Acetaminophen Dosing Calculator
This calculator determines safe daily acetaminophen limits based on your liver health and alcohol use. Always consult your doctor before taking any medication.
Maximum Safe Daily Dose:
Acetaminophen is one of the most common pain relievers in the world. You’ll find it in Tylenol, NyQuil, Vicodin, Sudafed, and over 600 other medicines-many of them sold without a prescription. It works well. It’s affordable. And for most people, it’s safe. But if you have liver disease, or even just drink alcohol regularly, the line between healing and harming can be thinner than you think. One extra pill. One cold medicine on top of your painkiller. One night of drinking after taking Tylenol. That’s all it can take to trigger serious liver damage-and sometimes, it’s too late by the time symptoms show up.
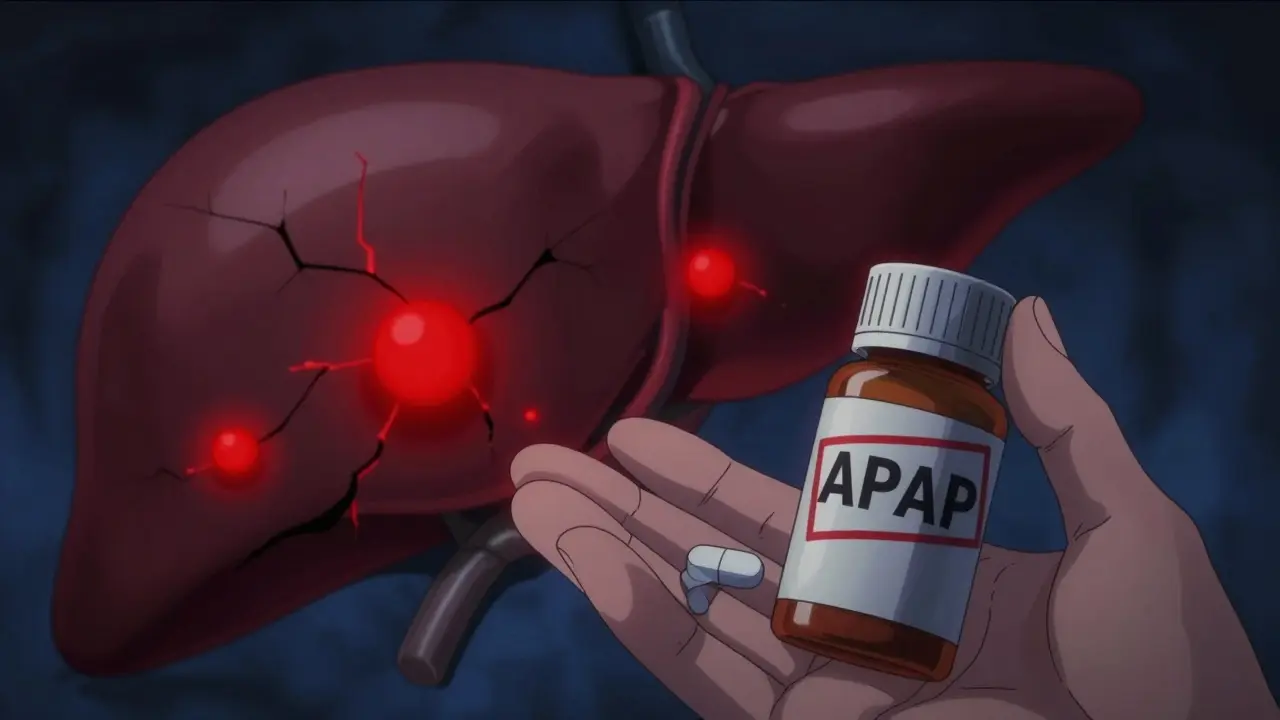
Why Acetaminophen Is Dangerous for People with Liver Disease
Your liver breaks down acetaminophen. Normally, it handles this job without trouble. But if your liver is already damaged-by hepatitis, fatty liver disease, alcohol use, or cirrhosis-it can’t process the drug the same way. Instead of safely converting acetaminophen into harmless waste, your liver starts producing a toxic byproduct called NAPQI. Healthy livers have enough glutathione to neutralize it. Damaged livers don’t. That’s when NAPQI starts killing liver cells. The result? Acute liver injury. In worst-case scenarios, it leads to liver failure.
What’s scary is that you might not feel anything until it’s too late. There’s no burning pain. No warning signs. Just fatigue, nausea, or vague discomfort-symptoms many people write off as a cold or the flu. By the time jaundice or confusion appears, the damage is often severe.
