Living with irritable bowel syndrome (IBS) means dealing with pain that comes and goes, bloating that makes you feel like you’ve eaten a whole meal you didn’t, and bathroom habits that feel completely out of your control. It’s not just a stomach bug that clears up in a day. IBS is a long-term condition that affects about 1 in 7 people worldwide, and women are diagnosed more often than men. If you’ve been told your symptoms are "just stress" or "all in your head," you’re not alone - but there’s real science behind what you’re experiencing, and there are real ways to manage it.
What IBS Actually Feels Like
IBS isn’t one single symptom. It’s a mix of things that happen together: abdominal pain, bloating, diarrhea, constipation, or both. The pain usually gets worse after eating and improves after you go to the bathroom. It’s not the kind of pain you can ignore - it can be sharp, crampy, or a deep ache that makes you stop what you’re doing.
Bloating is another big one. Your stomach might swell up, feel tight, and look bigger than usual - even if you haven’t overeaten. Some people feel like they’re carrying a balloon inside. Others notice mucus in their stool, extra gas, or the constant feeling that they haven’t fully emptied their bowels.
There are three main types of IBS, based on your main bowel pattern:
- IBS-D (diarrhea-predominant): Loose, watery stools, sudden urgency, sometimes multiple times a day. About 40% of people with IBS fall into this group.
- IBS-C (constipation-predominant): Hard, lumpy stools, straining, feeling incomplete after going. This affects around 35%.
- IBS-M (mixed): You switch between diarrhea and constipation. About 25% of people experience this pattern.
And it’s not just your gut. Around 7 in 10 people with IBS also deal with symptoms outside the digestive tract - like acid reflux, nausea, chest pain that isn’t heart-related, or even a lump-in-the-throat feeling. These aren’t separate problems. They’re part of how IBS affects your whole body.
How Do You Know It’s IBS - And Not Something Else?
There’s no single test for IBS. Doctors diagnose it by ruling out other conditions and checking if your symptoms match the Rome IV criteria. That means you’ve had abdominal pain at least once a week for the last three months, and it’s linked to bowel movements - either changing how often you go or how your stool looks.
But before they say "it’s IBS," they need to make sure it’s not something more serious. That’s why they look for "red flags" - signs that need extra testing:
- Starting symptoms after age 50
- Unexplained weight loss
- Blood in your stool
- Anemia (low iron levels)
- Family history of colon cancer or Crohn’s disease
- Diarrhea that wakes you up at night
If any of these are present, you’ll likely need blood tests, a stool test for inflammation (like calprotectin), or even a colonoscopy. For most people under 45 with no red flags, doctors can diagnose IBS based on symptoms alone - no invasive tests needed.
What Makes IBS Symptoms Worse
IBS doesn’t flare up randomly. Something usually triggers it. And for most people, it’s a mix of food, stress, and hormones.
Food is the biggest trigger - about 70% of people notice a clear link. High-FODMAP foods are the usual suspects. These are short-chain carbs that ferment in your gut and cause gas and bloating. Common ones include:
- Onions, garlic, and artichokes
- Wheat and rye bread
- Dairy products like milk and soft cheeses
- Apples, pears, and mangoes
- Honey and high-fructose corn syrup
- Artificial sweeteners like sorbitol and xylitol
Other common triggers: caffeine (coffee, tea, energy drinks), alcohol, spicy food, and fatty meals. You don’t have to cut all of these out forever - but figuring out which ones hit you hardest makes a huge difference.
