Most people with diabetes know their HbA1c number. It’s the number doctors talk about at every checkup. But here’s the problem: HbA1c only tells you what your average blood sugar has been over the last three months. It doesn’t tell you when you spiked after lunch, dropped overnight, or stayed stuck above 200 mg/dL for hours. That’s where Time in Range changes everything.
What Exactly Is Time in Range?
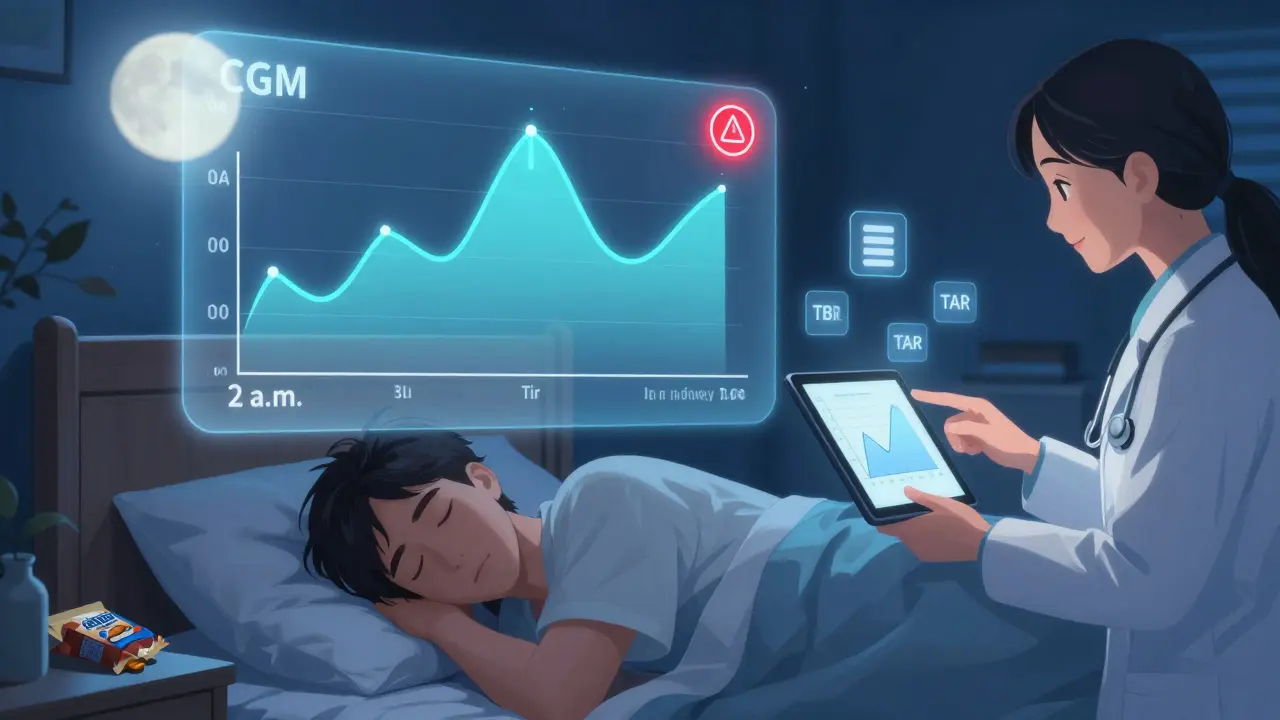
Time in Range, or TIR, is the percentage of time your blood glucose stays between 70 and 180 mg/dL (3.9-10.0 mmol/L). It’s not a guess. It’s not a lab test taken once every few months. It’s real-time data collected by a small sensor worn on your arm or stomach that checks your glucose every 5 minutes - day and night. Over a 14-day period, that’s up to 20,000 data points. And from those numbers, your device calculates exactly how much time you spent in your target zone.
