Not every bad reaction to a pill or injection is an allergy. In fact, most aren’t. But when it is an allergic reaction, it can turn dangerous fast. You might get a rash after taking amoxicillin, or feel your throat swell after an IV antibiotic. These aren’t just side effects-they’re your immune system sounding the alarm. And if you don’t know the difference, you could miss a life-threatening emergency or carry a misdiagnosis for years.
What Actually Counts as a Drug Allergy?
A true drug allergy happens when your immune system mistakes a medication for a threat and attacks it. This isn’t the same as nausea from antibiotics or dizziness from blood pressure pills. Those are side effects-expected, common, and not immune-driven. Allergies are rare, but they’re unpredictable. One person gets hives from penicillin; another takes the same drug with no issue. That’s why labeling yourself allergic without proper testing can be dangerous.According to the National Institutes of Health, about 10% of Americans say they’re allergic to a drug. But studies show more than 90% of those who think they’re allergic to penicillin aren’t. That’s not just a personal inconvenience-it affects your treatment options, increases your risk of infections like C. diff, and drives up healthcare costs. Mislabeling isn’t harmless. It’s a public health blind spot.
Common Signs of a Drug Allergy
Symptoms vary by how your body reacts. Some show up fast. Others creep in over days. Here’s what to watch for:- Skin rash - The most common sign. Can be red, flat spots or raised bumps. Often itchy.
- Hives - Raised, red, itchy welts that come and go. They may look like mosquito bites but spread quickly.
- Swelling - Lips, tongue, eyelids, or throat. This is a red flag. Swelling in the throat can block your airway.
- Itching - Even without a visible rash, intense itching can signal an allergic response.
- Difficulty breathing - Wheezing, tight chest, or shortness of breath. This isn’t just a cold.
- Gastrointestinal issues - Vomiting, diarrhea, or abdominal cramps-especially when paired with skin or breathing symptoms.
These symptoms can appear within minutes of taking the drug-or they can take days, even weeks. That’s why it’s easy to miss the connection. You might think your rash came from laundry detergent, not the new painkiller you started three days ago.
When It Gets Serious: Anaphylaxis and Other Life-Threatening Reactions
Anaphylaxis is the most dangerous drug allergy reaction. It hits fast-usually within an hour-and affects two or more body systems at once. For example: a rash and trouble breathing, or swelling and vomiting. It can lead to a sudden drop in blood pressure, loss of consciousness, or cardiac arrest.Don’t wait. If you or someone else has:
- Difficulty breathing or wheezing
- Swelling of the tongue or throat
- Dizziness or fainting
- Rapid pulse or cold, clammy skin
Call 911 immediately. Don’t try to drive yourself. Use an epinephrine auto-injector if you have one. Emergency responders need to act fast-every minute counts.
Other severe reactions include:
- Stevens-Johnson Syndrome (SJS) / Toxic Epidermal Necrolysis (TEN) - Starts like a flu, then the skin blisters and peels off in sheets. Mucous membranes in the mouth, eyes, and genitals are often involved. This is a hospital emergency.
- DRESS syndrome - Rash, fever, swollen lymph nodes, and liver damage. Symptoms can appear weeks after starting the drug and may flare up again even after stopping it.
- Serum sickness-like reaction - Rash, joint pain, fever, and swollen glands appearing one to three weeks after taking the drug.
These aren’t common-but when they happen, they require urgent care. Don’t dismiss a fever or joint pain after starting a new medication. Link it back to the drug.
