Steroid-Induced Psychosis Risk Calculator
Calculate Your Risk
This tool estimates your risk of developing steroid-induced psychosis based on clinical data from the article.
When someone starts taking high-dose steroids for a flare-up of arthritis, lupus, or asthma, they usually expect relief - not a mental health crisis. But steroid-induced psychosis is real, dangerous, and often missed. It doesn’t happen to everyone, but when it does, it can turn a routine treatment into a life-threatening emergency. Symptoms like confusion, agitation, hallucinations, or sudden paranoia can appear within just a few days. And if you don’t recognize them for what they are, you could be treating a medical side effect like a psychiatric disorder - with the wrong drugs, at the wrong dose, and at the wrong time.
What Exactly Is Steroid-Induced Psychosis?
Steroid-induced psychosis is a documented medical condition, not just a rumor. The DSM-5 classifies it as a substance/medication-induced psychotic disorder. That means it’s caused directly by corticosteroids - not by a pre-existing mental illness. You can’t diagnose it unless you’ve ruled out everything else: drug use, infections, low blood sugar, brain tumors, or electrolyte imbalances. But once those are out of the picture, and psychosis shows up shortly after starting steroids? It’s likely steroid-induced.
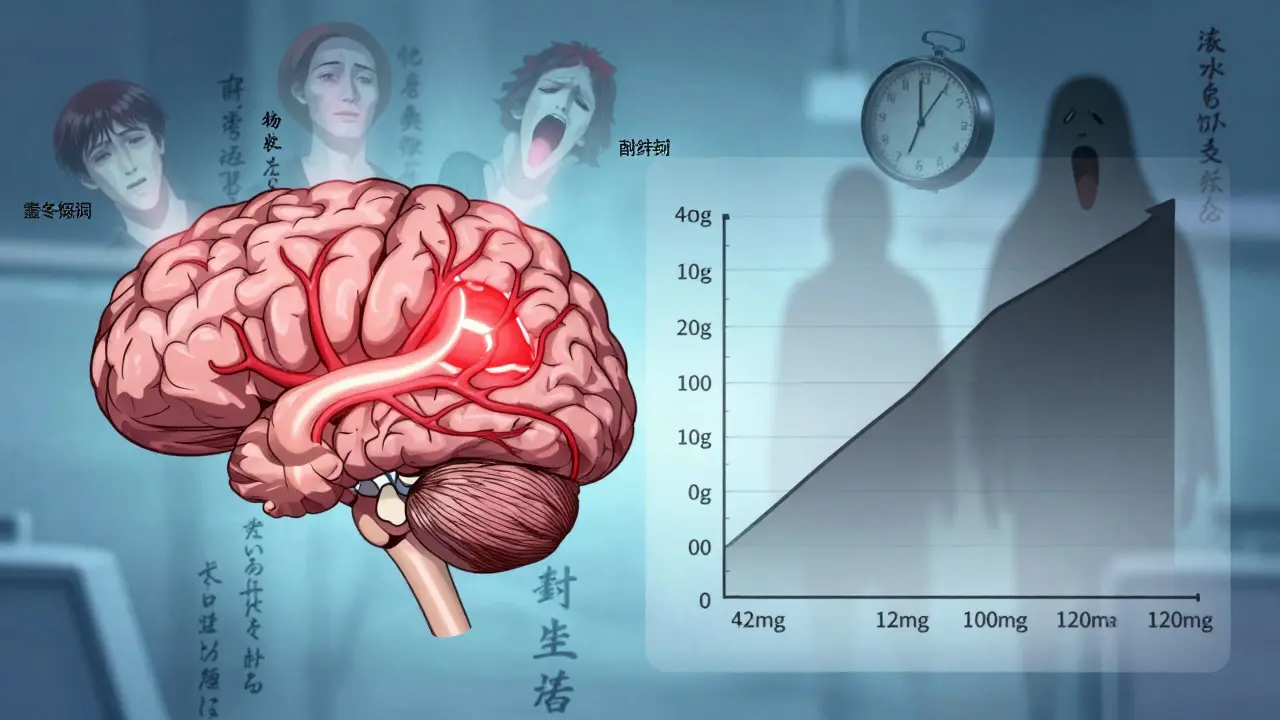
The numbers are startling. Studies show that between 2% and 60% of people on corticosteroids develop some kind of psychiatric symptom. That wide range? It’s because dose matters. At 40 mg of prednisone per day, about 4.6% of patients show signs. Jump to 80 mg or more? That jumps to 18.4%. In other words, if you’re giving someone a high-dose pulse therapy for a severe flare, you’re not just treating inflammation - you’re increasing their risk of losing touch with reality.