The goal? At least 70% of the day - that’s 17 hours out of 24. That’s not a suggestion. It’s the standard set by the American Diabetes Association (ADA) in their 2025 Standards of Care. Why? Because studies show people who hit this target have lower risks of eye, kidney, and nerve damage. And it’s not just for people on insulin. The ADA now says CGM and TIR should be considered for anyone with type 2 diabetes taking glucose-lowering meds, even if they’re not using insulin.
Why TIR Beats HbA1c Every Time
Imagine two people with the same HbA1c of 7.0%. Sounds perfect, right? But one person spends 85% of their day in range. The other? Only 50%. The second person might be spending 8 hours a day above 180 mg/dL, then crashing below 70 mg/dL at night. Their average looks fine. Their daily reality? A rollercoaster.
HbA1c is like reading the summary of a book. TIR is reading the whole thing. You see the plot twists - the late-night lows, the sugar spikes after a salad, the 3 a.m. highs. You don’t just know your average. You know your pattern.
And here’s the kicker: two people can have identical HbA1c levels but wildly different TIR scores. That’s why relying on HbA1c alone is like driving with blinders on. TIR shows you the road ahead.
The Numbers Behind the Screen
CGM devices don’t just give you TIR. They give you three key metrics:
- Time in Range (TIR): 70-180 mg/dL. Target: ≥70%
- Time Below Range (TBR): Below 70 mg/dL. Target: <4% (less than 1 hour/day)
- Time Above Range (TAR): Above 180 mg/dL. Target: <25%
Some people aim even tighter - Time in Tight Range (70-140 mg/dL). That’s the range most people without diabetes stay in. It’s not the official goal yet, but research is building toward it. A 2025 study in the Journal of Clinical Endocrinology & Metabolism found that even small increases in time spent below 140 mg/dL were linked to better long-term outcomes.
And it’s not just about percentages. CGM also shows your average glucose and how much your numbers swing around - called coefficient of variation. High variability? That’s a red flag. Even if your TIR is decent, wild swings stress your body and raise your risk of complications.
How Real People Use TIR to Take Control
One woman in Melbourne started using CGM after years of guessing what her meals did to her blood sugar. She thought oatmeal was a healthy breakfast. Her TIR data said otherwise - her glucose jumped to 210 mg/dL every morning. She switched to eggs and avocado. Within two weeks, her TIR went from 62% to 81%.
Another man noticed his glucose spiked every night after 10 p.m. He thought it was stress. His CGM showed he was snacking on trail mix before bed. He stopped. His nighttime TBR dropped from 8% to 1%.
These aren’t rare cases. A 2023 study from the Cleveland Clinic found that people using CGM to track TIR improved their HbA1c by an average of 0.8% in just six months - even without changing their medication. The real win? They reported less anxiety, more confidence, and fewer emergency visits.
What You Need to Get Started
You don’t need a PhD to use TIR. But you do need a CGM. The big names - Dexcom, Abbott, Medtronic - all offer devices that work with smartphones and give you clear graphs. Most sensors last 10-14 days. You stick it on, calibrate once (if needed), and let it run. No finger pricks. No waiting for lab results.
Here’s what you need to make it work:
- Get a CGM. If you’re on Medicare or private insurance in Australia, coverage for CGM in type 2 diabetes is expanding fast. Ask your doctor.
- Wear it for at least 14 days. You need at least 70% of the data to be valid. That means don’t rip it off after three days.
- Look at the patterns. Don’t just glance at the daily number. Zoom out. What happens after dinner? After walking? After sleep? Write it down.
- Talk to your diabetes educator. You don’t have to figure this out alone. Diabetes care teams are trained in interpreting TIR data. They can help you adjust food, activity, or meds.
Most people need one or two visits to learn how to read their graphs. After that, it becomes second nature.

Barriers - And Why They’re Falling
Let’s be honest. CGMs used to be expensive. Insurance didn’t cover them for type 2 diabetes. Many people couldn’t afford them. That’s changing. In the U.S., Medicare coverage for CGM in type 2 diabetes jumped from 15% in 2019 to 42% in 2023. Australia’s PBS is expanding access too. Prices for sensors are dropping. Abbott’s FreeStyle Libre is now one of the most affordable options globally.