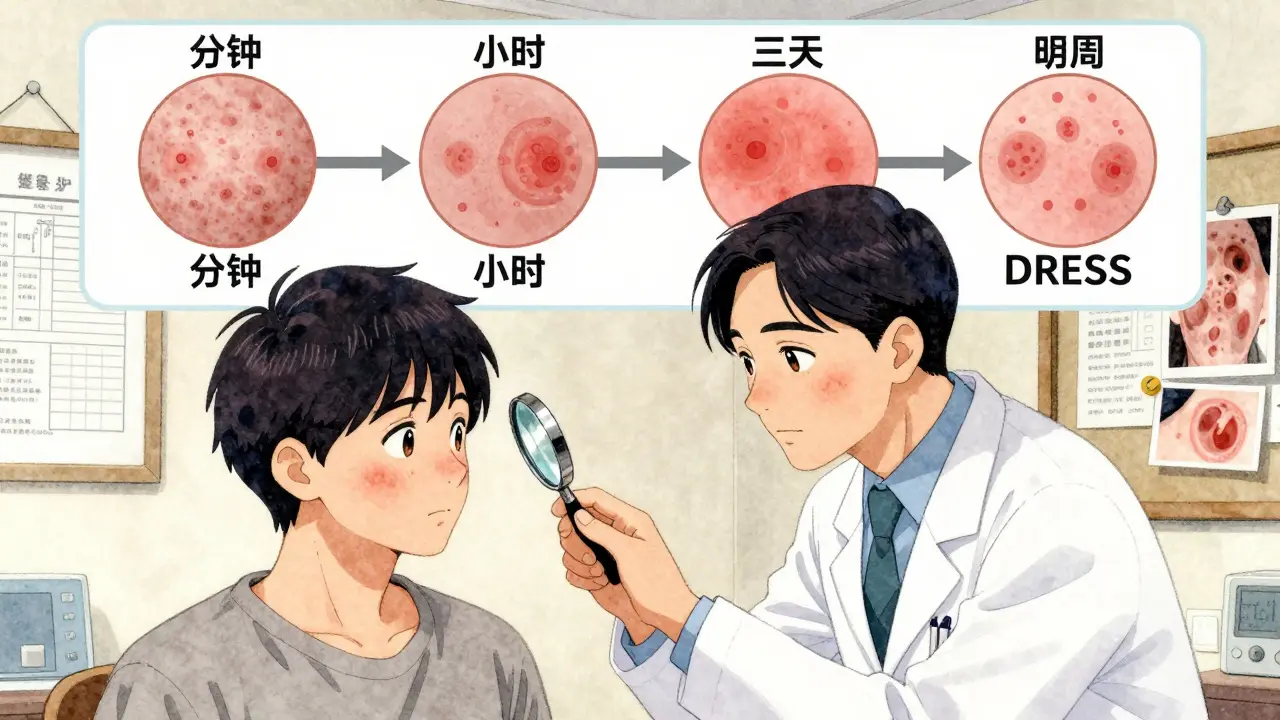
Timing Matters: How Soon After Taking the Drug Do Symptoms Appear?
The clock tells you a lot about what kind of reaction you’re dealing with.- Immediate (minutes to 1 hour) - Classic IgE-mediated allergy. Think hives, swelling, anaphylaxis. Penicillin, sulfa drugs, and some anesthetics often trigger this.
- Delayed (1 to 6 hours) - Still immune-driven, but slower. May include vomiting, diarrhea, or low blood pressure alongside skin symptoms.
- Days later (2-14 days) - Drug rash (exanthem). Often looks like measles. Doesn’t usually mean anaphylaxis risk, but still needs evaluation.
- Weeks later (1-3 weeks) - Serum sickness or DRESS. Fever and joint pain show up after you’ve stopped the drug. This is easy to miss because you don’t connect it to something you took days ago.
If you get a rash three days after starting a new antibiotic, don’t assume it’s harmless. Track it. Take a photo. Note the timing. That info helps your doctor decide if it’s a true allergy or just a side effect.
What to Do If You Suspect a Drug Allergy
If you think you’re having a reaction, stop the drug-but don’t throw out the bottle. Bring it with you to your doctor. Here’s what to do next:- Call your doctor for non-emergency symptoms like a mild rash or itching. They’ll ask for details: What drug? When did you start it? What exactly happened? When did symptoms begin?
- Take pictures - Skin changes fade fast. A photo helps your doctor see what you saw.
- Don’t self-diagnose - Just because you had a rash once doesn’t mean you’re allergic forever. Many people outgrow drug allergies or were misdiagnosed.
- See an allergist - Especially if you’ve had a serious reaction. They’re the only ones trained to test for drug allergies properly.
For penicillin, there’s a reliable test: skin prick tests followed by an oral challenge under medical supervision. If those are negative, you’re not allergic. That opens up safer, cheaper, more effective treatment options.
For other drugs? Testing is limited. But a detailed history and careful evaluation can still rule out allergies in many cases. Blood tests can help for severe delayed reactions like DRESS.

Why Getting Tested Matters
If you’re labeled allergic to penicillin but you’re not, you might be given a different antibiotic-like vancomycin or clindamycin. These are broader-spectrum. They kill more bacteria, good and bad. That raises your risk of dangerous infections like C. diff. They’re also more expensive and sometimes less effective.Studies show that over 90% of people who think they’re allergic to penicillin can safely take it after proper testing. That’s not a small number. That’s millions of people unnecessarily avoiding one of the safest, most effective antibiotics we have.
