When you’re pregnant, even a simple headache can turn into a panic. First trimester medication safety isn’t just a checklist-it’s a life-changing decision made in the dark. You’re not just taking a pill. You’re affecting a tiny, rapidly forming human being. And the clock is ticking.
Why the First 12 Weeks Are Everything
The first trimester isn’t just the early stage of pregnancy. It’s the most critical window for your baby’s body to build itself from scratch. From day 17 to day 56 after conception, every organ-heart, brain, limbs, eyes, ears-forms in a precise sequence. One missed step, one wrong chemical signal, and a structural defect can happen.That’s why 90% of major birth defects occur between weeks 3 and 8. Neural tubes close by day 26. The heart is wiring itself between days 20 and 40. Fingers and toes are shaping up by day 36. If you take a medication during this time, it doesn’t just float through your bloodstream-it can directly interfere with how your baby’s body is built.
This isn’t theory. The CDC and the National Birth Defects Prevention Study tracked over 5,000 pregnancies. They found that while many medications are commonly used, only two had solid, reliable safety data. The rest? We’re guessing.
What Medications Are Actually Safe?
Let’s cut through the noise. Not all meds are equal. Some have decades of use in pregnant people. Others? No one really knows.Acetaminophen (Tylenol) has been the go-to for pain and fever for years. The FHCSD says up to 4,000 mg daily is fine. But new research from 2023 suggests a possible link to higher risks of ADHD and autism with long-term or high-dose use. That doesn’t mean you can’t use it. It means: use the lowest dose for the shortest time. If you’re taking it every day for weeks, talk to your doctor.
NSAIDs like ibuprofen and naproxen are risky from the start. A 2011 Canadian study of 4,705 pregnancies found first-trimester use raised miscarriage risk by 60%. And it’s not just about losing the pregnancy. These drugs can interfere with early heart development. Skip them unless your doctor says otherwise.
Antibiotics are common. Amoxicillin? Safe. Cephalosporins? Safe. Erythromycin? Safe. Tetracycline? Never. It stains baby’s teeth and weakens bones. Fluoroquinolones like Cipro? Animal studies show cartilage damage. Human data is thin, but why risk it? Stick to the proven ones.
Antidepressants are a minefield. Paroxetine? Avoid. Studies show a 1.5 to 2 times higher risk of heart defects. Fluoxetine, sertraline, citalopram? No strong link to birth defects. But here’s the catch: stopping them can be more dangerous than taking them. Untreated depression increases preterm birth risk and can affect bonding. Work with your psychiatrist. Don’t quit cold turkey.
The Hidden Risks: OTC and Common Remedies
You wouldn’t think a cold medicine or antacid could hurt. But many do.Pseudoephedrine (Sudafed) is in almost every decongestant. A 2002 study linked it to gastroschisis-a rare abdominal wall defect. The risk is small, but real. Skip it in the first trimester. Use saline sprays or humidifiers instead.
Diphenhydramine (Benadryl), loratadine (Claritin), and cetirizine (Zyrtec)? Generally safe for allergies. But don’t overdo it. Some studies link high doses to fetal heart rhythm changes. One pill a day? Fine. Three a day? Not worth it.
Bismuth subsalicylate (Pepto-Bismol) sounds harmless. But it’s a form of aspirin. Aspirin can interfere with placental blood flow. Avoid it. Use ginger tea or small, frequent meals for nausea instead.
Loperamide (Imodium) for diarrhea? One study found 4 out of 226 babies exposed had heart defects. The risk is low, but again-why take it? Stick to hydration, bananas, rice, and applesauce until it passes.
What About Chronic Conditions?
If you have epilepsy, diabetes, asthma, or an autoimmune disease, stopping your meds isn’t an option. It’s deadly.For epilepsy, uncontrolled seizures raise fetal death risk by 400%. The right antiseizure meds? Way safer than seizures. Your neurologist and OB should work together. Never adjust your dose alone.
Diabetes? Uncontrolled blood sugar raises the risk of major birth defects from 2-3% to 10-15%. Tight control before and during pregnancy cuts that back down. Metformin and insulin are safe. Avoid oral meds like sulfonylureas unless absolutely necessary.
