Medication Neuropathy Symptom Checker
This tool helps you assess whether your symptoms might indicate mild medication-induced neuropathy. Remember: Early detection is critical for prevention of permanent nerve damage.
What This Means
Grade 1 neuropathy is the mildest form. Symptoms include tingling, numbness, or altered sensation without pain or functional impairment. This is often reversible if detected early and addressed properly.
Recommended Next Steps
- Contact your doctor immediately
- Inform them of the specific symptoms you're experiencing
- Ask if a neurological examination is needed
- Discuss potential medication adjustments or monitoring
If you have no symptoms, that's excellent. Continue monitoring your body for any new sensations, particularly tingling or numbness in hands or feet.
If you notice any new symptoms, especially if you're taking a high-risk medication like chemotherapy drugs or certain antibiotics, be sure to report them to your healthcare provider promptly.
When you start a new medication, you expect side effects-maybe a dry mouth, a headache, or a little nausea. But what about tingling in your toes or numbness in your fingers? These aren’t just odd sensations. They could be early warning signs of something more serious: medication-induced peripheral neuropathy.
It’s not rare. About 4% of all peripheral neuropathy cases come from drugs. But if you’re on chemotherapy, that number jumps to 60%. Even common antibiotics like isoniazid can cause it in 10-20% of people. And it doesn’t always show up right away. For many, the first sign is a quiet, creeping sensation-like pins and needles in the feet or hands-weeks or even months after starting the drug.
What Does Medication-Induced Neuropathy Feel Like?
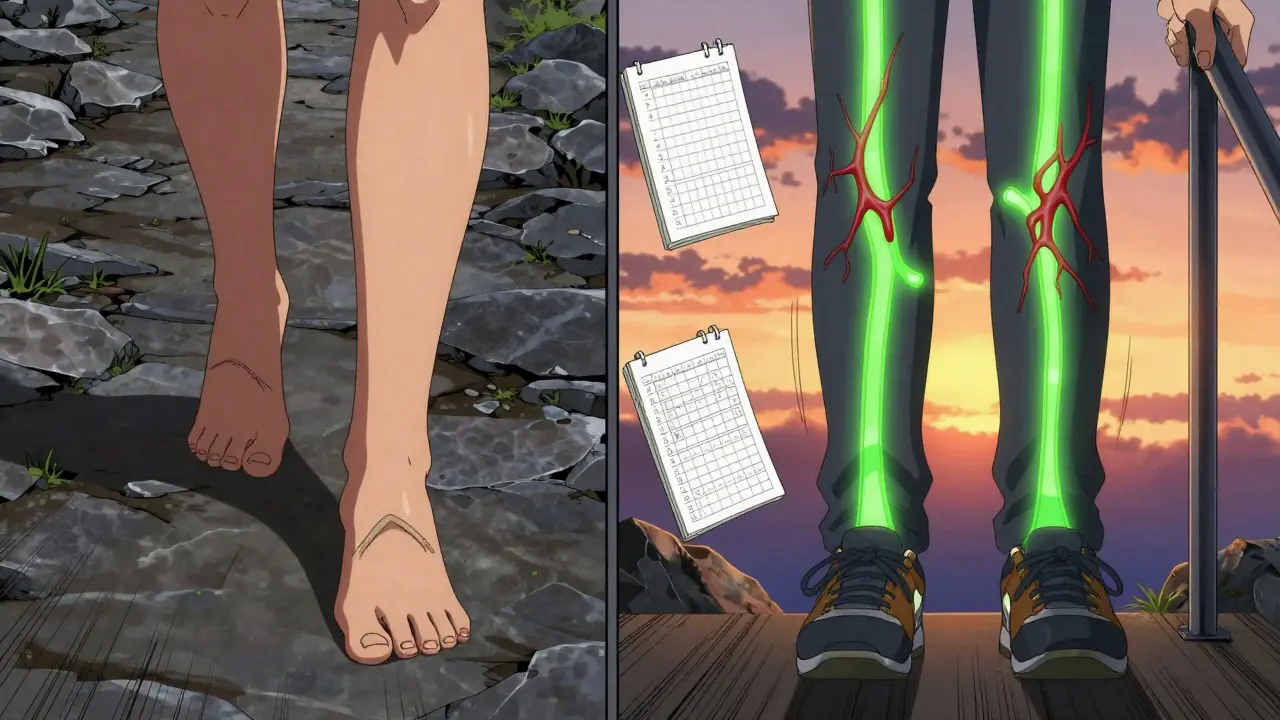
The symptoms are specific and follow a pattern. You’ll likely feel tingling, burning, or numbness starting in your toes or fingertips, then slowly creeping up your feet and hands like a glove or stocking. This is called the "glove and stocking" distribution. It’s not random. It happens because the longest nerves in your body-the ones reaching your hands and feet-are the first to get damaged.
