When your prescription costs more than your grocery bill, you’re not alone. Nearly 3 in 10 Americans skip doses or skip refills because they can’t afford their meds. The good news? There’s a proven, clinically safe way to cut those costs without sacrificing effectiveness: therapeutic alternative medication. It’s not just about switching to generics. It’s about finding a different drug-sometimes from a different class-that works just as well, but costs a fraction of the price.
What Is a Therapeutic Alternative?
A therapeutic alternative isn’t a generic version of your drug. It’s a different medication that treats the same condition with similar results. For example, if you’re taking brand-name esomeprazole (Nexium) for acid reflux, your doctor might suggest switching to generic omeprazole. Same effect. Same dose. One costs $365 a year. The other? $15.
This isn’t guesswork. Doctors and pharmacists use clinical guidelines to match medications based on real-world studies. The American College of Physicians says a therapeutic alternative must have:
- Proven equal effectiveness in head-to-head trials
- Similar safety risks
- Comparable dosing schedules
For instance, switching from Eliquis (apixaban) to warfarin for blood thinning can drop monthly costs from $450 to under $10. Or swapping Jardiance (empagliflozin) for generic metformin can cut diabetes treatment costs by 90%. These aren’t rare cases-they happen every day in clinics that know how to ask the right questions.
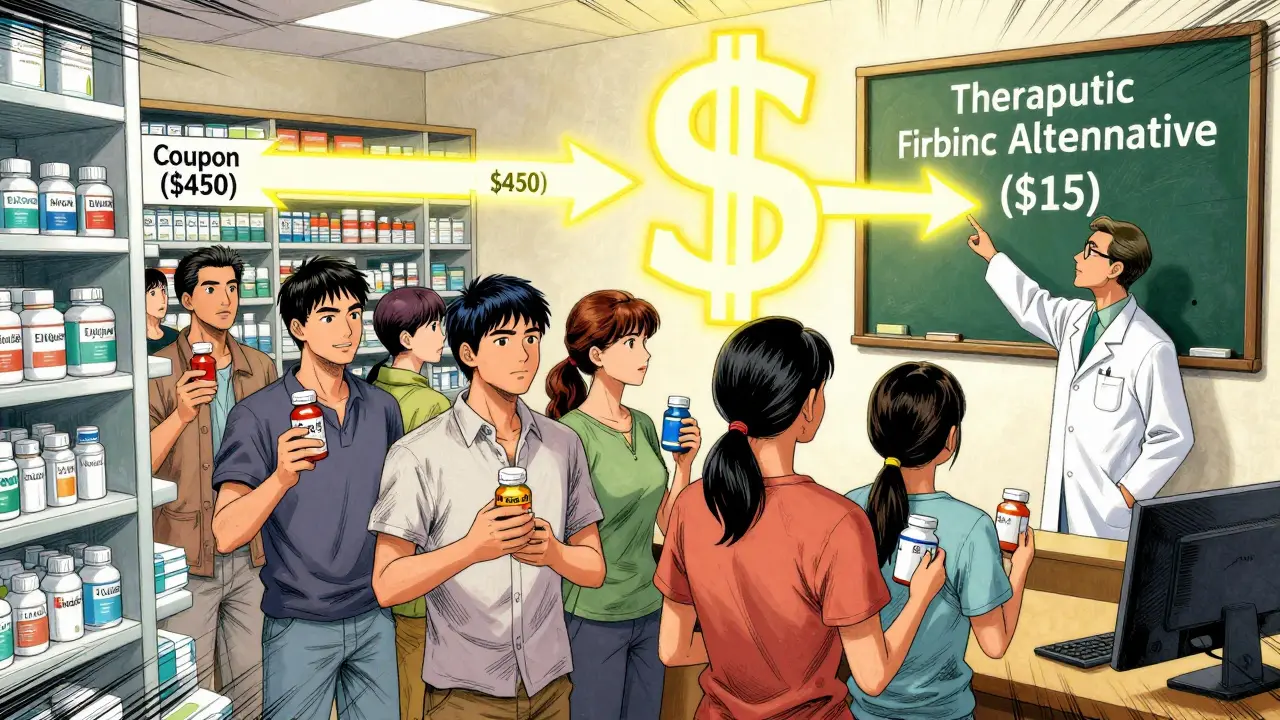
Why This Works Better Than Just Using Coupons
You’ve probably seen ads for GoodRx or manufacturer coupons promising $10 prescriptions. But here’s the catch: those discounts don’t always work. A 2023 JAMA study found that in 24% of cases, your insurance copay was still higher than what the pharmacy pays for the drug. That means the coupon doesn’t help-you’re still paying more than the pharmacy’s cost.
Therapeutic alternatives fix that. Instead of patching a high price with a discount, you replace the expensive drug entirely. And it’s not just for the uninsured. Even people with Medicare or private insurance benefit. A Vanderbilt study showed patients saved $17.77 per person per month on average-without any drop in health outcomes.