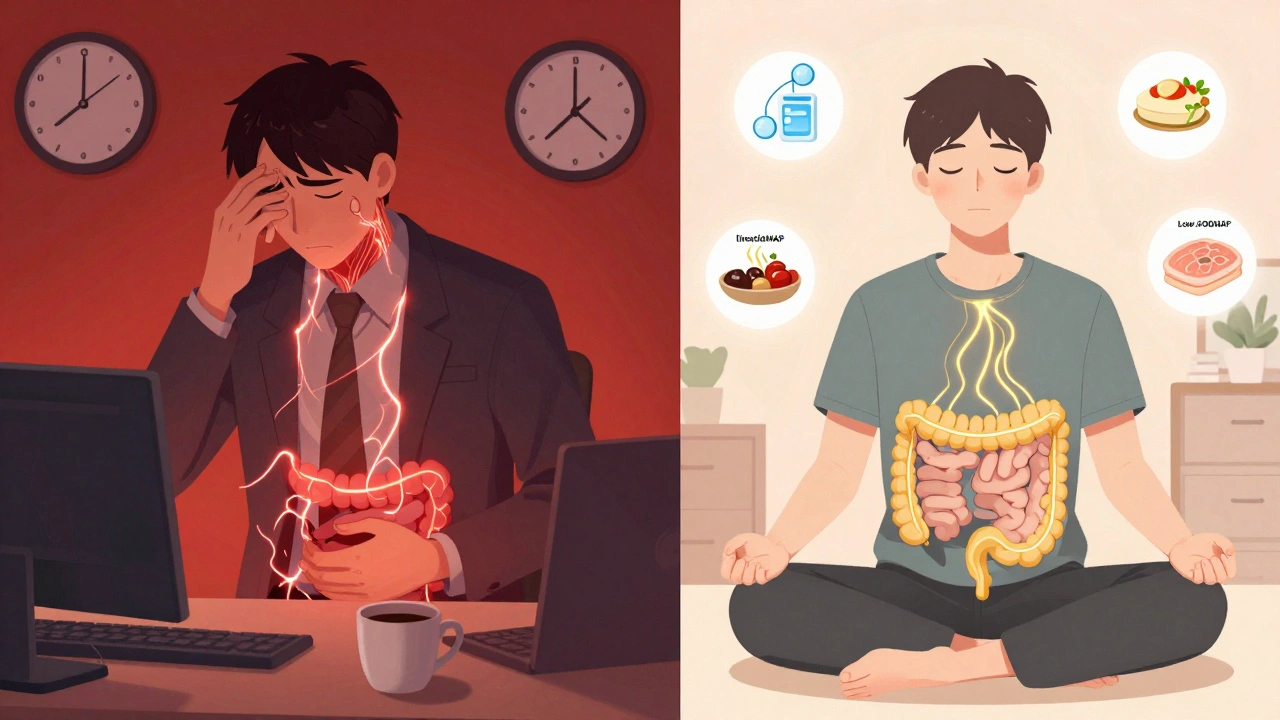
Stress doesn’t cause IBS, but it makes it worse. Studies show 60-80% of people report worse symptoms during stressful times - exams, work deadlines, family conflicts. Your gut and brain are wired together. When you’re anxious, your digestive system reacts. That’s why therapies like cognitive behavioral therapy (CBT) and gut-directed hypnotherapy work - they help calm that brain-gut connection.
Hormones play a big role too. Around 60-70% of women with IBS notice symptoms flare up right before or during their period. Estrogen and progesterone affect gut motility and sensitivity. If you’re on birth control or going through menopause, your symptoms might shift.
Antibiotics can also trigger IBS. About 1 in 4 people develop symptoms after a course of antibiotics. That’s because they disrupt the balance of good and bad bacteria in your gut - and that balance matters more than you think.
Medications That Actually Work
There’s no cure for IBS, but there are medications that help manage symptoms - and they’re chosen based on your subtype.
For IBS-D (diarrhea):
- Loperamide (Imodium): Over-the-counter. Slows down bowel movements. Works for about 6 in 10 people, but doesn’t touch the pain.
- Rifaximin (Xifaxan): A non-absorbed antibiotic. Taken for 14 days, it helps reduce bloating and diarrhea in 40-50% of people. It’s not for long-term use.
- Eluxadoline (Viberzi): FDA-approved in 2015. Reduces both pain and diarrhea. But it’s not safe for people without a gallbladder or with certain liver issues.
For IBS-C (constipation):
- Linaclotide (Linzess): Taken daily. Draws water into the intestines to soften stool. About 30-40% of people get at least three full bowel movements a week.
- Plecanatide (Trulance): Similar to linzess, but may cause less diarrhea as a side effect.
- Lubiprostone (Amitiza): Increases fluid secretion in the gut. Works for about 1 in 3 people.
For pain and overall symptoms:
- Antispasmodics like dicyclomine (Bentyl) or hyoscine (Buscopan): Help relax gut muscles. About 55% of people report less cramping.
- Low-dose antidepressants like amitriptyline (10-30 mg at night): Not for depression. These help by calming nerve signals between gut and brain. Works for 40-50% of people after 4-8 weeks.
Probiotics? Only one strain has solid proof: Bifidobacterium infantis 35624. It improved overall symptoms in about 35% of people in clinical trials. Most other probiotics? No clear benefit.
What Works Better Than Pills
Medications help, but the most effective long-term strategy is lifestyle-based. The low-FODMAP diet, when guided by a registered dietitian, improves symptoms in 50-75% of people. It’s not a forever diet - it’s a three-step process:
- Elimination: Cut all high-FODMAP foods for 2-6 weeks.
- Reintroduction: Add them back one at a time to find your triggers.
- Personalization: Build a diet that avoids only your specific triggers.