And it’s not just penicillin. Mislabeling affects how you’re treated for infections, surgeries, and chronic conditions. One wrong label can ripple through your entire medical history.
What Happens After Diagnosis?
If you’re confirmed allergic to a drug, you’ll get a medical alert bracelet or note in your chart. You’ll also get a plan:- Which drugs to avoid
- Safe alternatives
- What to do if you accidentally take it
- When to carry epinephrine
If you’re cleared of an allergy? That’s even better. You get back access to better, safer, cheaper treatments. You stop carrying a label that doesn’t fit you.
Final Thought: Don’t Guess. Get Checked.
A rash after a pill doesn’t automatically mean you’re allergic. A bad reaction doesn’t mean you’ll never take that drug again. The truth is hidden in details-timing, symptoms, and medical history. If you’ve ever had a reaction, don’t just assume. Talk to a doctor. See an allergist. Get tested.Your next prescription could depend on it.
How do I know if my rash is from a drug allergy or just a side effect?
A side effect is predictable and doesn’t involve your immune system-like nausea from antibiotics. A drug allergy triggers an immune response and often includes symptoms like hives, swelling, or trouble breathing. If you have a rash plus other symptoms like fever, joint pain, or swelling, it’s more likely an allergy. Timing matters too: side effects usually happen right away; allergic rashes can take days to appear. Always get it checked by a doctor.
Can I outgrow a drug allergy?
Yes, especially with penicillin. Many people who had a reaction as a child lose their sensitivity over time. Studies show up to 80% of people who were labeled penicillin-allergic as kids are no longer allergic after 10 years. That’s why testing is so important-you might be able to safely take the drug again.
Is there a blood test for drug allergies?
For most drugs, no reliable blood test exists. The exception is for severe delayed reactions like DRESS syndrome, where a blood test can show elevated eosinophils or liver enzymes. Skin testing is the gold standard for penicillin. For other drugs, doctors rely on your medical history and sometimes a controlled drug challenge under supervision.
Can I take a different antibiotic if I’m allergic to penicillin?
You can-but not always safely. Many alternatives are broader-spectrum, which increases your risk of infections like C. diff. They’re also more expensive and sometimes less effective. If you’re labeled penicillin-allergic, get tested. If you’re not truly allergic, you can use penicillin or related drugs like amoxicillin, which are safer and more targeted.
What should I do if I have a reaction but can’t see a doctor right away?
Take clear photos of any rash, swelling, or skin changes. Write down the name of the drug, when you took it, and when symptoms started. Avoid taking the drug again. If symptoms are mild (like a rash or itching), call your doctor the same day. If you have trouble breathing, swelling of the throat, dizziness, or feel faint-call 911 immediately. Don’t wait.
Are drug allergies more common in certain people?
Some people are at higher risk, like those with a history of other allergies (like hay fever or food allergies), or those who’ve had a reaction before. Certain drugs are more likely to trigger allergies-penicillin, sulfa drugs, NSAIDs, and some seizure medications. But anyone can develop a drug allergy at any time, even if they’ve taken the drug safely for years.
Can I be allergic to a drug I’ve taken before without problems?
Yes. Allergies can develop after repeated exposure. Your immune system can suddenly start recognizing a drug as a threat-even if you’ve taken it 10 times before with no issue. That’s why you should never assume safety based on past use. Always pay attention to new symptoms.
Is it safe to take a drug if I’m allergic to a similar one?
Sometimes, but never assume. For example, if you’re allergic to penicillin, you might still be able to take cephalosporins-but not always. Cross-reactivity varies. Only an allergist can determine if it’s safe based on your history and testing. Never try it on your own.






Michael Patterson
January 10, 2026 AT 14:54man i thought i was allergic to penicillin after that one rash back in 2018 but turns out it was just the laundry detergent i switched to lol. i kept avoiding all antibiotics for years until my doc finally pushed me to get tested. turns out i was fine. now i take amoxicillin like it's candy. why do people just assume they're allergic? it's insane how many of us are carrying around fake medical labels like they're trophies.
Priscilla Kraft
January 12, 2026 AT 10:59so glad this post exists 🙏 i had a friend who avoided all beta-lactams for 15 years because of a childhood rash-turned out she could’ve had normal pneumonia treatment instead of vancomycin. now she’s healthier, saved $$$, and doesn’t have to stress about every doctor’s visit. testing is a gift. please get tested if you’ve ever had a reaction. your future self will thank you 💙
Christian Basel
January 13, 2026 AT 09:03the immunoglobulin e-mediated hypersensitivity response is grossly overdiagnosed in primary care settings. most clinicians lack the training to differentiate between idiosyncratic drug reactions and true IgE-mediated anaphylaxis. this leads to unnecessary avoidance of first-line agents, increased antimicrobial resistance, and higher healthcare expenditures. the data is clear but the system is broken.
