Nonalcoholic fatty liver disease (NAFLD), now more accurately called metabolic dysfunction-associated steatotic liver disease (MASLD), affects about one in three adults worldwide. It’s not caused by alcohol. It’s caused by what you eat, how much you weigh, and the state of your gut. The liver becomes clogged with fat-not from drinking, but from sugar, refined carbs, and a broken gut microbiome. The good news? This isn’t permanent. Diet and weight loss can reverse it. And the gut is the missing piece most people overlook.
The Gut-Liver Connection You Can’t Ignore
Your gut and liver are connected by a direct highway: the portal vein. Every time you eat, what happens in your intestines doesn’t stay there. Bacteria in your gut produce toxins, metabolites, and signals that travel straight to your liver. In healthy people, the gut lining acts like a wall-keeping bad stuff out. In NAFLD, that wall cracks. Studies show 90% of people with fatty liver have a leaky gut. That means endotoxins like LPS (lipopolysaccharide) slip through, triggering liver inflammation. People with NAFLD have 2.3 times more of these toxins in their blood than healthy people. The gut microbiome in NAFLD patients looks different. It’s less diverse. Some helpful bacteria like Bacteroides vulgatus are missing. Harmful ones like Lachnospiraceae and Barnesiella intestinihominis are overgrown. And the good stuff-short-chain fatty acids like butyrate-plummets by 58%. Butyrate feeds the cells lining your gut. Without it, the wall breaks down even faster. This isn’t just correlation. It’s cause and effect.Diet Is the First Line of Defense
You can’t out-exercise a bad diet. But you can out-eat NAFLD. The goal isn’t just to lose weight-it’s to reset your gut. The Mediterranean diet isn’t just trendy. It’s backed by hard data. In a 6-month trial with 70 NAFLD patients, eating a Mediterranean diet with 30 grams of walnuts daily cut liver fat by 32%. Why? Walnuts are packed with fiber and polyphenols that feed good bacteria. Olive oil reduces inflammation. Vegetables and legumes boost fiber intake. And crucially, this diet cuts fructose-your gut’s worst enemy. Fructose, especially from soda, juice, and processed snacks, is metabolized almost entirely by the liver. It turns straight into fat. Studies show people who consume more than 25 grams of fructose a day have higher liver fat and worse gut permeability. That’s less than one can of soda. Cut it out, and you cut a major driver of the disease. Fiber matters too. Aim for 25-30 grams daily. Whole grains, lentils, broccoli, apples, and flaxseeds are your allies. Fiber doesn’t just help digestion-it feeds the bacteria that make butyrate. Higher fiber intake is linked to lower liver stiffness, a sign of less scarring. One study found that 10 grams of inulin (a prebiotic fiber) daily for 12 weeks increased butyrate by 47% and reduced liver stiffness by 15%.Weight Loss Isn’t Optional-It’s the Cure