The Safe Dose Isn’t the Same for Everyone
The official maximum daily dose for a healthy adult is 4,000 milligrams. But that number is misleading if you have liver disease. For someone with cirrhosis, hepatitis, or a history of heavy drinking, experts recommend cutting that in half-no more than 2,000 mg per day. Some doctors even suggest staying under 3,000 mg if you’re unsure.
And here’s the catch: many over-the-counter products have higher doses than you think. Tylenol Extra Strength? Each pill is 500 mg. Take four of them, and you’ve hit 2,000 mg. Add one cold medicine with acetaminophen (often labeled as APAP on the bottle), and you’re already at 3,000 mg. Now you’re dangerously close to the danger zone.
For children, dosing is based on weight: 10 to 15 mg per kilogram every 4 to 6 hours, with a maximum of 80 mg per kg per day. But parents often guess the dose or use kitchen spoons. That’s a mistake. Always use the syringe or cup that comes with the medicine. A teaspoon isn’t a milliliter. A tablespoon isn’t 15 mL. Even small errors can be dangerous in kids.
Alcohol and Acetaminophen: A Deadly Mix
If you drink alcohol regularly-even just a few drinks a week-you’re at higher risk. Alcohol makes your liver produce more of the toxic NAPQI while reducing your body’s ability to clear it. The combination doesn’t just increase risk. It lowers the safe dose. For people who drink, 2,000 mg a day is the absolute upper limit. Some experts say even that’s too much.
It’s not just about binge drinking. A daily glass of wine, a beer after work, or weekend drinking all add up. Many people don’t realize their alcohol use affects how their body handles medication. If you have liver disease and drink, you’re already stressing your liver. Adding acetaminophen is like pouring gasoline on a small fire.

Hidden Sources of Acetaminophen
You might not know you’re taking it. That’s the biggest problem.
- Vicodin, Percocet, and other opioid painkillers often contain acetaminophen.
- Cold and flu meds like NyQuil, DayQuil, and Theraflu all have it.
- Migraine meds like Excedrin include acetaminophen.
- Even some sleep aids and allergy pills list it as APAP.
Check every bottle. Look for “acetaminophen,” “APAP,” or “paracetamol.” If you’re taking more than one medicine, add up the total. Don’t assume the label says it all-some prescription bottles don’t highlight the acetaminophen content clearly. When in doubt, ask your pharmacist. They’ve seen this mistake happen too many times.
What to Do If You Think You’ve Overdosed
Time matters. If you’ve taken too much acetaminophen-whether on purpose or by accident-get help immediately. Don’t wait for symptoms. Don’t hope it’ll pass.
The antidote, acetylcysteine (NAC), works best if given within 8 hours of ingestion. It can still help up to 16 hours later, but every minute counts. Emergency rooms use the Rumack-Matthew nomogram-a chart that plots blood levels of acetaminophen against time after ingestion-to decide if you need treatment. If your levels are above the danger line, you’ll get NAC, usually through an IV.
Even if you’re not sure you took too much, tell the doctor everything you’ve taken. List all pills, liquids, and supplements. They’ll check your liver enzymes and run a blood test. If you’re pregnant, don’t delay. NAC is safe during pregnancy and can save both your life and your baby’s.

How to Use Acetaminophen Safely with Liver Disease
Here’s what actually works:
- Never exceed 2,000 mg per day if you have liver disease or drink alcohol.
- Avoid alcohol completely while taking acetaminophen.
- Read every label. Look for APAP or acetaminophen. Add up all sources.
- Use the lowest effective dose. If 325 mg works, don’t take 650 mg.
- Use a pill organizer or app to track doses. Don’t rely on memory.
- Ask your doctor before taking any new medicine-prescription or OTC.
- Keep all medications out of reach of children. Accidental overdoses in kids are common.
For chronic pain, talk to your doctor about alternatives. NSAIDs like ibuprofen carry their own risks, but they don’t harm the liver the same way. Physical therapy, heat packs, or nerve-targeted treatments might be safer long-term options.
What Happens After Liver Damage?
If acetaminophen causes liver failure, the only cure is a transplant. About 1,600 people in the U.S. develop acute liver failure from acetaminophen every year. Around 500 of them die. Many more survive but face years of recovery, ongoing monitoring, and sometimes permanent liver damage.
It’s not just about one bad decision. It’s about not knowing the rules. That’s why education matters. The same people who check food labels for sugar or sodium often ignore medicine labels. But acetaminophen doesn’t care if you’re trying to be careful. It only cares how much you take-and what your liver can handle.
Final Reality Check
You don’t need to avoid acetaminophen entirely if you have liver disease. But you do need to treat it like a loaded gun. One wrong move, and the consequences are irreversible. The safe dose isn’t a suggestion. It’s a boundary. Cross it once, and you might not get a second chance.
