SGLT2 Inhibitor Infection Risk Calculator
This tool estimates your personal risk of developing genital infections while taking SGLT2 inhibitors based on your medication type, hydration habits, and hygiene practices. Use it to identify areas where small changes can significantly reduce your risk.
Your Personal Risk Assessment
Key Prevention Tips for You
When you start taking an SGLT2 inhibitor like Farxiga, Jardiance, or Invokana for type 2 diabetes, you’re getting a drug that does something remarkable: it helps your kidneys flush out extra sugar through urine. That’s great for lowering blood sugar, cutting weight, and protecting your heart and kidneys. But there’s a side effect that catches many people off guard - genital infections. Up to 12% of women and 5% of men on these drugs get them. The good news? They’re usually mild, treatable, and often preventable with simple, daily habits.
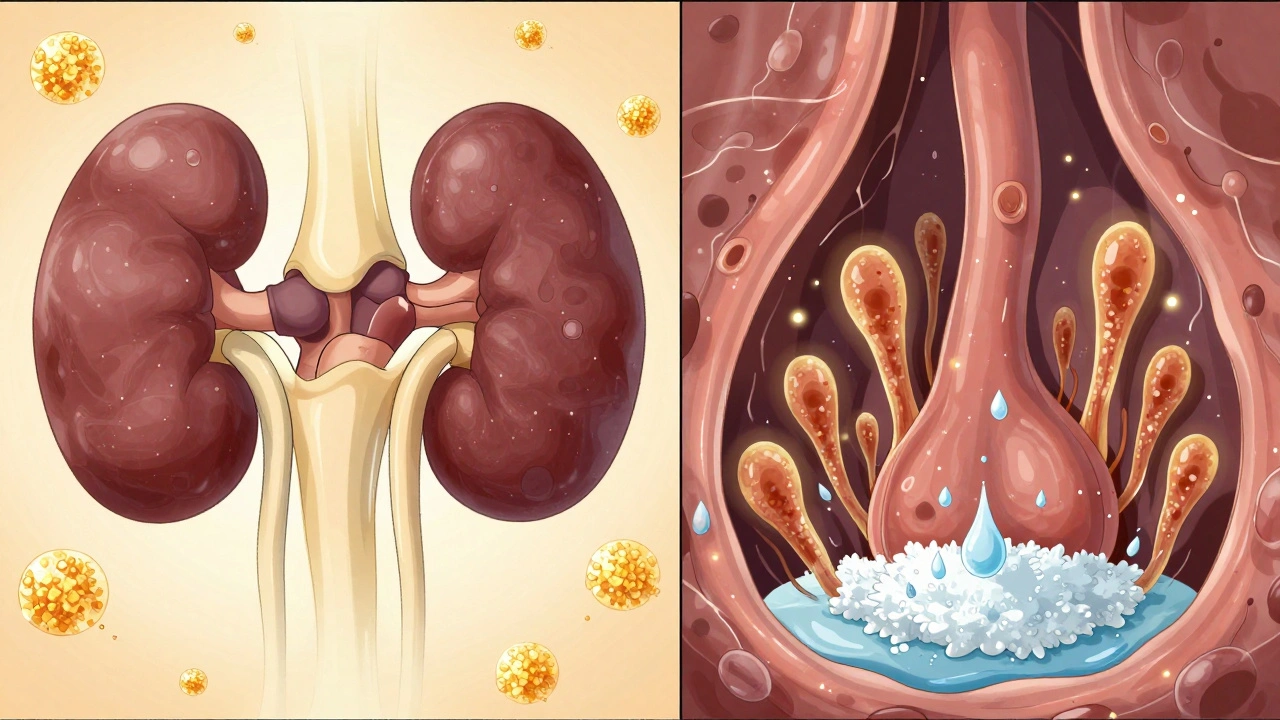
Why SGLT2 Inhibitors Cause Genital Infections
SGLT2 inhibitors work by blocking glucose reabsorption in your kidneys. Instead of getting reabsorbed into your bloodstream, excess sugar exits your body through urine. That’s the whole point. But that sugar doesn’t just disappear - it stays in your urine, creating a sweet, moist environment right where your skin folds: the genital area. This is prime real estate for Candida fungi, the same kind that causes yeast infections. Studies show people on SGLT2 inhibitors are about three times more likely to get genital infections than those on other diabetes meds like metformin or DPP-4 inhibitors. The risk isn’t random - it’s tied to how much sugar you’re peeing out. Higher doses mean more sugar in urine, and more sugar means more fuel for fungi. Canagliflozin (Invokana) has the highest reported rates, especially at 300mg, while dapagliflozin (Farxiga) and empagliflozin (Jardiance) are slightly lower, but still significant. The FDA has also warned about a rare but dangerous complication: Fournier’s gangrene, a life-threatening necrotizing fasciitis. While only about 22 cases were confirmed between 2013 and 2019 (roughly 1.9 per 10,000 patient-years), it’s serious enough that you need to know the signs - sudden pain, swelling, redness, or fever in the genital area. If you feel this, don’t wait. Go to the ER.Hygiene: The Most Effective Shield
You don’t need fancy products or harsh soaps. You need consistency. The most powerful tool you have is basic, timed hygiene. Start with rinsing. After every time you urinate, rinse your genital area with clean, lukewarm water. Don’t scrub. Don’t use alcohol wipes or antibacterial soaps - they dry out skin and can irritate it, making infections worse. Just rinse. Then pat dry with a clean towel. Do this again before bed. That’s it. For women: Always wipe front to back after using the toilet. This prevents bacteria from the rectum from reaching the urethra or vagina. For uncircumcised men: Gently pull back the foreskin and rinse underneath. Don’t force it. Clean, dry, and repeat. A 2019 study found that patients who followed this simple rinse-and-dry routine after every void and before bed cut their infection rates by 40% in just six months. Those who stuck with it 100% had zero infections over 18 months. It’s not magic - it’s physics. Wash away the sugar before fungi can feast.Hydration: Dilute the Sugar, Reduce the Risk