Losing weight isn’t about looks. It’s about survival. If you have NAFLD, losing just 5-7% of your body weight improves liver fat in 81% of people. Lose 10%, and nearly half of those with the more serious form-NASH-see it resolve completely. These aren’t guesses. They’re results from a 2023 meta-analysis of over 12,000 patients. The trick? Lose it slowly. Aim for 0.5-1 kg per week. Crash diets backfire. They stress the liver, worsen inflammation, and make you more likely to regain weight. A daily calorie deficit of 500-750 kcal works best. Combine it with movement. Walking 30 minutes a day, strength training twice a week-these aren’t just helpful. They’re necessary. People who combine diet and exercise reduce liver enzymes (ALT) by 28 units, while those who only diet drop it by 15. That’s a big difference when your liver is already struggling. Real people succeed with structured programs. At the Mayo Clinic, patients who followed a 12-month plan with diet, exercise, and behavioral coaching kept 68% of their weight off after two years. Those who tried on their own? Only 29% kept it off. Support matters. Tracking food. Setting small goals. Finding non-food rewards. These aren’t fluffy tips-they’re what separates long-term success from temporary loss.Probiotics and Prebiotics: Helpful, But Not Magic
Probiotics aren’t a cure. But they’re a powerful tool. A double-blind trial with 100 NAFLD patients showed that taking a daily mix of Lactobacillus rhamnosus GG, Bifidobacterium longum, and Streptococcus thermophilus for 24 weeks reduced liver fat by 23% and lowered ALT by 31%. That’s comparable to some medications. The key? Strain specificity and dose. You need at least 10^9 CFU per day, and multiple strains. Single-strain supplements? Usually useless. Prebiotics are even simpler. Eat more fiber. That’s it. Inulin, resistant starch (from cooled potatoes or rice), and oats feed the good bugs. One study found that 8 grams of fructo-oligosaccharides daily for 12 weeks boosted butyrate and lowered liver stiffness. No pills needed. Just food. Fecal transplants? Still experimental. Early trials show minor improvements in liver enzymes, but no real change in liver tissue. Not ready for prime time. Stick to diet and proven probiotics.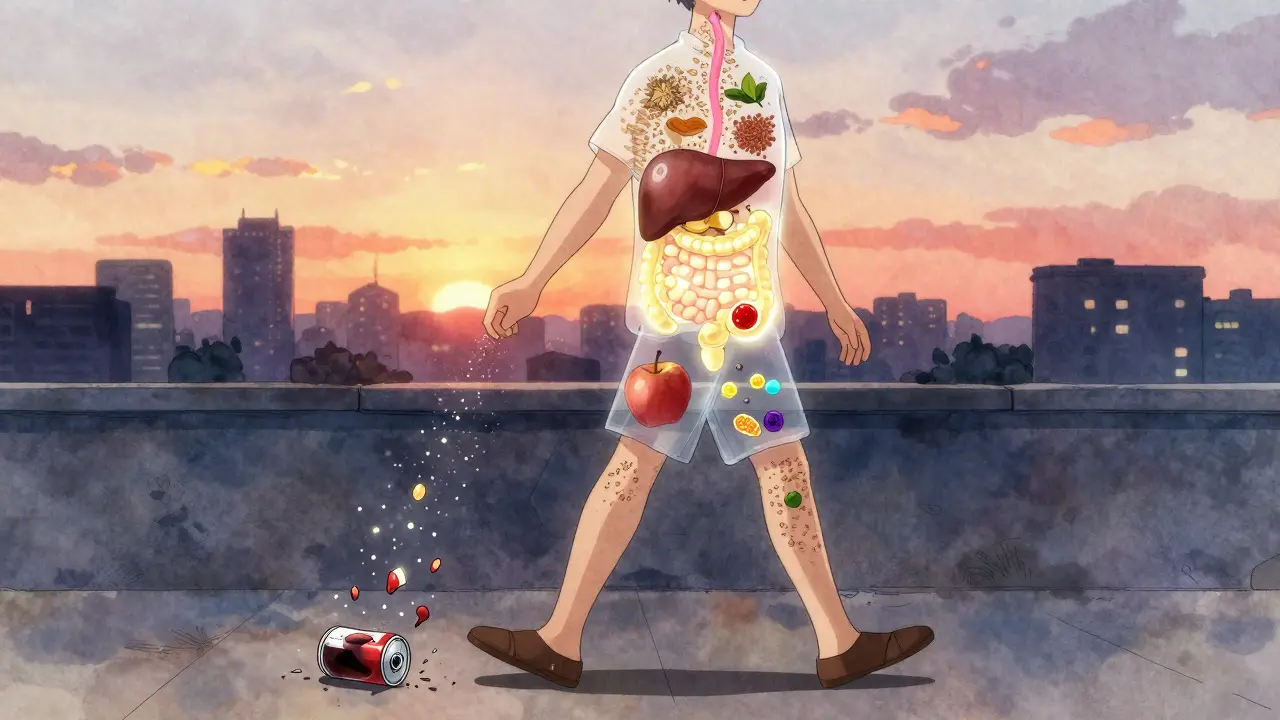
What Not to Do
Don’t fall for quick fixes. Detox teas, liver cleanses, and miracle supplements? They don’t touch the root causes. They’re marketing. The FDA hasn’t approved any drug for NAFLD yet. The only proven treatments are weight loss and diet change. Avoid artificial sweeteners. They may seem safe, but studies link them to gut dysbiosis and increased glucose intolerance-both bad for fatty liver. Same with ultra-processed foods. They’re loaded with hidden sugars, unhealthy fats, and additives that damage your gut lining. Don’t skip meals to lose weight. That slows your metabolism, increases hunger, and makes you binge later. Eat regularly. Focus on protein and fiber at every meal to stay full longer.Real-Life Success: What Works for People
In online communities like Reddit’s r/NAFLD, thousands share their stories. The most common success story? The Mediterranean diet with intermittent fasting. The 5:2 method-eating normally five days, cutting calories to 500-600 on two non-consecutive days-helped 63% of users report less fatigue and bloating within weeks. One man in Melbourne lost 14% of his body weight in 8 months by swapping sugary breakfasts for eggs and avocado, cutting soda, and walking after dinner. His liver enzymes dropped from 120 to 38. But it’s not easy. Forty-one percent of people say social events and cravings are their biggest hurdles. That’s normal. You don’t have to be perfect. One bad meal won’t undo progress. Consistency over perfection is the rule.What’s Next?