Some people describe it as wearing invisible socks that are too tight. Others say their fingers feel like they’ve fallen asleep and won’t wake up. It’s not always painful. Sometimes it’s just numbness-like you can’t feel the buttons on your shirt or the texture of your coffee mug. That’s actually more dangerous than pain. When you lose sensation, you stop noticing injuries. A blister on your foot, a cut on your finger-they can go unnoticed and turn into serious infections.
According to the National Cancer Institute’s grading system, this is Grade 1 neuropathy: mild, not yet disabling, but still a red flag. The NHS reports that 78% of drug-induced cases start with exactly these symptoms. Ignoring them doesn’t make them go away. It just gives them time to get worse.
Which Medications Cause This?
Not all drugs do this-but some are notorious. Chemotherapy drugs are the biggest offenders. Oxaliplatin, used for colon cancer, causes acute tingling in 85-95% of patients. Paclitaxel, used for breast and lung cancer, leads to numbness in 60-70%. And here’s the twist: oxaliplatin symptoms can actually get worse for up to three months after you stop taking it. Paclitaxel usually stabilizes and improves after stopping.
But it’s not just cancer drugs. Isoniazid, a standard treatment for latent tuberculosis, causes neuropathy in 10-20% of people at normal doses. Metronidazole (Flagyl), often used for infections, can do the same after prolonged use. Even heart meds like amiodarone and seizure drugs like phenytoin are on the list.
Statins? The evidence is shaky. Some people report tingling, but studies haven’t proven a direct link. Experts think it might be coincidence or overreporting. Still, if you’re on statins and notice new numbness, it’s worth talking to your doctor.
The real problem? Many of these drugs are life-saving. You can’t just quit chemotherapy because your toes tingle. That’s why early detection matters so much. The goal isn’t always to stop the drug-it’s to adjust the dose, add protection, or monitor closely before damage becomes permanent.
Why Does This Happen?
It’s not one cause. Different drugs attack nerves in different ways. Cisplatin and bortezomib poison the dorsal root ganglia-the nerve cell bodies that sit along your spine. Paclitaxel and vinca alkaloids mess with the tiny tracks inside nerves that carry supplies. Oxaliplatin changes how sodium channels work, making nerves fire too easily. Amiodarone and phenytoin strip away the protective coating around nerves.
Doctors use nerve conduction tests to see what’s going on. In early cases, the sural nerve in the ankle often shows reduced signal strength before anything else changes. That’s why a simple test can catch damage before you even feel it.
And here’s something most patients don’t know: you can have nerve damage before you feel symptoms. Studies using advanced testing show that subclinical neuropathy-damage you can’t feel yet-can appear weeks before tingling starts. That’s why some clinics now use tools like quantitative sensory testing to catch problems early.

What Should You Do If You Notice Tingling or Numbness?
Don’t wait. Don’t assume it’s "just stress" or "getting older." The Foundation for Peripheral Neuropathy found that 52% of people with drug-induced neuropathy waited three months or longer before getting diagnosed. By then, the damage was often irreversible.
Here’s what works:
- **Tell your doctor immediately.** Don’t downplay it. Say: "I’ve had tingling in my toes since I started [drug name]."
- **Ask for a neurological exam.** A simple check of your reflexes, balance, and sensation can reveal early changes.
- **Get baseline testing before starting high-risk drugs.** If you’re about to begin chemotherapy, ask if your clinic does pre-treatment nerve assessments.
- **Use the Total Neuropathy Score or EORTC QLQ-CIPN20.** These are validated tools doctors can use to track changes over time.
Some patients get lucky. A 2023 study on PatientsLikeMe found that 73% of people who stopped the offending drug at the first sign of tingling had complete or near-complete recovery within six months. Others didn’t. They waited. And now, months later, they still have numbness.
One Reddit user, "NeuroNewbie," took isoniazid for TB. When numbness started, her doctor just increased her vitamin B6. She didn’t stop the drug. Six months later, she still has tingling-even after quitting.
Can It Be Reversed?