Studies show 70% of people identify their personal triggers during the reintroduction phase. That means you don’t have to give up forever - just avoid the ones that hurt you.
Stress management isn’t optional. Gut-directed hypnotherapy and CBT have success rates of 40-60% - comparable to medication. Many people find relief through mindfulness, yoga, or even regular walking. The goal isn’t to eliminate stress - it’s to change how your body reacts to it.
For people who’ve struggled for years, combining diet, stress tools, and the right medication leads to improvement in 60-70% of cases within six months.
What’s Next for IBS Treatment
Research is moving fast. Scientists are now looking at gut bacteria as a key player. In 2023, the FDA gave breakthrough status to a new drug called ibodutant, which targets nerve signals in the gut. Early results show 45% of patients had major symptom relief - double the placebo group.
Fecal microbiota transplants (FMT) - basically a gut bacteria transplant - are being tested in trials. One study found 35% of IBS patients went into remission after FMT, compared to 15% in the control group.
But here’s the truth: even with new drugs, personalized care is still the gold standard. No one-size-fits-all solution exists. What works for your friend might not work for you. That’s why tracking your symptoms - what you ate, how stressed you were, when you slept - is one of the most powerful tools you have.
Living With IBS: Real Talk
Many people wait over six years to get diagnosed. That’s not because doctors are slow - it’s because symptoms overlap with other conditions. If you’ve been dismissed, keep pushing. Bring your symptom log. Mention the Rome IV criteria. Ask about FODMAPs.
And don’t believe the myth that IBS is "just anxiety." It’s real. It’s physical. It’s measurable. And it’s manageable.
People with IBS miss an average of 13 work or school days a year. That’s a lot. But with the right mix of diet, stress tools, and medication, most people can get back to living - not just surviving.
You don’t have to wait until your next flare-up to start making changes. Pick one thing: track your meals for a week. Try a 10-minute breathing exercise before bed. Talk to your doctor about loperamide or a low-FODMAP diet. Small steps add up.
Can IBS turn into colon cancer?
No, IBS does not increase your risk of colon cancer or cause permanent damage to your intestines. It’s a functional disorder - meaning your gut looks normal on scans, but it doesn’t work properly. However, if you develop new symptoms like unexplained weight loss, blood in stool, or anemia, you need to see a doctor to rule out other conditions like colorectal cancer or inflammatory bowel disease.
Is the low-FODMAP diet hard to follow?
Yes, it’s challenging - especially at first. Many people find it overwhelming because it cuts out common foods like bread, onions, garlic, and dairy. But it’s not meant to be permanent. Working with a registered dietitian helps you eliminate only what’s necessary, then safely reintroduce foods to find your personal triggers. About 78% of people report difficulty sticking to it long-term, but 62% say their symptoms improved enough to make it worth it.
Do probiotics help with IBS?
Most probiotics don’t help - but one strain does: Bifidobacterium infantis 35624. It’s available in specific supplements like Align or VSL#3. Studies show it improves bloating, pain, and bowel habits in about 35% of users. Other probiotics, even popular ones like Lactobacillus or Bifidobacterium lactis, haven’t shown consistent benefits in high-quality trials. Don’t waste money on random probiotics - look for this specific strain.
Can stress cause IBS?
Stress doesn’t cause IBS, but it makes symptoms much worse. People with IBS have a more sensitive gut-brain connection. When you’re stressed, your brain sends stronger signals to your gut, which can trigger pain, cramping, or changes in bowel habits. That’s why therapies like cognitive behavioral therapy (CBT) and gut-directed hypnotherapy are so effective - they help retrain that connection. Managing stress won’t cure IBS, but it’s one of the most powerful tools for reducing flare-ups.
How long does it take for IBS medication to work?
It depends on the drug. Loperamide works within hours. Linaclotide and eluxadoline usually show results in 1-2 weeks. Antispasmodics like Bentyl may take a few days. Low-dose antidepressants like amitriptyline take the longest - 4 to 8 weeks at full dose before you see improvement. Don’t give up if you don’t feel better right away. Some treatments need time to build up in your system.
Should I avoid gluten if I have IBS?
Only if you’ve been tested for celiac disease and it’s negative. Many people with IBS feel better on a gluten-free diet, but that’s often because they’re cutting out wheat - which is high in FODMAPs (fructans), not because gluten itself is the problem. A 2022 study found that 70% of people who thought gluten triggered their IBS had no reaction when tested under controlled conditions. Test for celiac first. If it’s negative, focus on FODMAPs instead.