The field is moving fast. New drugs targeting the gut-liver axis are in phase 3 trials. One, called VE-117, is a precise mix of bacteria designed to activate FXR-a receptor that reduces liver fat by 38% in early results. But even if these drugs come to market, they’ll work best alongside diet and weight loss. The naming shift from NAFLD to MASLD in January 2024 wasn’t just semantics. It reflects a deeper understanding: this is a metabolic disease. The liver is just the symptom. The real problem is in the gut, the diet, and the body’s energy balance.
Simple Steps to Start Today
- Replace sugary drinks with water, herbal tea, or sparkling water with lemon.
- Add one serving of vegetables to every meal-broccoli, spinach, carrots, kale.
- Swap white bread and rice for whole grains: oats, quinoa, brown rice.
- Include healthy fats: olive oil, avocado, nuts (especially walnuts).
- Walk 30 minutes after dinner, five days a week.
- Try a daily probiotic with at least 10 billion CFU and multiple strains (L. rhamnosus, B. longum).
- Track your weight weekly. Aim for 0.5-1 kg loss per week.
FAQ
Can NAFLD be reversed without losing weight?
No. Weight loss is the only proven way to reverse fatty liver disease. Even small losses-5-7% of body weight-improve liver fat in most people. Without losing weight, dietary changes alone may slow progression but won’t fully reverse the condition. The liver needs to burn off excess fat, and that only happens when you create a sustained calorie deficit.
How long does it take to see improvements in fatty liver?
You can see changes in liver enzymes and gut symptoms within 4-8 weeks of starting a healthy diet and losing weight. Liver fat reduction is measurable by ultrasound or MRI after 3-6 months. For NASH (inflammation), it takes longer-often 6-12 months of consistent lifestyle change. The key is persistence. Early improvements in energy and digestion are good signs your body is healing.
Are probiotics worth taking for NAFLD?
Yes-if you choose the right ones. Not all probiotics work. Look for multi-strain formulas with at least 10^9 CFU per day, including Lactobacillus rhamnosus GG and Bifidobacterium longum. Clinical trials show these strains reduce liver fat and inflammation. But they’re not a substitute for diet and weight loss. Think of them as a support tool, not a cure.
Does intermittent fasting help NAFLD?
Yes, especially the 5:2 method or 14:10 time-restricted eating. Fasting reduces insulin levels, which helps the liver burn fat. It also gives your gut a break, improving barrier function. Studies show intermittent fasting reduces liver fat by up to 30% in 3 months. But it’s not for everyone. If you have diabetes, low blood pressure, or a history of eating disorders, talk to your doctor first.
What foods should I avoid with NAFLD?
Avoid added sugars (especially fructose in soda, juice, candy), refined carbs (white bread, pastries), trans fats (fried foods, margarine), and ultra-processed snacks. Limit alcohol-even small amounts can worsen liver damage. Artificial sweeteners like aspartame and sucralose may disrupt gut bacteria and should be minimized. Focus on whole, unprocessed foods instead.
Is NAFLD the same as alcoholic liver disease?
No. Alcoholic liver disease is caused by heavy drinking. NAFLD (now MASLD) happens in people who drink little to no alcohol. Both can look similar on a scan, but the causes are completely different. You can have NAFLD even if you’ve never had a drink. The treatment is also different-alcohol abstinence is the only fix for alcoholic liver disease, while NAFLD responds to diet, weight loss, and gut health.





Hayley Ash
December 31, 2025 AT 01:14Also 'MASLD'? Really? So now we're rebranding because 'fatty liver' sounds too gross? Congrats, you just invented corporate wellness jargon.
kelly tracy
January 1, 2026 AT 10:23Joseph Corry
January 3, 2026 AT 03:26And yet - the very notion of 'reversal' implies a teleological arc toward health, which presupposes a normative conception of bodily integrity that may itself be a social construct. The gut-liver axis, then, is not merely anatomical - it is hermeneutic.
Colin L
January 3, 2026 AT 14:40srishti Jain
January 4, 2026 AT 21:02Cheyenne Sims
January 5, 2026 AT 19:22Shae Chapman
January 7, 2026 AT 14:10Nadia Spira
January 8, 2026 AT 01:04henry mateo
January 8, 2026 AT 13:30Kunal Karakoti
January 9, 2026 AT 08:45