Combining tricyclic antidepressants (TCAs) like amitriptyline with common over-the-counter antihistamines like diphenhydramine (Benadryl) might seem harmless - especially if you're trying to sleep better or manage allergies. But for many people, especially those over 65, this mix can trigger something far more dangerous than drowsiness: anticholinergic overload.
What Is Anticholinergic Overload?
Your body uses acetylcholine, a key neurotransmitter, to control everything from memory and attention to bladder function and heart rate. Anticholinergic drugs block this chemical. When just one medication does it, your body can often compensate. But when two or more anticholinergic drugs are taken together - like a TCA and a first-gen antihistamine - the effect stacks up. That’s anticholinergic overload.It’s not rare. A 2020 study in Elsevier found over 6,800 documented cases of high-risk drug interactions involving TCAs and antihistamines. Many of these were in older adults prescribed amitriptyline for nerve pain and diphenhydramine for insomnia. Neither drug was flagged as dangerous alone. Together? They created a perfect storm.
Why TCAs and Antihistamines Are a Dangerous Pair
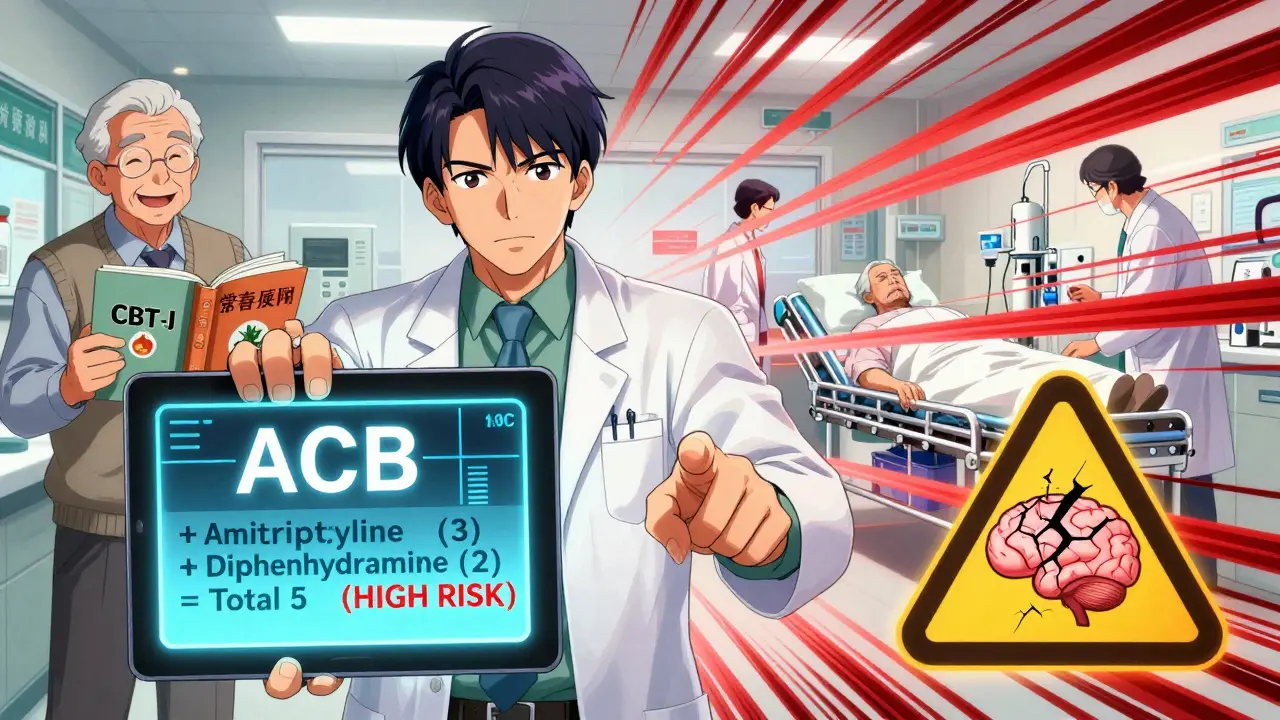
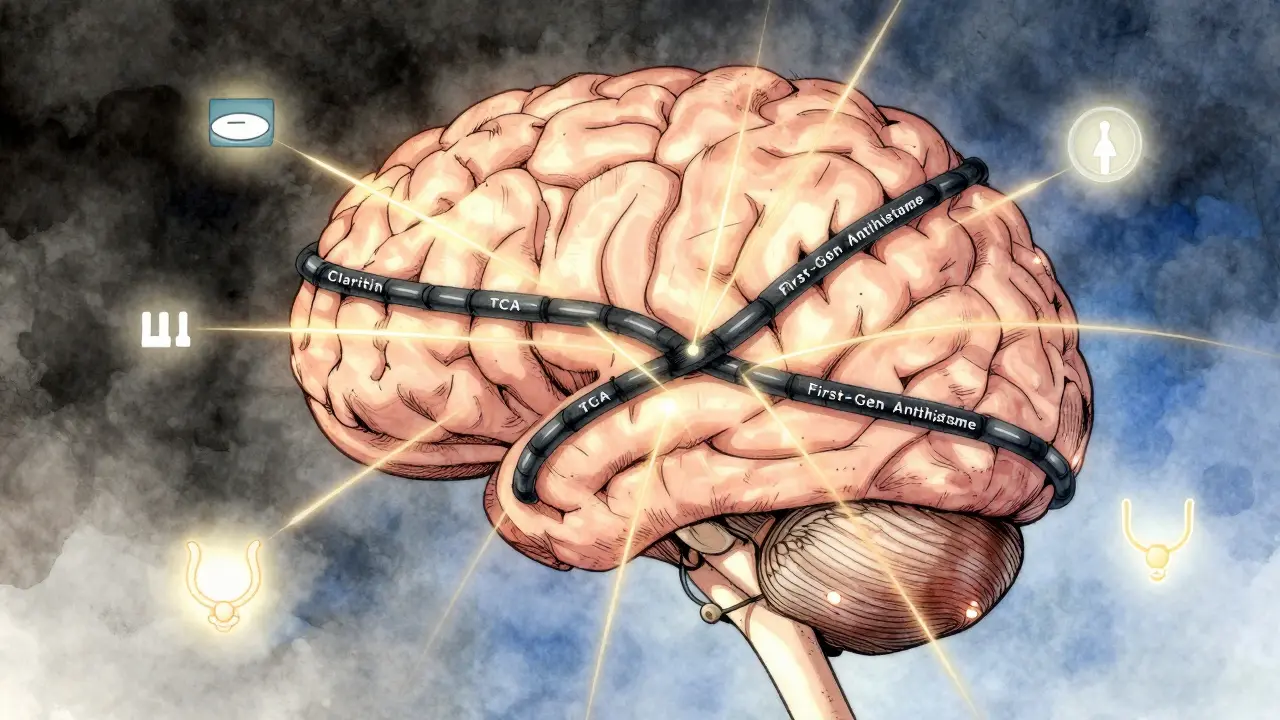
Tricyclic antidepressants were developed in the 1950s. They work by boosting serotonin and norepinephrine, but they also strongly block muscarinic receptors - the same ones targeted by anticholinergics. Amitriptyline, for example, has a binding affinity (Ki) of 8.9 nM for the M1 receptor. That’s high. Diphenhydramine, while weaker individually (Ki of 1,000 nM), is often taken in doses of 25-50 mg, multiple times a day. When you add them up, the total anticholinergic burden becomes toxic.First-generation antihistamines - diphenhydramine, hydroxyzine, chlorpheniramine - are notorious for this. They cross the blood-brain barrier easily and hit the same receptors as TCAs. Second-generation antihistamines like loratadine (Claritin) and cetirizine (Zyrtec)? Almost none of that effect. Their ACB (Anticholinergic Cognitive Burden) score is 0. Diphenhydramine? Score of 2. Amitriptyline? Score of 3. Add them? That’s a 5 - the highest risk category. Research shows a score of 4 or higher doubles your risk of dementia over time.
Who’s at Risk?