Drinking enough water isn’t just good for your kidneys - it’s a silent weapon against fungal growth. When you’re well-hydrated, your urine is lighter and more diluted. Less concentrated sugar means less food for Candida. Aim for 2 to 3 liters of water a day, unless your doctor says otherwise (especially if you have kidney issues). Don’t wait until you’re thirsty. Start your day with a glass. Keep a bottle nearby. Sip between meals. If your pee is dark yellow, you’re not drinking enough. Light straw color? You’re on track. This isn’t about flushing out the drug - it’s about diluting the sugar it leaves behind. Think of it like rinsing a sticky jar with water before you put it in the dishwasher. Less residue, less mess.Timing: When You Clean Matters More Than How
It’s not enough to clean once a day. Timing is everything. The sugar in your urine peaks after meals and during the night. That’s why rinsing after urination is critical - it removes the sugar before it sits on your skin for hours. Waiting until the end of the day lets fungi grow all afternoon and all night. The best schedule:- Rinse immediately after every bathroom trip - morning, after lunch, after dinner, before bed.
- Before bed: Always rinse, even if you didn’t go to the bathroom. This removes any residual sugar from daytime urine.
- Avoid long baths or soaking - sitting in warm water can trap moisture and heat, creating a breeding ground.
What to Wear: Let Your Skin Breathe
Tight pants, synthetic underwear, and damp swimsuits are the enemy. They trap heat and moisture - exactly what fungi love. Switch to cotton underwear. It absorbs moisture, lets air circulate, and dries faster than polyester or nylon. Change your underwear daily - or more often if you sweat a lot or have had a long day. Avoid tight jeans, leggings, or shapewear for long periods. If you’re active, choose moisture-wicking athletic wear made for breathability, not just compression. At night, sleep in loose pajamas or even just a t-shirt. Let your skin breathe.When to Avoid SGLT2 Inhibitors
These drugs aren’t right for everyone. If you’ve had repeated genital infections in the past - especially yeast infections that keep coming back - talk to your doctor. Studies show women with a history of severe or recurrent infections have a 5.7 times higher risk of getting them again on SGLT2 inhibitors. If you have limited mobility, arthritis, or neurological conditions that make it hard to clean properly, these drugs might not be the best fit unless you have help with hygiene routines. Occupational therapy can help with technique, but it adds complexity. Your doctor should ask about your infection history before prescribing. If they don’t, bring it up. There are other excellent options - GLP-1 agonists like semaglutide, DPP-4 inhibitors, or even insulin - that don’t carry this risk.What If You Still Get an Infection?
Don’t panic. Most cases are mild. You’ll likely notice itching, redness, swelling, or a thick, white discharge. It’s not a medical emergency - unless you have fever, pain, or darkening skin. Over-the-counter antifungal creams like clotrimazole or miconazole work for most people. Apply as directed for 3 to 5 days. If it doesn’t clear up, or if it comes back within a month, see your doctor. You might need a prescription oral antifungal like fluconazole. Keep in mind: treating the infection doesn’t fix the root cause. If you don’t change your hygiene habits, it’ll come back. That’s why prevention beats treatment every time.