What Do the Symptoms Look Like?
It doesn’t start with hearing voices. It starts with confusion. A patient who was coherent yesterday suddenly can’t follow a simple conversation. They’re restless, irritable, or pacing the room. That’s the red flag. Within 1 to 5 days of starting steroids - sometimes even on day two - these early signs appear. If you wait for full-blown hallucinations or delusions, you’ve already missed the window for easy intervention.
Here’s how it typically progresses:
- Days 1-3: Anxiety, sleeplessness, irritability, poor concentration
- Days 3-5: Confusion, disorientation, emotional lability
- Days 5-7: Full psychosis - hallucinations (auditory or visual), paranoid delusions, mania
Some patients get depression. Others get mania. A 1983 review of 79 cases found 28% developed mania, 40% had depression, and 14% had full psychosis. Interestingly, short-term steroid users are more likely to swing into mania. Long-term users? They tend to sink into depression. Both are dangerous. Mania can lead to reckless behavior. Depression can lead to suicide.
Why Does This Happen?
Steroids aren’t just anti-inflammatory drugs. They’re powerful hormones that mimic cortisol, your body’s natural stress hormone. When you flood the system with synthetic versions - like prednisone, dexamethasone, or methylprednisolone - you throw the entire hormonal system out of balance.
Your brain has receptors for cortisol. Too much of it, especially in areas like the amygdala and prefrontal cortex, messes with mood, memory, and judgment. It’s not random. This is the same mechanism that causes mood swings in Cushing’s syndrome (when your body makes too much cortisol naturally) or depression in Addison’s disease (when it makes too little). Synthetic steroids don’t just turn off inflammation - they hijack your brain’s chemistry.
And here’s the kicker: the brain doesn’t distinguish between natural cortisol and the drug version. So when you give someone 100 mg of prednisone, their brain thinks it’s drowning in stress hormones. That’s when logic breaks down.
Emergency Response: What to Do Right Now
If a patient on steroids suddenly becomes agitated, confused, or paranoid - stop assuming it’s schizophrenia. The first rule of emergency management? Rule out medical mimics before you label it psychiatric.
Here’s the emergency protocol:
- Ensure safety. If the person is violent or suicidal, remove weapons, call security, and use verbal de-escalation. Never rely on restraints unless absolutely necessary - they increase trauma and aggression.
- Check the timeline. Did psychosis start within 5 days of starting or increasing steroids? If yes, that’s your biggest clue.
- Run basic labs. Check blood sugar (hyperglycemia is common), sodium, potassium, calcium, and thyroid levels. Infection? Urine culture. Head CT? Only if neurological signs are present. Don’t over-test - just rule out the obvious mimics.
- Start treatment. Two things need to happen at once: taper the steroids and start low-dose antipsychotics.
How to Taper Steroids - Safely
Here’s the most important fact: 92% of patients recover fully when steroids are reduced to under 40 mg/day of prednisone (or equivalent). That’s not a guess. That’s from multiple clinical studies. But you can’t just stop steroids cold.
For someone on 120 mg/day of prednisone for a flare, you don’t drop to zero. You drop to 40 mg. Then hold. Monitor. If symptoms improve, you can slowly taper further over weeks. If they’re on dexamethasone? 6 mg/day is the target ceiling.
Why not go lower faster? Because if the patient needs steroids for adrenal insufficiency, transplant rejection, or severe autoimmune disease, you risk triggering adrenal crisis, organ rejection, or a rebound flare. You’re not curing their disease - you’re managing a side effect while keeping their primary condition stable.
Medications: What Works and What Doesn’t
No drug is FDA-approved specifically for steroid-induced psychosis. But we have strong evidence for what works:
| Drug | Dose (Oral) | Dose (IM) | Notes |
|---|---|---|---|
| Olanzapine | 2.5-20 mg/day | 10 mg IM | Fast-acting, low EPS risk. Disintegrating tablets help with noncompliant patients. |
| Risperidone | 1-4 mg/day | 2-5 mg IM | Good for agitation. Watch for sedation and prolactin rise. |
| Haloperidol | 0.5-1 mg/day | 2-5 mg IM | Effective but high EPS risk. Always give with diphenhydramine or benztropine. |
Don’t use high doses. A 2022 survey found 61% of ER doctors gave 20-30 mg of olanzapine - more than double what’s needed. That’s not more effective. It’s more dangerous. Sedation, low blood pressure, and movement disorders become likely. Stick to the low-dose range. You’re not treating schizophrenia. You’re treating a drug reaction.