bobby chandra
December 3, 2025 AT 03:08IBS is the silent ninja of digestive disorders-quiet, relentless, and always showing up when you least want it. I used to think it was just ‘bad gut luck’ until I tracked my meals and realized onions and garlic were my personal villains. The low-FODMAP diet? Brutal at first, but life-changing. I can now eat dinner without mentally calculating bathroom access. No magic pill beats knowing your triggers.
And yes-stress makes it worse. But it’s not ‘all in your head.’ Your gut has its own nervous system. It’s biology, not weakness.
Start small. One week of food journaling. One deep breath before bed. You’ve got this.
Archie singh
December 4, 2025 AT 07:53Let’s be real-most people with IBS are just weak-willed and overindulgent. You think your ‘sensitive gut’ is special? Everyone’s gut reacts to stress. You’re just lazy. Stop blaming food. Stop chasing probiotics like they’re holy water. The real problem? You refuse to eat like a normal human. Cut out the drama. Eat plain chicken and rice. Done.
Also-FODMAPs? That’s just a fancy word for ‘I can’t handle real food.’
Gene Linetsky
December 5, 2025 AT 18:14Wait-so you’re telling me Big Pharma doesn’t want you to know that IBS is caused by 5G radiation and glyphosate in your kombucha? I’ve been researching this for 17 years and I’ve got spreadsheets. The FDA knows. The WHO knows. They’re just covering it up because the gut-brain axis is a backdoor for mind control.
Also, FMTs? That’s just fecal transplants. Sounds like a sci-fi horror movie. But here’s the truth: if you take activated charcoal with magnesium citrate every 48 hours and avoid all electromagnetic fields, your IBS vanishes. I’ve cured three people this way. One of them was my cousin. He’s now a yoga instructor in Bali.
They don’t want you to know this. But now you do.
Ignacio Pacheco
December 7, 2025 AT 15:49So let me get this straight-you’re telling me a drug called ibodutant works better than placebo, but we still don’t know why? And the ‘gold standard’ is… keeping a food diary? Wow. Medicine is just glorified guesswork wrapped in jargon.
Also, ‘gut-directed hypnotherapy’? That’s not a treatment. That’s a TED Talk with a fancy name. But hey, if whispering to your colon helps you sleep, more power to you. I’ll stick with loperamide and denial.
Jim Schultz
December 7, 2025 AT 23:31Okay, but let’s analyze this statistically: 70% of IBS patients report food triggers? That’s a massive correlation-but correlation isn’t causation! Did anyone control for confounding variables like sleep deprivation, screen time before bed, or chronic underhydration? No. And yet, we’re handing out low-FODMAP diets like they’re gospel.
Also, the claim that ‘Bifidobacterium infantis 35624’ works? That’s one study. One. And it was funded by a supplement company. Where’s the independent replication? Where’s the meta-analysis? Where’s the power calculation? This isn’t medicine-it’s anecdotal marketing dressed in lab coats.
And don’t get me started on ‘gut-brain axis’-it’s a buzzword with zero mechanistic clarity. We’re treating symptoms, not root causes. And calling it ‘manageable’? That’s just a euphemism for ‘we have no cure.’
Kidar Saleh
December 9, 2025 AT 02:05Living with IBS in the UK is a different kind of hell. The NHS won’t refer you to a dietitian until you’ve suffered for five years. I waited three years just to get a referral. By then, I’d tried every supplement, every diet, every ‘natural remedy’ known to man.
But when I finally got the low-FODMAP guidance? It changed everything. Not because it was perfect-but because someone listened. Not just told me to ‘take a pill’ or ‘stop being stressed.’
IBS doesn’t care about your job title, your income, or your social media followers. It just wants you to know: you’re not broken. You’re just wired differently. And that’s okay.
Find your rhythm. Not the ‘perfect’ one. Yours.
Chloe Madison
December 9, 2025 AT 18:21As someone who’s helped over 200 clients manage IBS through diet and stress coaching, I can tell you this: the most powerful tool isn’t a pill-it’s consistency. Not perfection. Consistency.
One client, a 42-year-old teacher, tracked her meals for 14 days. She discovered that her morning latte and almond butter toast were triggering her IBS-D. She switched to oat milk and gluten-free toast. Within two weeks, she was back to teaching without panic attacks before class.
And yes-stress is a trigger. But it’s not the villain. It’s the signal. Your body is screaming, ‘I need rest.’ So rest. Breathe. Walk. Journal. Drink water. These aren’t ‘alternative’ practices. They’re biological necessities.
You don’t need to be a nutritionist. You just need to pay attention. Start today. One meal. One breath. One step.
Vincent Soldja
December 10, 2025 AT 12:51IBS is real.