Also, coupons only work for brand-name drugs. Therapeutic alternatives work whether you’re on brand, generic, or specialty medication. If your drug has no generic, there’s often another drug in a different class that works just as well.
How to Ask Your Doctor for a Lower-Cost Option
Many patients don’t ask because they assume their doctor already picked the cheapest option. They’re wrong. Most doctors don’t know the price of the drugs they prescribe. A 2023 AAFP survey found that 43% of patients had trouble convincing their provider to consider alternatives.
Here’s how to change that:
- Start the conversation early. Don’t wait until you can’t afford the refill. Bring it up at your next checkup. Say: "I’m having trouble affording my medication. Are there other options that work just as well?"
- Be specific. Don’t just say "it’s too expensive." Name the drug and mention what you’re paying. Example: "I’m paying $450 a month for Lyrica. Is there something similar that costs less?"
- Do your homework. Use GoodRx or a pharmacy’s $4 list (Walmart, CVS, Kroger) to find cheaper alternatives. Print out the price comparison. Bring it to your appointment. Studies show patients who bring price data are 2.5x more likely to get a switch.
- Ask about extended prescriptions. A 90-day supply often costs less than three 30-day refills. Some plans cut copays by 25% for longer supplies.
- Ask for a trial. If your doctor is hesitant, suggest a short trial. "Can we try the alternative for 30 days? If it doesn’t work, I’ll switch back."
Doctors are more likely to agree if you show you’ve done your research. You’re not arguing-you’re collaborating.
When a Therapeutic Alternative Won’t Work
Not every drug has a safe alternative. About 15% of specialty medications-like those for cancer, rare diseases, or advanced autoimmune conditions-have no clinically equivalent options. In those cases, therapeutic interchange isn’t possible.
Also, some people respond differently to drugs. One patient switched from Jardiance to metformin and saw their blood sugar spike. Another switched from pregabalin to gabapentin and had no pain relief. These aren’t failures-they’re individual responses. That’s why your doctor should monitor you after a switch.
If you’ve tried an alternative and it didn’t work, go back. Don’t suffer in silence. Your doctor can help you find another option or apply for patient assistance.
Where to Find Reliable Alternatives
You don’t need to be a medical expert to find cheaper options. Here are the best tools:
- GoodRx - Compares prices at 70,000+ pharmacies. Shows both brand and generic alternatives. Free to use.
- NeedyMeds - Lists free or low-cost drug programs from drug manufacturers. Covers over 1,000 medications.
- Walmart, CVS, Kroger $4 Lists - These pharmacies offer 30-day supplies of common medications (like metformin, lisinopril, atorvastatin) for $4. No insurance needed.
- RxAssist - A nonprofit database of patient assistance programs. Filters by income and condition.
For Medicare patients, ask about tiering exceptions. If your drug is on a high tier, your doctor can request a lower cost-sharing tier if a therapeutic alternative is inappropriate for you. CMS requires these requests to be processed in 72 hours for urgent cases.

Real Stories: What Actually Happens
One patient on Reddit switched from brand-name Lyrica ($450/month) to generic gabapentin. Her neurologist was skeptical-until she showed data from a 2021 study proving they work equally well for neuropathic pain. She now pays $15 a month.
Another, a 68-year-old with high blood pressure, was on a $380/month brand-name drug. Her pharmacist suggested switching to generic atorvastatin. She saved $380/month. Her BP stayed stable. Her doctor called it "the easiest win I’ve seen in years."
But not all stories are smooth. A patient switched from Taltz to methotrexate for psoriasis. The alternative didn’t control her symptoms. She ended up in the ER with a flare-up that cost $18,000. That’s why monitoring matters. Always follow up with your provider after a switch.
What’s Changing in 2026
Things are moving fast. In 2025, the Centers for Medicare & Medicaid Services (CMS) updated rules to require all Part D plans to use standardized criteria for therapeutic interchange. Electronic health records like Epic now have built-in tools that suggest cheaper alternatives at the click of a button. One study showed adoption jumped 15% after these tools were added.
Also, the proposed Lower Drug Costs Now Act could let Medicare negotiate prices for 250 drugs by 2030. But experts warn: even if those prices drop, therapeutic alternatives will still be cheaper. Oliver Wyman estimates negotiated prices will still be 20-40% higher than the cost of a therapeutic substitute.
Expect more states to allow substitution for biologics (currently allowed in only 12). And AI tools are now predicting which patients are most likely to benefit from a switch-with 89% accuracy.
Final Thoughts: You Have Power
You don’t have to accept high drug prices as normal. Therapeutic alternatives are a legal, safe, and widely supported strategy used by top hospitals and clinics. The system is designed to make you feel powerless-but it’s not.
If you’re struggling to pay for your meds, you have three steps:
- Find out what your drug costs at different pharmacies (use GoodRx).
- Look up cheaper alternatives with similar effects.
- Bring that info to your doctor and ask: "Can we try this instead?"
It’s not about being difficult. It’s about being informed. And every time you do this, you’re not just saving money-you’re helping make the system work better for everyone.