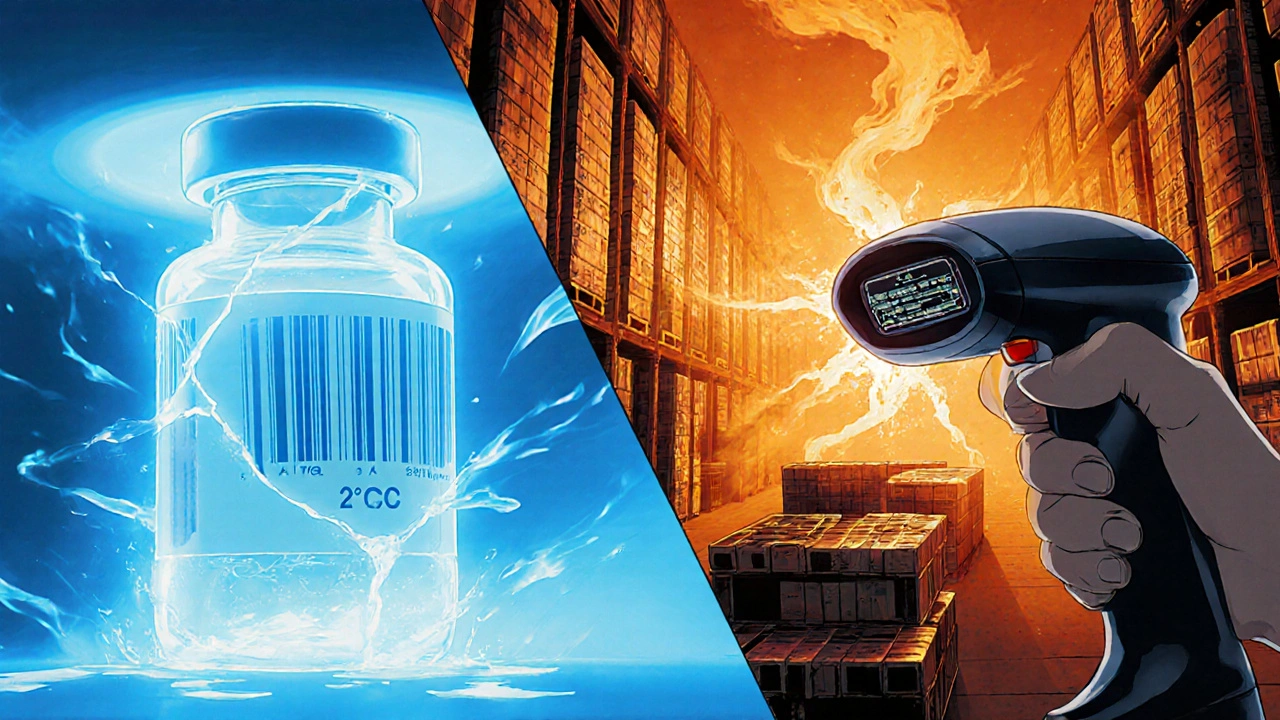
Seventy-two percent of biologic drugs-like cancer treatments, vaccines, and autoimmune therapies-must stay between 2°C and 8°C from factory to fridge. Fifteen percent need to be frozen below -60°C. That’s not a suggestion. That’s a scientific requirement. If a shipment sits in a hot warehouse for four hours, the drug can degrade. The patient gets a pill that looks normal but does nothing. Or worse, it triggers a dangerous immune reaction.
And it’s not just temperature. The FDA’s Drug Supply Chain Security Act (DSCSA), fully enforced since November 2023, requires every prescription drug package to have a unique 2D barcode. This lets pharmacies and distributors trace a pill back to its manufacturer. But 76% of hospitals say integrating this with their old inventory systems is a nightmare. Legacy software doesn’t talk to new scanners. Staff spend hours manually checking barcodes instead of helping patients.
Blockchain is being adopted by big pharma-up 37% since 2020-but it’s expensive. Setting up a full track-and-trace system costs an average of $450,000 per hospital and takes eight months. Small clinics can’t afford it. So while big companies track every vial, millions of pills move through shadow networks with no digital paper trail.
Why the System Is So Fragile
The pharmaceutical supply chain has 3.2 times more regulations than the average consumer goods chain. Yet it carries 47% less inventory. Why? Because most drugs expire in 12 to 36 months. You can’t stockpile them like toilet paper. That leaves zero room for error.