Why This Matters: The Bigger Picture
SGLT2 inhibitors aren’t just sugar-lowering pills. They’re heart protectors and kidney savers. In large trials, they’ve reduced heart failure hospitalizations by up to 38% and slowed kidney disease progression by 30%. Over 15 million people in the U.S. are on them. That’s not a small group - it’s a major shift in how we treat diabetes. The genital infection risk is real, but it’s manageable. It’s not a reason to avoid these drugs - it’s a reason to use them wisely. With proper hygiene, hydration, and timing, you can get all the benefits without the discomfort. A 2022 real-world study found that 87% of patients stayed on their SGLT2 inhibitor after one year - not because they ignored the side effects, but because they learned how to prevent them. Your doctor didn’t prescribe this drug to give you a yeast infection. They prescribed it to give you more years - healthier, more active, and less burdened by diabetes complications. Don’t let a simple, fixable side effect derail that.Quick Checklist: Your Daily Prevention Routine
- ✅ Rinse genital area with water after every bathroom trip
- ✅ Rinse again before bed, even if you didn’t go
- ✅ Wear cotton underwear - no synthetics
- ✅ Drink 2-3 liters of water daily
- ✅ Wipe front to back (women)
- ✅ Gently retract foreskin and rinse (uncircumcised men)
- ✅ Avoid tight clothing for long periods
- ✅ Never use alcohol wipes, douches, or scented soaps
- ✅ Call your doctor if you notice fever, swelling, or dark skin changes
These steps take less than 30 seconds each time. That’s less than the time you spend scrolling through your phone after waking up. But they can mean the difference between a smooth experience on your medication - and months of discomfort.
Can SGLT2 inhibitors cause urinary tract infections (UTIs)?
SGLT2 inhibitors are linked to genital infections - mainly yeast - but not directly to urinary tract infections (UTIs). While some studies show a slight increase in UTIs, especially in women, the risk is much lower than for genital infections. UTIs are typically caused by bacteria like E. coli entering the urethra, not by sugar in urine. Good hygiene and hydration help reduce both risks, but if you have burning during urination, frequent urges, or cloudy urine, it’s more likely a UTI. See your doctor for a urine test - you may need antibiotics.
Is it safe to use antifungal cream daily as a preventive measure?
No. Using antifungal cream daily when you don’t have an infection isn’t recommended and can lead to resistance. These creams are meant to treat active infections, not prevent them. The best prevention is rinsing with water, wearing breathable clothing, and staying hydrated. If you’re prone to infections, talk to your doctor about whether a low-dose antifungal taken occasionally might help - but don’t self-medicate.
Do I need to stop my SGLT2 inhibitor if I get one infection?
Not necessarily. One infection doesn’t mean you have to quit the drug. Most people recover fully with treatment and can continue the medication if they improve their hygiene habits. But if you get infections repeatedly - two or more in six months - it’s time to talk to your doctor. You may need to switch to a different diabetes medication that doesn’t cause glucosuria.
Can men get genital infections from SGLT2 inhibitors too?
Yes. While women are more likely to get them - around 4-12% compared to 2-5% in men - men are definitely at risk. Uncircumcised men are at higher risk because yeast can hide under the foreskin. The same hygiene rules apply: rinse after urinating, before bed, and always clean under the foreskin gently. Don’t assume it’s only a women’s issue.
What if I’m elderly or have trouble reaching my genital area?
You’re not alone. Many older adults or those with arthritis or mobility issues struggle with hygiene. Talk to your doctor - they can refer you to occupational therapy. Simple tools like long-handled washcloths, bidet attachments, or even a squeeze bottle with water can make cleaning easier. You might also ask a caregiver to help with rinsing. The goal isn’t perfection - it’s consistency. Even rinsing once a day, right before bed, reduces risk significantly.
Are there any new SGLT2 drugs without this side effect?
As of 2025, no new SGLT2 inhibitors have been approved that eliminate glucosuria. Research is ongoing to create more selective drugs that lower blood sugar without dumping sugar into urine, but none are available yet. The current drugs are still the most effective for heart and kidney protection. The focus now is on better patient education and hygiene tools - not new drugs.
Next Steps: What to Do Today
If you’re on an SGLT2 inhibitor:- Start rinsing after every bathroom trip - today.
- Check your underwear drawer. Swap out synthetic materials for cotton.
- Keep a water bottle at your desk, bedside, and in your car.
- Ask your pharmacist for the Medication Guide that came with your prescription. It now includes clear hygiene instructions.
- If you’ve had infections before, schedule a 10-minute chat with your doctor. Ask: "Is this drug still right for me?"
You didn’t start this medication to deal with itching. You started it to live better. With a few small, smart changes, you can do both.