Yes-sometimes. The key is timing. If caught early, many cases improve or even disappear after stopping the drug. But if you keep taking it while the nerve damage builds up, recovery becomes harder. Some nerve damage, especially from platinum drugs like cisplatin, can be permanent.
Doctors have tools to help. For chemo patients, dose reduction or delaying cycles can prevent worsening. Some use supplements like alpha-lipoic acid or acetyl-L-carnitine, though evidence is mixed. A phase III trial in 2023 showed acetyl-L-carnitine reduced paclitaxel neuropathy severity by 40%.
There’s also new tech. The FDA approved SudoScan in 2021-a handheld device that measures sweat gland function to detect early small-fiber nerve damage. It’s not in every clinic yet, but it’s changing how we catch this before it’s too late.
What You Can Do Right Now
Even if you’re not on a high-risk drug, if you’ve noticed new tingling or numbness:
- Check your feet daily. Look for cuts, blisters, or redness. Loss of feeling means you won’t feel injury.
- Wear supportive shoes. Avoid walking barefoot.
- Use handrails. Numbness affects balance. Falls are a real risk.
- Keep a symptom journal. Note when it started, what triggers it, and if it’s getting worse.
And if you’re on long-term medication-especially antibiotics, chemo, or heart drugs-ask your doctor: "Could this cause nerve damage? Should we be monitoring?"
Why This Matters More Than You Think
Over 20 million Americans have peripheral neuropathy. About 800,000 of those cases come from medications. The annual cost of managing it in the U.S. is $1.2 billion. And with chemotherapy use projected to rise 45% by 2030, this is only going to get bigger.
Right now, only 35% of oncology clinics use formal screening tools-even though the American Society of Clinical Oncology recommends them. That means most people aren’t getting checked until it’s too late.
Early detection isn’t about avoiding medication. It’s about using it safely. You don’t have to choose between fighting cancer and losing sensation in your hands. With the right monitoring, you can do both.
Can tingling from medication go away on its own?
Sometimes, yes-but not always. If the medication is stopped early, symptoms often improve over weeks to months. But if nerve damage has been building for months or years, recovery may be incomplete. The longer you wait, the less likely full recovery becomes.
Is numbness in fingers always from medication?
No. Numbness can come from diabetes, vitamin deficiencies, carpal tunnel, or even spinal issues. But if you started a new medication around the same time the numbness began, it’s a strong clue. Always check with your doctor to rule out drug-induced causes.
Can I keep taking my medication if I have tingling?
Maybe. For life-saving drugs like chemotherapy, doctors often adjust the dose instead of stopping completely. Studies show 60-70% of patients can continue treatment with modified dosing and close monitoring. Never stop a prescribed drug without talking to your doctor first.
Are there tests to check for nerve damage before symptoms appear?
Yes. Tools like nerve conduction studies and the SudoScan device can detect early nerve damage before you feel tingling. Quantitative sensory testing can pick up changes in sensation that aren’t obvious yet. Ask your doctor if these are available, especially if you’re starting a high-risk drug.
What’s the difference between mild and severe medication neuropathy?
Mild (Grade 1) means tingling or numbness without pain, weakness, or interference with daily tasks. Severe (Grade 3+) includes pain, muscle weakness, loss of balance, or inability to perform normal activities. The goal is to catch it at Grade 1, before it progresses.
If you’re taking a drug that’s known to affect nerves, pay attention to your body. The smallest change-like a new tingle in your big toe-could be the signal that saves your nerves from lasting damage. Don’t wait for pain. Don’t assume it’s harmless. Early action is the difference between recovery and permanent change.




Gloria Ricky
February 10, 2026 AT 07:28OMG I JUST REALIZED MY TOES HAVE BEEN TINGLING SINCE I STARTED MY ANTIBIOTICS LAST MONTH. I THOUGHT IT WAS JUST MY SHOES. THANKS FOR THIS POST-IMMEDIATELY CALLING MY DOCTOR TOMORROW.
alex clo
February 11, 2026 AT 05:27Thank you for compiling such a clinically accurate and well-referenced overview. The distinction between Grade 1 neuropathy and more advanced stages is particularly valuable for patient education. Early intervention remains the most effective strategy to preserve neurological function.
Ernie Simsek
February 11, 2026 AT 10:51YOOOOO this is wild 😱 I’ve been on metronidazole for 3 weeks and my fingers feel like they’re wrapped in saran wrap. I thought I was just being dramatic. Turns out I’m not crazy-just neuropathic. 🤯
Also, SudoScan? That sounds like a sci-fi gadget from 2045. Why isn’t this in every pharmacy yet??