And here’s the kicker: 78% of the world’s active pharmaceutical ingredients (APIs)-the actual chemical ingredients in pills-are made in just two countries: China and India. One flood in Hyderabad, a labor strike in Shanghai, or a trade ban, and the entire global supply of a critical drug can vanish overnight. During the first six months of the pandemic, drug shortages jumped 300%. That wasn’t just bad luck. It was a system designed for efficiency, not resilience.
Emerging economies are hit hardest. Caribbean hospitals have a supply chain pressure index of 8.1-far above the safe target of -0.5. In places like Haiti or Jamaica, delays aren’t measured in days. They’re measured in weeks. Patients miss chemotherapy cycles. Antibiotics run out. Diabetics go without insulin. And there’s no backup.
The Hidden Cost of Cybersecurity Gaps
Most people don’t realize that the supply chain is now a digital battlefield. In 2024, a software failure from CrowdStrike knocked out 759 hospitals across North America. Pharmacies couldn’t print labels. IV pumps stopped working. Patients were turned away. The cause? A third-party vendor’s system got hacked.
Censinet found that 74% of healthcare cybersecurity incidents in 2023 came from suppliers-not the hospitals themselves. A small logistics company with weak firewalls can be the entry point for a ransomware attack that shuts down an entire drug distribution network. And once the system is down, it takes an average of 14.2 days to recover. That’s two weeks without critical meds for cancer patients, transplant recipients, and people on dialysis.
Who’s Fixing It-and What’s Still Missing
Some progress is being made. The FDA now requires full electronic tracing by November 2025. AI-powered demand forecasting is expected to cut shortages by 35% by 2027. Companies like Pfizer have built supply chain protocols rated 4.7 out of 5. But most generic manufacturers? Their guidelines average 3.2 out of 5. That’s a massive gap.
There’s also a training crisis. Supply chain managers need 120+ hours of specialized training just to comply with DSCSA. The PharmChain certification program has trained 8,400 people since 2022-but that’s a drop in the bucket compared to the 30,000 manufacturing sites and 180 countries involved. Most hospitals don’t have a single person fully trained in pharmaceutical logistics.
And while blockchain and AI sound futuristic, they won’t help if the last mile is broken. In rural areas, 32% of deliveries still fail because refrigerated trucks don’t reach them. Or the power goes out, and the cold chain breaks. No technology fixes that if the infrastructure isn’t there.
What Needs to Change Now
Patients shouldn’t have to gamble with their health because of a broken supply chain. Here’s what needs to happen:
- Invest in regional manufacturing hubs to reduce dependence on China and India. Countries like Australia and Canada are starting this-but it’s slow.
- Standardize data systems so every pharmacy, distributor, and hospital speaks the same digital language. No more manual entry. No more incompatible scanners.
- Require minimum inventory buffers for life-saving drugs. If a drug is essential, it shouldn’t be treated like a seasonal fashion item.
- Expand cold chain access in rural and low-income areas. This isn’t luxury-it’s basic healthcare infrastructure.
- Hold third-party vendors accountable with the same security standards as hospitals. If your software can crash a hospital, you need to be regulated like one.
The $1.5 trillion pharmaceutical industry has the money. It has the technology. What it’s missing is the will to prioritize people over profit margins. Right now, the system works fine-until it doesn’t. And when it fails, it’s not a spreadsheet that breaks. It’s a patient’s life.
Can counterfeit drugs really get into the supply chain?
Yes. Despite regulations, counterfeit drugs still enter the supply chain, especially in low-income countries and through unregulated online pharmacies. The WHO estimates that 1 in 10 medical products in developing nations are substandard or falsified. Even in the U.S., the FDA has seized thousands of fake versions of popular drugs like Ozempic and Viagra. Blockchain and serialization help, but they’re not foolproof if the system isn’t monitored at every step.
Why can’t we just stockpile more drugs?
Many drugs, especially biologics and insulin, have short shelf lives-sometimes as little as 12 months. Stockpiling them means risking waste if they expire. Also, storage requires expensive cold chain facilities. A single specialized warehouse costs $2.8 million to build and maintain. For manufacturers, it’s cheaper to make drugs just-in-time. But that leaves no buffer when something goes wrong.
Are generic drugs more likely to have supply issues?
Yes. Generic manufacturers often operate on thin margins and rely on a single factory for a single drug. If that factory has a quality issue, power outage, or regulatory shutdown, the entire U.S. supply can vanish overnight. Brand-name drugs usually have multiple production sites and bigger reserves. That’s why shortages hit generics hardest-like the 2023 epinephrine crisis that affected hundreds of hospitals.