Lithium can prevent mania, but it’s risky. It takes weeks to work, needs blood monitoring, and can cause kidney or thyroid damage. Only use it if the patient has recurrent mania and you’ve consulted a psychiatrist.
Antidepressants? SSRIs may help depression. Antiseizure drugs like valproate? Sometimes used for mood stabilization. But evidence is weak. Stick to antipsychotics first.

What Emergency Staff Get Wrong
Most ER doctors know steroids can cause mood changes. But only 43% consistently follow the tapering guidelines. Why? Because they’re scared. They think, “If I reduce steroids, the patient’s lupus will explode.” But here’s the truth: psychosis is more dangerous than a flare. A patient in psychosis can harm themselves, others, or refuse care. A flare can be managed later. Psychosis can kill today.
Another mistake? Delaying treatment. Waiting for “clear psychosis” means waiting until the patient is screaming, hitting walls, or trying to jump out a window. By then, you need heavy sedation, restraints, and possibly police involvement. Catch it early - confusion and agitation are your clues.
The American College of Emergency Physicians updated its guidelines in March 2023: Use 50-75% less antipsychotic than you would for primary psychosis. That’s not a suggestion. It’s a standard.
What’s Coming Next
Researchers aren’t waiting. The NIH is running a study (NCT04876321) tracking 500 patients on high-dose steroids to find genetic markers that predict who’ll develop psychosis. Early data suggests certain variations in cortisol receptor genes make people far more vulnerable.
By mid-2025, the American Psychiatric Association will release a clinical decision tool. It’ll ask: What’s the dose? How long have they been on it? Any past mood disorders? Family history? Then it’ll spit out a risk score and recommend whether to taper, monitor, or add a protective med.
This isn’t science fiction. It’s the next step in making steroid therapy safer.
Bottom Line
Steroid-induced psychosis is treatable. It’s predictable. And it’s often missed. If you’re prescribing or managing steroids - especially at high doses - you need to think about the brain as much as the lungs, joints, or skin. Look for confusion. Look for agitation. Look for changes within the first week. Act fast. Taper the steroid. Start low-dose antipsychotics. Don’t overmedicate. Don’t delay.
It’s not a psychiatric emergency. It’s a medical one. And when you treat it that way, recovery isn’t just possible - it’s almost guaranteed.
Can steroid-induced psychosis happen with low doses?
Yes, but it’s rare. Most cases occur at doses above 40 mg/day of prednisone or equivalent. However, some individuals are unusually sensitive - especially those with a personal or family history of mood disorders. Even 20 mg/day has triggered symptoms in isolated cases. Always monitor for early signs, no matter the dose.
How long does it take to recover after stopping steroids?
Symptoms usually improve within days to weeks after tapering. Most patients see significant relief within 7-14 days. Full recovery typically happens within 4-6 weeks. If symptoms persist beyond 6 weeks, other causes - like an underlying psychiatric disorder - should be re-evaluated.
Is steroid-induced psychosis the same as bipolar disorder?
No. Steroid-induced psychosis is triggered by medication and resolves when the drug is reduced. Bipolar disorder is a chronic brain condition with recurring episodes unrelated to external substances. However, steroids can trigger a first episode in someone predisposed to bipolar disorder - making diagnosis tricky. The key is timing: if symptoms started within days of a steroid dose increase, it’s likely drug-induced.
Can steroids cause psychosis in people with no mental health history?
Absolutely. Many patients have no prior psychiatric history. In fact, studies show about half of all cases occur in people with no prior mental illness. Steroid-induced psychosis doesn’t require a pre-existing condition - it’s caused by the drug’s effect on brain chemistry.
Why not just give more antipsychotics to fix it faster?
Because higher doses don’t work better - they just increase side effects. Studies show low-dose antipsychotics (like 5-10 mg olanzapine) are just as effective as high doses for steroid-induced cases. High doses can cause dangerous drops in blood pressure, extreme sedation, or movement disorders. The goal is symptom control, not sedation. Less is more here.






John Cena
February 19, 2026 AT 17:56