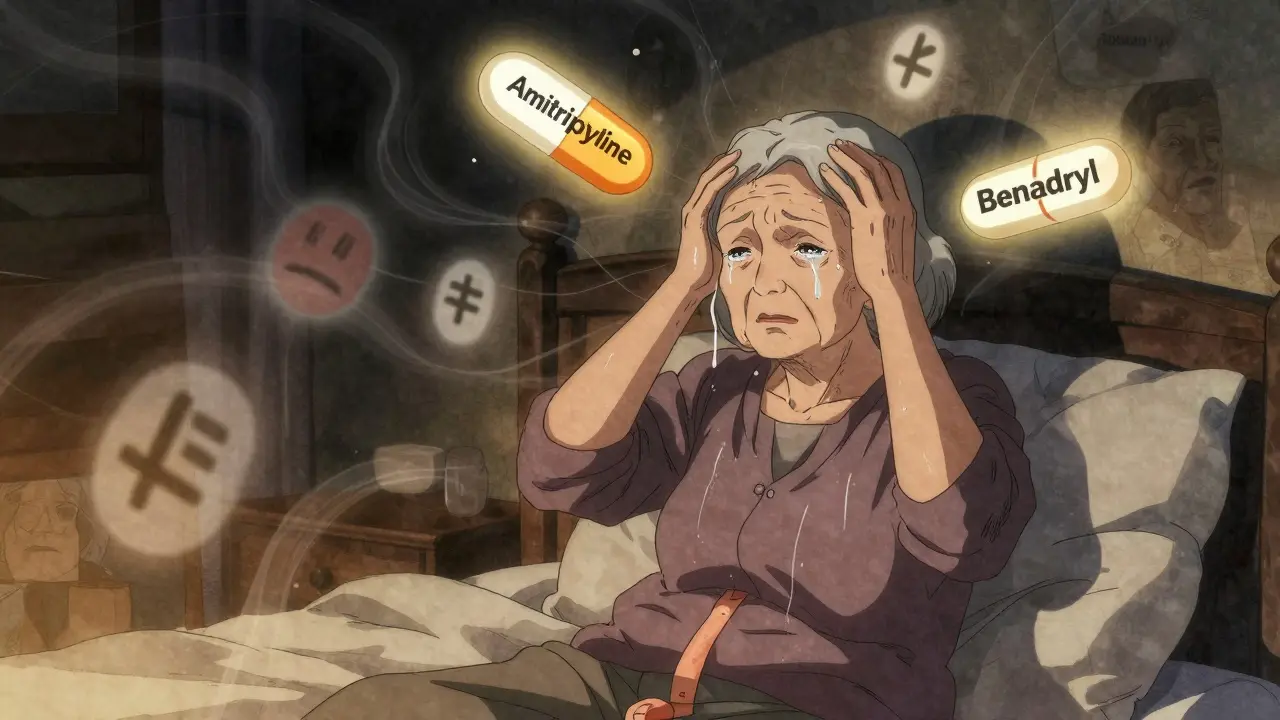
It’s not just seniors. But they’re the most vulnerable. As we age, our liver and kidneys slow down. We metabolize drugs slower. That means these medications stick around longer. A 70-year-old taking amitriptyline 50 mg nightly and diphenhydramine 25 mg for allergies isn’t just sleepy - they’re at risk of confusion, urinary retention, constipation, dry mouth, blurred vision, and even acute delirium.One patient on Psych Forums described being rushed to the ER after her doctor added Benadryl to her amitriptyline for sleep. She ended up with severe confusion and couldn’t urinate. Her doctors called it anticholinergic toxicity. She wasn’t overdosing. She was just taking two common, widely prescribed drugs.
Another case from Reddit’s r/medschool: three elderly patients admitted with sudden delirium, all on TCA + diphenhydramine combinations. Their primary care doctors didn’t see the connection. Neither did the patients - they thought the confusion was just “getting older.”
The Real Cost: Cognitive Decline and Dementia
This isn’t just about short-term side effects. Long-term use of anticholinergic drugs is linked to dementia. A landmark 2015 study in JAMA Internal Medicine found people who took anticholinergics daily for three or more years had a 54% higher risk of developing dementia. The more drugs, the higher the risk. The longer the exposure, the worse the outcome.That’s why the American Geriatrics Society’s Beers Criteria (2023 update) explicitly says: “Avoid first-generation antihistamines in older adults taking TCAs.” It’s not a suggestion. It’s a warning based on decades of evidence.
Even short-term use matters. A 2023 study in the Journal of the American Geriatrics Society showed that just 30 days of combined TCA and diphenhydramine use increased delirium risk by 200% in patients over 65. That’s not a typo. Two full times more likely to become confused, disoriented, or hallucinate - and it can happen in days.
What You Can Do
If you’re taking a TCA - amitriptyline, nortriptyline, imipramine, clomipramine - and you’re also using an OTC sleep aid, allergy pill, or motion sickness medication, stop and ask: Is this necessary?- Check your meds: Look at every pill you take. Is it diphenhydramine, hydroxyzine, chlorpheniramine? If yes, it’s anticholinergic.
- Use the ACB scale: Amitriptyline = 3, diphenhydramine = 2. Add them? 5 = high risk. If your total score is 3 or more across all meds, talk to your doctor.
- Switch antihistamines: Replace Benadryl with loratadine (Claritin), fexofenadine (Allegra), or cetirizine (Zyrtec). They work just as well for allergies and don’t cross into the brain.
- Try non-drug sleep aids: Melatonin (0.5-5 mg), good sleep hygiene, or cognitive behavioral therapy for insomnia (CBT-I) are safer long-term than diphenhydramine.