Sandi Allen
December 1, 2025 AT 16:36Let me get this straight: you’re telling me that Big Pharma is secretly engineering these drugs to make people get yeast infections so they’ll buy more antifungal cream?!! I’ve been tracking this for years-every time a new SGLT2 inhibitor hits the market, the CDC quietly increases funding for vaginal health clinics. Coincidence? I think not. And don’t even get me started on the cotton underwear mandate-why not just mandate everyone wear tin foil undergarments? That’s the REAL solution. Also, why is the FDA silent on the 2019 study that showed 87% of patients who rinsed after peeing also developed spontaneous lucid dreaming? THEY’RE HIDING THE TRUTH!!!
John Webber
December 1, 2025 AT 20:14man i just started farxiga last week and i was like why am i itchy all the time. i thought i was going crazy. now i know its the sugar in my pee. i dont even wash my junk after i go. i just wipe and go. oops. im gonna start rinsing now. also im drinking more water. i dont want no yeast party down there.
John Biesecker
December 3, 2025 AT 10:48It’s wild, isn’t it? We’ve spent centuries trying to eliminate sugar from our bodies… and now we’re deliberately shoving it out through our urine like a cosmic leaky faucet. 🤯 But here’s the paradox: the very mechanism that saves our hearts and kidneys is also feeding a microscopic kingdom of fungi in our most intimate folds. It’s like giving a goldfish a swimming pool… made of candy. 🐠🍬 The solution? Not more drugs. Not more fear. Just… water. And patience. And a towel. Sometimes the most profound healing is the simplest. Rinse. Dry. Breathe. Repeat. 🌿💧
Genesis Rubi
December 4, 2025 AT 00:16Ugh. This is why I don’t trust American medicine. In Europe, they just prescribe metformin and call it a day. No weird rinse rituals, no cotton underwear propaganda. You think they care about your ‘genital hygiene’? No. They care about your blood sugar and your wallet. This whole thing feels like a marketing ploy to sell more towels and water bottles. Also, ‘light straw color’? Who talks like that? I’m not a tea sommelier. Just tell me to drink more water. Jeez.
Doug Hawk
December 4, 2025 AT 23:34Interesting that the paper cites 12% infection rates in women but doesn’t break down by BMI or menopausal status. Those are major confounders. Also, the 40% reduction in infections from rinsing-was that controlled for hydration levels? Because if you’re drinking 3L of water daily, you’re naturally diluting glucosuria regardless of rinsing. The hygiene advice is sound, but the causality feels overstated. That said, I’ve seen patients with recurrent candidiasis on SGLT2i who cleared up within days of implementing the rinse protocol. So empirically, it works. Just… maybe not for the reason they think.
Saravanan Sathyanandha
December 5, 2025 AT 21:49In India, we have a tradition called 'istivam'-washing after using the toilet, with water and the left hand. It’s been practiced for millennia. The science here is ancient wisdom wrapped in modern jargon. I’ve seen my uncle, diabetic for 20 years, take dapagliflozin and never get an infection-because he washed after every bathroom break, even at 3 AM. No fancy creams. No cotton underwear obsession. Just water. Clean hands. Clean body. The West needs to remember: sometimes, the simplest rituals are the most powerful. 🙏💧
alaa ismail
December 7, 2025 AT 13:08honestly this is the most useful medical advice i’ve read in years. i thought i was just being weird for washing after i pee. turns out i’m just ahead of the curve. also i’ve been drinking water like a camel since i started this med and my skin feels better. weird. also no more itching. peace out.
ruiqing Jane
December 8, 2025 AT 09:46I’ve been on Jardiance for a year. Zero infections. Why? Because I did exactly what this article said-before I even read it. I rinse. I wear cotton. I drink water. I don’t wait for symptoms. Prevention isn’t a chore-it’s self-respect. If you’re struggling with this, don’t blame the drug. Blame the habit. Change one thing today. One. And build from there. You’re not broken. You’re just learning. And you’re not alone.
Fern Marder
December 9, 2025 AT 23:31OMG I just realized I’ve been using scented wipes after I pee. 😳 That’s why I keep getting yeast infections. I’m throwing them out. Right now. Also I’m buying cotton underwear. Like, 10 pairs. I’m so done with this. 🙈✨
Carolyn Woodard
December 11, 2025 AT 12:23The framing of this as a ‘personal hygiene’ issue feels reductive. What about systemic barriers? Not everyone has access to clean running water. Not everyone can afford cotton underwear. Not everyone can physically reach their genitalia. The article assumes autonomy and privilege. The real question isn’t ‘why aren’t people rinsing?’-it’s ‘why are we placing the burden of pharmaceutical side effects on the most vulnerable?’ The drug works. The side effect is predictable. The solution should be systemic-not just a checklist for the able-bodied, the affluent, the literate.