The market is booming. The global CGM market hit $4.8 billion in 2022. By 2030, it’s expected to hit $18.6 billion. Why? Because doctors and patients alike are seeing the proof: better numbers mean fewer complications, fewer hospital visits, and better quality of life.
What’s Next?
The future of TIR isn’t just about tracking - it’s about predicting. AI tools are being built to look at your data and say: “Your glucose spikes after pasta. Try swapping it for lentils.” Or: “You’re likely to drop low after evening walks. Have a small snack before you go.”
And research is getting more precise. Scientists are now studying how even small increases in Time in Tight Range (70-140 mg/dL) affect long-term health. We’re moving from “good enough” to “what’s optimal.”
One thing’s clear: TIR is no longer a fancy add-on. It’s becoming the new standard - just like HbA1c was 20 years ago. The goal isn’t just to survive with diabetes. It’s to live well. And TIR gives you the map to do that.
Is Time in Range better than HbA1c?
Yes - for daily management. HbA1c tells you your average over three months. TIR shows you exactly when and why your blood sugar goes off track. Together, they give the full picture. But TIR is what helps you make real-time changes to avoid highs and lows.
Do I need to be on insulin to use CGM for Time in Range?
No. The 2025 ADA Standards explicitly recommend CGM for adults with type 2 diabetes on any glucose-lowering medication - even metformin or GLP-1 agonists. You don’t need insulin to benefit from seeing your glucose patterns.
How accurate are CGM devices?
Modern CGMs are very accurate, with most meeting ISO 15197:2013 standards. They’re typically within 10-15% of a lab glucose reading. While occasional calibration is needed (especially with older models), most new sensors like Abbott’s Libre 3 require no finger pricks at all.
Can TIR help prevent diabetes complications?
Evidence strongly suggests it can. Studies link higher TIR with lower risks of retinopathy, kidney disease, and nerve damage. While long-term data is still being gathered, experts agree: spending more time in range reduces the stress on your body - and that’s what causes complications over time.
How long should I wear a CGM to get useful TIR data?
At least 14 days. The 2019 International Consensus says you need at least 70% of your sensor data to be valid - meaning you should wear it almost every day. One week isn’t enough. Two weeks gives you a full picture of how your glucose responds to meals, sleep, stress, and activity.
Are there downsides to using CGM and tracking TIR?
The main ones are cost (though coverage is improving), sensor discomfort for some, and the initial overwhelm of too much data. But most users adapt quickly. The benefits - fewer lows, better sleep, more confidence - far outweigh the challenges. If you’re feeling stuck, talk to a diabetes educator. They’re trained to help you interpret the numbers.






Pat Mun
February 12, 2026 AT 23:38Now I adjust meals based on trends, not guesses. And yeah, I hit 78% TIR last month. Small wins, but they add up.
Robert Petersen
February 13, 2026 AT 15:07Ernie Simsek
February 13, 2026 AT 19:30My A1c’s been 6.8 for 5 years. Why am I paying $300/month for a gadget that tells me what my body’s been doing since 1999? I’ll stick with my glucometer and a napkin full of scribbles.
Sonja Stoces
February 14, 2026 AT 21:00christian jon
February 15, 2026 AT 03:12Alyssa Williams
February 15, 2026 AT 20:27Annie Joyce
February 17, 2026 AT 16:02Jack Havard
February 19, 2026 AT 08:18Neha Motiwala
February 20, 2026 AT 01:51Rob Turner
February 20, 2026 AT 09:35Craig Staszak
February 21, 2026 AT 22:46Luke Trouten
February 22, 2026 AT 12:21alex clo
February 23, 2026 AT 12:58Gabriella Adams
February 25, 2026 AT 11:30athmaja biju
February 27, 2026 AT 04:23