For pain? Amitriptyline is still a first-line choice for neuropathic pain. But if you’re on it, avoid antihistamines. Period. There are better options for sleep or allergies - and they won’t fog your brain.
What Doctors Are Doing Now
The tide is turning. In 2023, the FDA required all TCA and first-gen antihistamine labels to include clear warnings about cumulative anticholinergic effects. Electronic health records like Epic now block these combinations - if a doctor tries to prescribe them together, the system pops up a hard alert. A 2022 JAMIA study showed 92% of such attempts were flagged.Psychiatrists are catching on too. A 2023 survey found 78% now routinely check anticholinergic burden using the ACB scale - up from just 32% in 2018. The American Geriatrics Society’s “Anticholinergic Burden Audit” has already led to 41% of inappropriate TCA-antihistamine pairs being discontinued in participating clinics.
And research is moving forward. The National Institute on Aging is funding a $2.4 million study (2023-2026) to track how long-term anticholinergic exposure affects memory. Early data suggests even brief exposure can trigger lasting changes in brain function.
What to Ask Your Doctor
If you’re on a TCA and use OTC meds for sleep or allergies, here’s what to say:- “I’m taking amitriptyline. Is the sleep aid I’m using safe with it?”
- “Could this combination be affecting my memory or causing confusion?”
- “Are there non-anticholinergic alternatives for my allergies or insomnia?”
- “Can we check my total anticholinergic burden using the ACB scale?”
Don’t assume your doctor knows. Many still think Benadryl is harmless. They may not realize TCAs are among the strongest anticholinergics in common use. Bring the facts. Be specific. Your brain is worth it.
Alternatives That Work
You don’t have to suffer to be safe.- Allergies: Loratadine (Claritin), fexofenadine (Allegra), cetirizine (Zyrtec) - all ACB score 0. No brain fog.
- Sleep: Melatonin (0.5-5 mg), magnesium glycinate, or CBT-I. No anticholinergic risk.
- Pain: If amitriptyline isn’t working or causing side effects, ask about nortriptyline or desipramine - they’re TCAs with lower anticholinergic activity. Or consider SNRIs like duloxetine, which have minimal anticholinergic effects.
- Depression: SSRIs like sertraline or escitalopram have anticholinergic side effects in only 5-10% of users - compared to 30-50% with TCAs.
For some, TCAs are still the best option. But they shouldn’t be paired with anything that adds to the burden. That’s not medical wisdom - it’s basic pharmacology.
Final Thought: Your Brain Isn’t Replaceable
We’ve been told for decades that Benadryl is safe. That it’s just a sleepy pill. But the science is clear: when it meets a TCA, it’s not just sleepy. It’s dangerous. And it’s not just old people. Anyone taking multiple anticholinergics - even for a few weeks - is at risk.There’s no need to choose between pain relief and sleep. There are safer paths. You just need to ask the right questions - and be ready to change what you’re taking.
Can I take Benadryl with amitriptyline?
No. Combining Benadryl (diphenhydramine) with amitriptyline significantly increases anticholinergic burden, raising the risk of confusion, urinary retention, constipation, delirium, and long-term cognitive decline. Both drugs block acetylcholine, and together they can overwhelm your system - especially if you’re over 65. Switch to a non-anticholinergic antihistamine like loratadine or cetirizine instead.
What are the signs of anticholinergic overload?
Common signs include extreme drowsiness, confusion, memory problems, dry mouth, blurred vision, trouble urinating, constipation, rapid heartbeat, and hallucinations. In older adults, sudden delirium is often the first red flag. If you notice these symptoms after starting or increasing either a TCA or an antihistamine, seek medical help immediately.
Are all antihistamines dangerous with TCAs?
No. Only first-generation antihistamines like diphenhydramine, hydroxyzine, and chlorpheniramine have strong anticholinergic effects. Second-generation antihistamines - loratadine (Claritin), fexofenadine (Allegra), and cetirizine (Zyrtec) - have minimal to no effect on acetylcholine receptors and are safe to use with TCAs.
Can anticholinergic overload cause permanent damage?
Yes. Long-term use of anticholinergic drugs, especially in combination, is linked to an increased risk of dementia. A 2015 JAMA study found a 54% higher risk with chronic use. Even short-term exposure in older adults can trigger delirium that may not fully resolve. Stopping the drugs can help, but prevention is far safer than trying to reverse the damage.
What’s the best sleep aid if I’m on amitriptyline?
Melatonin (0.5-5 mg) is the safest option. It doesn’t interact with TCAs or affect acetylcholine. Cognitive behavioral therapy for insomnia (CBT-I) is also highly effective and drug-free. Avoid diphenhydramine, doxylamine, and any OTC sleep aid that lists “antihistamine” as an active ingredient.