Thyroid meds? Levothyroxine isn’t just safe-it’s essential. Your body needs 30-50% more thyroid hormone during pregnancy. If your TSH goes above 2.5 mIU/L, your baby’s brain development suffers. Get tested early and often.
Hydroxychloroquine (Plaquenil) for lupus or rheumatoid arthritis? Safe in pregnancy. In fact, stopping it can cause flare-ups that harm both you and your baby.
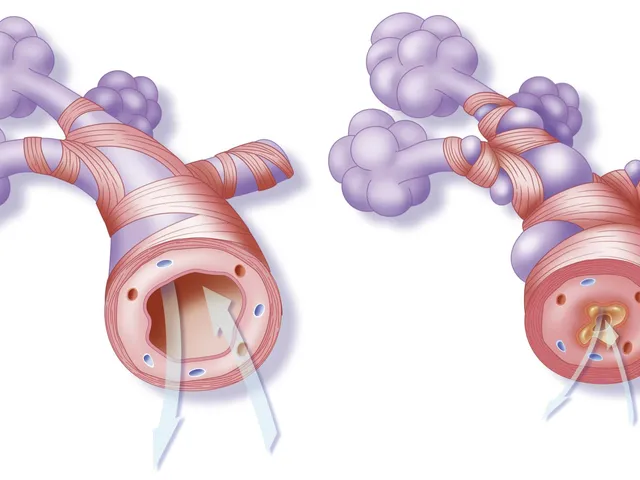
Corticosteroids? A 2013 meta-analysis found a possible 1.3 to 1.6 times higher risk of cleft lip or palate. But if you need them for asthma or severe allergies, the benefit outweighs the risk. Talk to your doctor about the lowest possible dose.
The Big Problem: We Don’t Know Enough
Here’s the truth: 98% of prescription drug labels don’t have clear pregnancy safety info. Only 10% of FDA-approved medications have solid data on how they affect a developing fetus.That’s not a failure of science. It’s a failure of policy. For decades, drug companies didn’t test on pregnant people. Why? Fear of lawsuits. So we’re flying blind.
Over 96% of commonly used medications lack enough human data to say if they’re safe. That’s not just inconvenient-it’s terrifying. A mother takes a medication because she’s in pain, or anxious, or sick. She doesn’t know if it’s harmless or harmful. And her doctor? Often doesn’t know either.
That’s why services like MotherToBaby exist. They field over 15,000 calls a year from pregnant people asking, “Is this safe?” They don’t guess. They pull from global databases, animal studies, and real human outcomes. If you’re unsure, call them. It’s free. It’s confidential. It’s lifesaving.
What to Do Right Now
If you’re pregnant-or thinking about it-here’s your action plan:- Confirm your dates. Know exactly when conception happened. Ultrasound dating is more accurate than your last period.
- List every medication. Prescription, OTC, vitamins, herbs, supplements. Even the ones you took last month.
- Check with a specialist. Don’t rely on Google or a pharmacist’s quick answer. Talk to a teratology expert or call MotherToBaby.
- Ask about alternatives. Can you use a heating pad instead of ibuprofen? Can you manage anxiety with therapy instead of meds?
- If you need meds, use the lowest dose for the shortest time. Never assume “it’s just a little.” Even small amounts can matter during organ formation.
There’s no perfect answer. But there’s a smarter way. You don’t have to choose between your health and your baby’s. You just need better information.
When to Worry-and When to Breathe
If you took a medication before you knew you were pregnant, don’t panic. Most exposures don’t cause harm. The risk is often tiny. What matters is what you do next.Did you take isotretinoin (Accutane)? That’s a hard stop. It causes severe birth defects in 20-35% of cases. Call your doctor immediately.
Did you take a single dose of ibuprofen for a headache? Probably fine. The risk is tied to repeated or prolonged use.
Did you start a new antidepressant? Don’t quit. Talk to your provider about switching to a safer option like sertraline if needed.