Adewumi Gbotemi
January 14, 2026 AT 00:41i’m from nigeria and here people just stop taking medicine when they feel funny. no testing, no follow-up. i had a cousin who got a rash from co-trimoxazole and now she won’t take any antibiotic. she got sick again last month and almost died because she refused to go to the hospital. this info needs to spread everywhere.
Jennifer Littler
January 15, 2026 AT 22:49the part about DRESS syndrome scared me. i had a fever and joint pain after taking allopurinol last year. my doctor called it "viral" and moved on. now i’m wondering if i missed something serious. maybe i should get bloodwork done? i don’t want to be one of those people who thinks it’s "just a bug" until it’s too late.
Vincent Clarizio
January 17, 2026 AT 15:54oh wow. so we’re supposed to believe that 90% of people who think they’re allergic to penicillin are wrong? that’s like saying 9 out of 10 people who think they’re gluten intolerant are just eating too much bread. i mean, sure, maybe. but how do you prove a negative? what if your immune system just decided to flip the switch one day? this feels like medical gaslighting dressed up as science.
Sam Davies
January 18, 2026 AT 22:52so let me get this straight. you’re telling me i can stop being "allergic" to penicillin just by walking into an allergist’s office and letting them poke me with a needle? and then i get to go back to using the cheap, effective drug instead of the expensive, toxic one? wow. so much for the pharmaceutical industry’s profit margins. who knew truth was so inconvenient?
Alex Smith
January 19, 2026 AT 10:25funny how we’ll trust a stranger’s opinion on TikTok about "detoxing" but won’t get a simple skin test for something that could save our lives. the fact that we’re still treating drug allergies like superstition instead of science is wild. maybe if doctors spent less time writing scripts and more time asking "when did this start?" we’d be better off.
Priya Patel
January 20, 2026 AT 19:52my mom had a rash after amoxicillin when i was a kid. she never took it again. now she’s 72 and just got tested last year-turns out she’s fine! she cried. said she spent 50 years scared of her own body. this is the kind of info that changes lives. thank you for sharing 💕
Sean Feng
January 22, 2026 AT 10:11stop overcomplicating this if you get a rash stop taking the pill
Roshan Joy
January 23, 2026 AT 07:08in india we don’t have easy access to allergists but i’ve seen so many people avoid penicillin because their uncle got a rash once. i always tell them: take a pic, write down the date, and ask a pharmacist. if it’s more than just a rash, don’t guess. find a way to get checked. your life might depend on it.
Matthew Miller
January 24, 2026 AT 12:21you people are ridiculous. you think a doctor’s opinion matters? the system is designed to keep you scared and dependent. penicillin is cheap, sure-but so are the lawsuits. they’d rather you take vancomycin and pay $2000 than risk a malpractice suit from someone who "thought" they were allergic. this whole post is corporate propaganda wrapped in a lab coat.
Madhav Malhotra
January 24, 2026 AT 21:37i remember in my village in india, people used to say "if it burns, it’s poison"-so they’d stop any medicine that made them feel weird. now i’m studying medicine and realize how many lives we lost because no one knew the difference between side effects and real allergies. this article? it’s a lifeline. thank you.
Jason Shriner
January 26, 2026 AT 07:01so let me get this straight… i’m supposed to trust a doctor who’s never even met me before to tell me whether my body’s lying to me? what if my immune system is just… sensitive? what if it’s not about penicillin at all but about the way modern medicine has poisoned our microbiomes? maybe the real allergy is to industrial pharmaceuticals. maybe we’re allergic to capitalism.
Alfred Schmidt
January 26, 2026 AT 18:41THIS IS WHY PEOPLE DIE. YOU THINK A RASH IS "MILD"? YOU THINK "I’LL JUST WAIT AND SEE" IS OKAY? I LOST MY BROTHER TO ANAPHYLAXIS BECAUSE HE DIDN’T KNOW THE DIFFERENCE BETWEEN A SIDE EFFECT AND A DEATH SENTENCE. IF YOU’RE NOT TAKING THIS SERIOUSLY, YOU’RE NOT JUST IGNORANT-YOU’RE DANGEROUS.