How do I know if I’m on too many anticholinergic drugs?
Use the Anticholinergic Cognitive Burden (ACB) scale. Each drug gets a score: 0 = no effect, 1 = mild, 2 = moderate, 3 = high. Add up all your meds. A total of 3 or more puts you at risk. Amitriptyline = 3, diphenhydramine = 2. If your total is 4 or higher, talk to your doctor about deprescribing.





srishti Jain
December 30, 2025 AT 14:03My grandma took Benadryl with her amitriptyline for years. One day she stopped recognizing us. ER said anticholinergic toxicity. They didn't even know the drugs were the problem.
Nadia Spira
December 31, 2025 AT 12:08Let’s be clear: this isn’t pharmacology-it’s institutionalized geriatric neglect disguised as clinical practice. The medical-industrial complex thrives on polypharmacy because it’s profitable, not because it’s principled. We’ve pathologized aging into a pharmacopeia of iatrogenic catastrophe. The ACB scale? A Band-Aid on a hemorrhage. We need systemic deprescribing protocols, not just ‘switch to Claritin.’ The system is broken, and your melatonin supplements won’t fix it.
Joseph Corry
January 1, 2026 AT 16:10Interesting that you cite JAMA and the Beers Criteria, yet ignore the confounding variables-comorbidities, renal clearance, genetic polymorphisms in CYP enzymes. The ACB scale is a crude heuristic, not a clinical algorithm. Attributing dementia risk to a 5-point score without controlling for baseline cognitive reserve is reductionist at best. Also, loratadine has its own issues with QT prolongation in susceptible populations. Nothing’s risk-free.
kelly tracy
January 1, 2026 AT 16:39So let me get this straight-my doctor prescribed me amitriptyline for chronic pain and said Benadryl was fine for allergies, but now you’re telling me I’ve been slowly poisoning my brain? And no one warned me? This is criminal negligence. I’ve been taking this combo for 7 years. I thought I was just getting older. I’m 58. I’m not ready to be a dementia statistic.
Hayley Ash
January 2, 2026 AT 05:21Wow what a revelation-mixing two drugs that make you sleepy is dangerous? Next you’ll tell me drinking coffee with alcohol gives you a headache. Someone call the FDA. I’m sure the 1950s doctors who invented these drugs were just trolling us
Shae Chapman
January 3, 2026 AT 09:10Thank you for posting this. I’ve been terrified for months after my mom had a delirium episode. I didn’t know it was the meds. I just thought she was ‘acting weird.’ Now I’ve switched her to Zyrtec and melatonin. She’s back to her old self. This needs to be shouted from the rooftops 💔
Cheyenne Sims
January 5, 2026 AT 06:37The American Geriatrics Society’s Beers Criteria is not a suggestion-it is a clinical imperative grounded in decades of peer-reviewed evidence. The conflation of ‘common’ with ‘safe’ is a dangerous cultural fallacy. First-generation antihistamines possess no therapeutic advantage over second-generation alternatives in the treatment of allergic rhinitis or insomnia. Their continued use in geriatric populations represents a failure of medical education and regulatory enforcement. Any clinician who prescribes diphenhydramine to a patient on a tricyclic antidepressant is practicing malpractice by omission.
Colin L
January 5, 2026 AT 08:11I’ve been on amitriptyline for 12 years for fibromyalgia. I used to take Benadryl every night because I couldn’t sleep. I didn’t realize my brain fog wasn’t just ‘stress’-it was the drugs. I lost six months of my life to confusion, forgetting names, forgetting where I put my keys. My wife cried when I finally stopped it. I didn’t know it was reversible. I thought I was just getting old. Now I take melatonin and do breathing exercises. I feel like I got my mind back. I wish someone had told me sooner. I’m not mad-I’m just sad that this isn’t common knowledge.
henry mateo
January 5, 2026 AT 08:23i read this and i thought oh no i take zyrtec and amitriptyline so im good but wait zyrtec is safe right? then i saw the acb scale and i was like oh thank god i didnt know any of this. my doc never mentioned it. thanks for sharing this. i feel like a idiot but also so much more informed now
Kunal Karakoti
January 5, 2026 AT 12:01There’s a deeper question here: why do we treat symptoms rather than root causes? If someone needs antihistamines for allergies, perhaps their immune system is dysregulated. If they need sleep aids, perhaps their circadian rhythm is fractured. We replace one chemical imbalance with another, never asking why the body is signaling distress. The ACB scale is a bandage. We need to ask not ‘what drug to avoid,’ but ‘why are we prescribing so much in the first place?’