How do temperature excursions affect drug effectiveness?
Even a brief exposure to heat or cold can break down the molecular structure of biologics. Insulin can clump. Vaccines can lose potency. Cancer drugs can become toxic. Real-time monitoring shows that 42% fewer temperature excursions occur when sensors are used-but 32% of rural deliveries still lack them. A drug that looks fine might be 80% less effective. Patients won’t know until it’s too late.
What can patients do to protect themselves?
Ask your pharmacist: Is this the same brand or a substitute? If it’s a new version, ask if it’s been approved for your condition. Keep track of your medication schedule-if refills are delayed, report it to your doctor and the FDA’s MedWatch program. For critical drugs like insulin or epinephrine, consider keeping a small backup supply if legally allowed. And always report unusual side effects after a switch in medication-it could help catch a supply chain problem before it harms others.






Noah Fitzsimmons
November 20, 2025 AT 06:58Oh wow, another ‘pharma is broken’ rant. Congrats, you noticed the supply chain isn’t perfect. Newsflash: it’s never been perfect. The real issue? You people think $200 insulin should be free because ‘life is precious.’ Meanwhile, the same people who scream about shortages are the ones who won’t pay for generics or buy from Canada. You want reliability? Pay for it. Stop pretending this is a moral crisis when it’s just economics with a stethoscope.
And don’t get me started on blockchain. You think a fancy QR code fixes a truck that doesn’t have AC in rural Alabama? Wake up. The problem isn’t tech-it’s your refusal to accept that medicine isn’t Amazon Prime.
Eliza Oakes
November 22, 2025 AT 06:38Okay but have y’all seen the *actual* data on counterfeit drugs? The WHO says 1 in 10 in developing nations-but in the US? It’s like 0.001%. Yet everyone’s acting like we’re all about to die from fake Ozempic bought off Instagram. It’s like panic-buying toilet paper but for pills.
And who’s the genius who decided we need a 2D barcode on every single pill? Who’s gonna scan that when you’re in a hospice bed with your hand shaking? This isn’t security-it’s bureaucratic theater. They’re not protecting patients. They’re protecting liability.
Also, ‘regional manufacturing hubs’? Cool. Let’s just rebuild the entire pharmaceutical industry because China got a flood. Meanwhile, my grandma’s blood pressure med is still $3 at Walmart. Don’t fix what ain’t broke, unless you’re trying to make it more expensive.
Clifford Temple
November 22, 2025 AT 15:00Let’s cut the BS. This whole article reads like a UN report written by a grad student who’s never left a CVS. China and India make 78% of APIs? Good. That means we’re not wasting our tax dollars on overpriced domestic production. We outsource the dirty work to people who actually know how to make chemicals. You want ‘resilience’? Then stop whining and start investing in our own military-grade cold chain logistics. Not ‘regional hubs’-real infrastructure.
And why is no one talking about the fact that the FDA approves 90% of generic drugs from factories that haven’t been inspected since 2015? That’s the real scandal. Not blockchain. Not barcodes. It’s regulatory capture by Big Pharma and their lobbyists who want to scare you into paying more for the same damn pills.
Stop blaming the supply chain. Start blaming the regulators who sleep through inspections while CEOs take vacations in the Hamptons.
Corra Hathaway
November 24, 2025 AT 10:35Okay but can we just take a second to appreciate how insane it is that a person’s life hinges on a *temperature sensor*? 🤯
I work in a rural clinic and we had a shipment of insulin arrive at 18°C last winter. The truck driver didn’t even know it was supposed to be cold. We had to put it in the fridge for 48 hours and pray. No alarms. No alerts. Just… hope.
But here’s the good news: people are waking up. Nurses are demanding better. Pharmacies are pushing back. And yeah, the tech is expensive-but we’ve got to start somewhere. I’m not asking for perfection. I’m asking for *basic dignity*. Your grandma shouldn’t have to ration epinephrine like it’s gold.