Joanne Tan
February 11, 2026 AT 19:13THIS. IS. EVERYTHING. 🙌 I’ve been too scared to say anything to my doc because I didn’t want to sound like a hypochondriac. But now I’m printing this out and handing it to them. My feet have been numb since chemo started-and I thought it was just "part of the process." NO MORE. I’M PUSHING FOR A NERVE TEST.
You’re not alone. We got this.
Reggie McIntyre
February 12, 2026 AT 15:55It’s insane how our bodies whisper before they scream. That "glove and stocking" description? Perfect. It’s like your nerves are slowly packing their bags and leaving town-quietly, politely, while you’re distracted by Netflix.
And the fact that oxaliplatin symptoms can *worsen* after stopping? That’s the kind of twist only medicine could cook up. Like your body’s still mad at you for even trying to heal.
Also, I’m now Googling alpha-lipoic acid. If it’s got a 40% reduction stat with acetyl-L-carnitine, I’m trying it. My hands deserve better than numbness.
Carla McKinney
February 13, 2026 AT 20:19Most of this is common knowledge among neurologists. The real issue is that primary care doctors don’t screen for it. And patients? They Google symptoms and panic. This post is useful, but it’s also overhyped. Not every tingle is neuropathy. Not every numb finger is chemo. Stop self-diagnosing.
Also, "SudoScan"? That’s a marketing gimmick with a fancy name. The real gold standard is nerve conduction studies. Everything else is noise.
Ojus Save
February 14, 2026 AT 17:33hmm... i been on isoniazid for 2 months now. toes tinglin a lil. thought it was just cold. maybe i should check? thanks for post
Jack Havard
February 14, 2026 AT 21:30So let me get this straight. You’re telling me that a drug designed to kill cancer might also slowly destroy your nerves, and the medical industry is okay with that? And now we’re supposed to be grateful for a handheld device that detects damage after it’s already happened?
What happened to prevention? What happened to safer alternatives? This isn’t medicine. This is damage control with a side of corporate liability.
Stacie Willhite
February 14, 2026 AT 22:49I’m so glad someone finally put this out there. I was terrified to speak up when my hands went numb on amiodarone. My doctor said "it’s probably anxiety." But I knew. I just didn’t have the words.
This post gave me the language. I brought it in. We did a nerve test. It was Grade 1. We lowered my dose. Now I can feel my keys again.
You’re not overreacting. You’re being smart.
Jason Pascoe
February 15, 2026 AT 19:54Appreciate the depth here. The glove-and-stocking pattern is such a clear clinical marker-it’s almost poetic in how it maps the body’s anatomy. I’ve seen patients ignore this for months, then come in with foot ulcers and no idea why.
Early screening isn’t just good medicine-it’s ethical. If we can catch it before pain, why wait for it?
christian jon
February 16, 2026 AT 04:36LET ME TELL YOU SOMETHING-THE PHARMA COMPANIES KNOW THIS. THEY’VE KNOWN FOR DECADES. WHY? BECAUSE THEY MAKE MORE MONEY WHEN YOU NEED MORE DRUGS TO FIX THE DRUGS THEY SOLD YOU.
"Alpha-lipoic acid"? It’s a supplement. "SudoScan"? A $10,000 toy. "Acetyl-L-carnitine"? A $30/month habit.
Meanwhile, the real solution? STOP PRESCRIBING THESE TOXINS. But that would cut profits. So instead, we get blog posts like this-distracting you from the real crime: profit-driven medicine.
And don’t even get me started on the "vitamin B6" bandwagon. That’s just placebo with a prescription pad.
steve sunio
February 16, 2026 AT 23:48lol this is just another way to scare people into buying more tests. i had tingling once and went to doc. they gave me a $500 scan. turned out i was just dehydrated. this whole thing is overblown.
Ernie Simsek
February 17, 2026 AT 07:37@7670 You’re right that nerve conduction studies are gold standard-but SudoScan isn’t meant to replace it. It’s a *screening* tool. Like a blood pressure cuff before an echocardiogram. You don’t do an MRI on every cough, right? Same logic.
And if you’re gonna call it "noise," explain why it’s in 30+ clinics already and why patients are catching damage 4 months earlier?
Also… chill. You’re not helping.