Don’t wait for a warning sign. Don’t assume your doctor told you everything. Don’t think it won’t happen to you. Thousands of people thought the same thing. Check your meds. Track your doses. Talk to your pharmacist. And if you’re unsure-skip it. There are other ways to manage pain. Your liver will thank you.




Alex Carletti Gouvea
January 19, 2026 AT 20:49Look, I don’t care if you have cirrhosis or drink like a fish-4,000 mg is the label limit, and if you can’t read a bottle, that’s your problem. Stop crying about ‘safe doses’ and take responsibility. I’ve been taking Tylenol with my beer for 20 years and my liver’s still ticking. Don’t infantilize adults.
Ben McKibbin
January 21, 2026 AT 07:56There’s a chilling elegance in how acetaminophen exploits vulnerability-it’s not malicious, just indifferent. Your liver doesn’t judge you for drinking, for taking extra pills, for trusting the label. It just metabolizes. And when it can’t, it dies quietly, cell by cell, while you scroll through memes thinking you’re fine. This isn’t about dosage limits-it’s about the illusion of control. We treat medicine like candy because we refuse to acknowledge our own fragility. The real toxicity isn’t NAPQI-it’s denial.
Rod Wheatley
January 22, 2026 AT 07:37PLEASE, PLEASE, PLEASE-read this carefully!! If you have liver disease OR drink alcohol-even one glass of wine a night-DO NOT exceed 2,000 mg per day!! I’ve seen too many people end up in the ER because they took ‘just one’ cold med on top of Tylenol!! Check EVERY bottle-APAP is acetaminophen!! Use a pill organizer!! Write it down!! Don’t rely on memory!! And if you’re unsure-ASK YOUR PHARMACIST!! They’re not just there to hand you pills-they’re your safety net!! Your liver doesn’t get a second chance!!
Uju Megafu
January 22, 2026 AT 19:51Oh wow, another ‘medical authority’ telling people what to do while sipping their organic matcha latte. Let me guess-you’ve never taken Tylenol in your life, have you? Meanwhile, people in Nigeria are dying from malaria because they can’t afford ibuprofen, and you’re here lecturing about ‘2,000 mg limits’? This is why America thinks it owns health. Your ‘expertise’ is just privilege wrapped in a warning label. Go fix your own broken system before you tell the rest of us how to die.
Ashok Sakra
January 24, 2026 AT 15:53Bro I took 10 tylenol once and felt fine. My cousin took 20 and lived. Your liver is like a muscle. You push it, it gets stronger. Why are you scared of medicine? Everyone knows acetaminophen is safe. You just need to be strong. Stop making it a big deal. I don’t even read labels. I just take what I need.
Andrew Rinaldi
January 26, 2026 AT 01:55I’ve been sitting with this for hours. It’s not the dosage that’s the issue-it’s the cultural blindness to how we treat our bodies as disposable machines. We’ve normalized self-harm through convenience. We don’t fear the drug; we fear the idea that we might be responsible for our own decline. The real tragedy isn’t the liver failure-it’s that we didn’t pause long enough to ask, ‘Why am I taking this?’ Maybe the pain isn’t in the body. Maybe it’s in the silence we refuse to hear.
Gerard Jordan
January 27, 2026 AT 01:18Big love to everyone reading this 🙏 Seriously-this is life-saving info. If you’re taking anything with APAP, stop. Look. Add. Pause. Breathe. Your liver is working overtime just to keep you alive. Don’t ask it to carry more than it can. You’re worth more than a quick fix. And if you’re unsure? Text your pharmacist. They’ll reply. They care. 💙
michelle Brownsea
January 28, 2026 AT 22:39It’s not just about the dose-it’s about the arrogance of pharmaceutical companies who design products to be dangerously confusing. ‘APAP’? Really? Who thought that was a good idea? And why do pharmacies not require a warning label on every single bottle that says, ‘THIS MAY KILL YOU IF YOU’RE NOT CAREFUL’? This isn’t medical advice-it’s corporate negligence dressed up as education. And don’t get me started on the fact that this isn’t even taught in high school health class. We’re raising a generation of people who think ‘over-the-counter’ means ‘harmless.’
Roisin Kelly
January 30, 2026 AT 20:59They’re lying. They always lie. Acetaminophen is a government tool to control the population. The liver damage? A cover-up for something bigger. I know someone who got sick after taking Tylenol-and then their insurance got canceled. Coincidence? Nah. They want you dependent on the system. Skip the meds. Drink lemon water. Your liver will thank you… or maybe it won’t. Who even knows anymore?