Most people who take medications in early pregnancy have healthy babies. But you owe it to yourself-and your baby-to be informed, not afraid.
Is acetaminophen safe during the first trimester?
Acetaminophen is still considered the safest pain reliever during pregnancy, with guidelines allowing up to 4,000 mg per day. However, recent studies suggest a possible link to increased risk of ADHD and autism with long-term or high-dose use. Use the lowest effective dose for the shortest time possible. Avoid daily use unless medically necessary.
Can I take ibuprofen in the first trimester?
It’s best to avoid ibuprofen and other NSAIDs in the first trimester. A 2011 study of over 4,700 pregnancies found a 60% increased risk of miscarriage with first-trimester use. NSAIDs can also interfere with early heart development. Use acetaminophen instead for pain or fever.
Is it safe to take prenatal vitamins with iron during the first trimester?
Yes. Prenatal vitamins with iron are not only safe-they’re essential. Iron supports increased blood volume and helps prevent anemia, which is common in pregnancy. Most prenatal vitamins also include folic acid, which reduces neural tube defect risk by up to 70%. Take them daily starting before conception if possible.
What should I do if I took a medication before knowing I was pregnant?
Don’t panic. Most exposures don’t cause harm. Write down the medication, dose, and when you took it. Call MotherToBaby or consult a teratology specialist. They’ll assess your specific situation using real data. Avoid self-diagnosing with internet searches-most are misleading or alarmist.
Are herbal supplements safe during the first trimester?
No. Most herbal supplements have not been tested for safety in pregnancy. Some, like black cohosh or dong quai, can trigger contractions. Others, like high-dose vitamin A, can cause birth defects. Stick to prenatal vitamins and avoid all herbs unless your doctor specifically approves them.
Can I continue my antidepressants during pregnancy?
It depends on the medication. Paroxetine should be avoided due to heart defect risks. Fluoxetine, sertraline, and citalopram are considered safer. But stopping antidepressants can increase risks of preterm birth, low birth weight, and postpartum depression. Work with your OB and psychiatrist to weigh risks and benefits-don’t stop on your own.
Is it safe to take allergy medications in the first trimester?
Loratadine (Claritin) and cetirizine (Zyrtec) are generally considered safe. Diphenhydramine (Benadryl) is also used, but avoid high doses. Avoid pseudoephedrine (Sudafed) in the first trimester due to a possible link to gastroschisis. Saline sprays and humidifiers are good non-drug alternatives.
What about thyroid medication like levothyroxine?
Levothyroxine is not only safe-it’s critical. Your thyroid needs increase by 30-50% during pregnancy. Untreated low thyroid function can affect your baby’s brain development. Get your TSH checked early and often. Your dose will likely need adjustment. Never stop taking it without medical advice.
Next Steps: What to Do Today
If you’re pregnant or planning to be:- Make a full list of everything you take-prescription, OTC, supplements, herbs.
- Call MotherToBaby (1-866-626-6847) or visit their website for free, expert advice.
- Schedule a pre-pregnancy or early pregnancy consult with your OB or a maternal-fetal medicine specialist.
- Stop taking anything you’re unsure about until you get professional advice.
- Start taking folic acid (400-800 mcg daily) if you haven’t already.
You’re not alone. Thousands of pregnant people face the same fears every day. The goal isn’t perfection. It’s awareness. And with the right information, you can protect your health-and your baby’s future-without living in fear.




Jocelyn Lachapelle
December 15, 2025 AT 13:20We’re not robots. We’re humans trying to survive.
Lisa Davies
December 15, 2025 AT 15:53Nupur Vimal
December 17, 2025 AT 14:02Melissa Taylor
December 18, 2025 AT 08:20Christina Bischof
December 18, 2025 AT 15:17Michelle M
December 19, 2025 AT 11:52Sai Nguyen
December 20, 2025 AT 23:54RONALD Randolph
December 22, 2025 AT 19:29Benjamin Glover
December 24, 2025 AT 09:58Raj Kumar
December 25, 2025 AT 06:56Mike Nordby
December 26, 2025 AT 12:17John Samuel
December 28, 2025 AT 03:50