Also, if you think this is ‘just logistics,’ you’ve never held someone’s hand while they’re waiting for a life-saving drug that’s stuck in a warehouse 300 miles away. 💙
Paula Jane Butterfield
November 25, 2025 AT 20:32hi everyone! just wanted to share something i learned from a friend who works in pharma logistics in india-did you know that in some parts of rural india, they use *ice packs wrapped in cloth* to keep vaccines cold during motorcycle deliveries? no refrigerated trucks, no sensors, just ingenuity and grit. it’s not ideal, but it works.
and honestly? we’re all so focused on tech and blockchain and barcodes, but the real hero is the person who drives 4 hours through a monsoon to deliver insulin to a diabetic kid. no one’s talking about them. no one’s paying them enough. no one’s training them.
maybe the fix isn’t more tech-it’s more *people*. more respect. more investment in the human chain, not just the digital one. also, typo: ‘pharmachain’ should be ‘pharmachain’ 😅
Simone Wood
November 27, 2025 AT 05:04Let’s be brutally honest: the entire supply chain is a regulatory farce. DSCSA? A 14-year-long bureaucratic ballet that costs billions and delivers zero patient outcomes. The FDA’s ‘electronic tracing’ mandate by 2025? A gimmick. The system still relies on manual reconciliation because nobody wants to upgrade their 2007 ERP software.
And don’t get me started on ‘biologics.’ They’re not magic. They’re proteins. Proteins degrade. That’s science. But we’ve turned them into sacred relics, requiring $2.8M warehouses and a PhD to handle them. Meanwhile, aspirin is shipped like potatoes. Double standards.
Real solution? Simplify. Standardize. Deregulate the non-critical stuff. Let the market optimize. Stop pretending this is a humanitarian crisis-it’s a cost-recovery problem dressed in lab coats.
Swati Jain
November 28, 2025 AT 16:55As someone who works in API manufacturing in India, I’ve seen this from the other side. Yes, we make 78% of the world’s raw ingredients. But we’re not the villains. We’re the ones getting slapped with export bans, sudden FDA shutdowns, and price caps while Western companies pocket 80% of the profit.
And yes, we have floods. We have strikes. We have power outages. But guess what? We still ship. We still deliver. We don’t have $450K to install blockchain. We have 3 workers, a fridge, and a prayer.
Stop blaming us. Start paying us fairly. Stop demanding ‘zero tolerance’ when you’re the ones who pay $0.02 per pill and expect miracles. The real failure? The profit-driven model that treats human lives like inventory units.
Also-blockchain won’t fix a broken wage system. 😊
Florian Moser
November 30, 2025 AT 10:43There’s a lot of noise here, but the core issue is simple: we treat pharmaceutical logistics like it’s optional. It’s not. It’s as critical as water treatment or power grids. We don’t let power companies skip inspections because they’re ‘too expensive.’ Why do we let drug distributors do it?
Here’s what actually works: mandatory training for every warehouse worker handling biologics. Real-time temperature logging with automatic alerts. Minimum stock buffers for Tier-1 essential drugs. And accountability-no more ‘third-party vendor’ loopholes.
It’s not about ideology. It’s about systems. And systems can be fixed. We just need the will to fund them. The tech exists. The data exists. What’s missing is the political courage to say: ‘No more excuses.’
jim cerqua
December 1, 2025 AT 14:22Let me tell you about the time I watched a cancer patient cry because her chemo was delayed by 11 days because a warehouse in New Jersey lost power for 7 hours. No backup generators. No alerts. Just silence.
And now? Now we’re arguing about blockchain? About barcodes? About ‘regional hubs’? No. The problem isn’t the chain. It’s the people who treat it like a spreadsheet. The CEOs who get bonuses for ‘efficiency.’ The regulators who inspect factories once every five years. The politicians who cut Medicaid funding but tweet about ‘cancer research.’
This isn’t a supply chain failure. It’s a moral failure. And it’s not going to be fixed by tech. It’s going to be fixed when someone in a suit loses their job over it. Until then? Patients keep dying. Quietly. Alone. And no one’s watching.
So go ahead. Write another article. I’ll be here. Waiting for the next one.
Donald Frantz
December 2, 2025 AT 05:09One thing everyone’s ignoring: the real bottleneck isn’t manufacturing or temperature control-it’s distribution. We have the tech. We have the capital. But we don’t have the workforce. There are 180 countries involved, 30,000 sites, and fewer than 10,000 certified pharmaceutical logisticians. That’s 3 per site on average. Most sites have zero.
Blockchain won’t help if the person scanning the barcode doesn’t know what ‘2–8°C’ means. AI forecasting won’t help if the warehouse manager doesn’t know how to interpret a spike in demand.
Fix the training. Fix the certification. Fix the pay. Everything else follows. The system isn’t broken-it’s understaffed and undertrained. And that’s fixable. With investment. With urgency. With respect.