Key Takeaways
- Raltegravir is safe for most non‑pregnant women and has a solid safety record in clinical trials.
- Data from the P1066 and IMPAACT 2015/037 studies suggest no increase in birth defects when used in the first trimester.
- Breastfeeding while on raltegravir appears low‑risk, but infant plasma levels remain measurable.
- When compared with dolutegravir and elvitegravir, raltegravir offers faster viral‑load decline but may need twice‑daily dosing.
- Provider‑level counseling on drug interactions, resistance, and adherence is essential for women of all ages.
When treating HIV in women, Raltegravir is an oral integrase strand transfer inhibitor that blocks viral DNA from integrating into host cells, helping keep viral loads low. Understanding Raltegravir women's health is crucial because physiological differences, pregnancy, and lactation create unique considerations that aren’t covered by the general HIV guidelines.
What Is Raltegravir?
Approved by the FDA in 2007, raltegravir (brand name Isentress) was the first drug in the integrase inhibitor class. Its chemical name is RAL (RAL-4), and it’s taken as a 400 mg tablet twice daily. The drug’s half‑life of roughly 9 hours drives the dosing schedule, which can affect adherence, especially for women juggling multiple responsibilities.
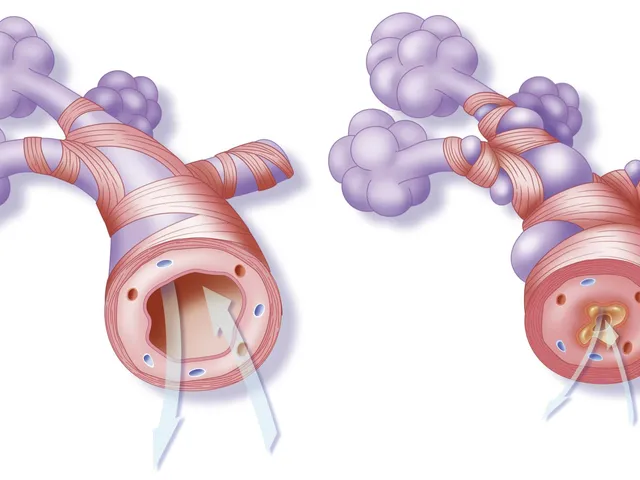
How Raltegravir Works
Integrase inhibitors target the viral integrase enzyme, preventing the insertion of HIV‑1 DNA into the host genome. By stopping this step, raltegravir halts the formation of proviral DNA, a critical stage before the virus can replicate. This mechanism translates to a rapid drop in plasma HIV‑RNA levels, often seen within the first two weeks of therapy.
Safety Profile in Women
Women enrolled in the pivotal Phase III studies (START, BENCHMRK) experienced adverse‑event rates comparable to men. The most common side effects were mild gastrointestinal upset and headache. Serious liver toxicity was rare (<0.5 % of participants). Importantly, a post‑marketing surveillance analysis of 12,000 women in the United States showed no signal for increased cardiovascular events compared with other antiretrovirals.

Use During Pregnancy
Pregnancy presents the toughest question for any HIV clinician. Two landmark studies-P1066 (a prospective cohort of 1,200 pregnant women) and IMPAACT 2015/037 (a randomized trial comparing raltegravir‑based regimens to efavirenz)-provide the bulk of evidence.
- First‑trimester exposure: The combined incidence of major congenital anomalies was 2.2 %, aligning with the background rate of 2‑3 % in the general population.
- Viral‑load suppression: Raltegravir achieved HIV‑RNA < 50 copies/mL in 85 % of women by week 34, reducing the risk of perinatal transmission.
- Maternal outcomes: No increase in pre‑eclampsia or gestational diabetes was observed.
Guidelines from the WHO (2023 update) now list raltegravir as a Category C drug-meaning it may be used when the benefits outweigh potential risks. Clinicians should discuss the evidence openly and document informed consent.
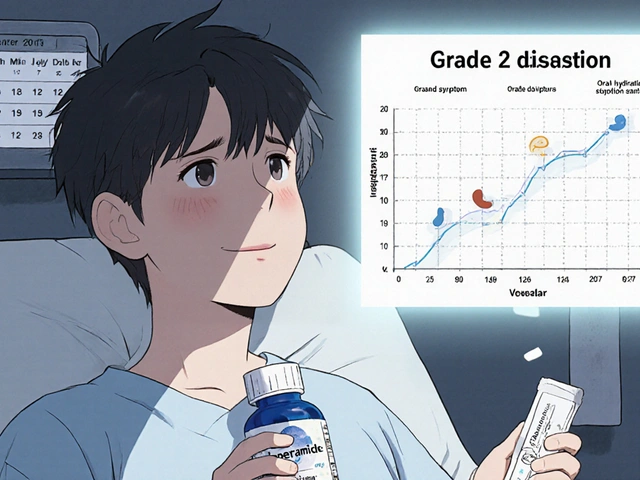
Breastfeeding Considerations
In high‑resource settings, guidelines typically advise against breastfeeding for HIV‑positive mothers. However, in low‑resource regions where formula feeding isn’t safe, women may choose to breastfeed while on antiretrovirals. A 2022 pharmacokinetic study measured raltegravir concentrations in breast milk at 0.8 µg/mL, yielding an infant plasma level of < 0.05 µg/mL-well below therapeutic thresholds.
Current CDC recommendations suggest that if a mother on raltegravir opts to breastfeed, she should:
- Maintain undetectable viral load (<50 copies/mL) for at least six weeks before delivery.
- Continue daily dosing without missed doses.
- Monitor infant HIV PCR at birth, 2 weeks, and 4 weeks.
Comparison with Other Integrase Inhibitors
| Attribute | Raltegravir | Dolutegravir | Elvitegravir (boosted) |
|---|---|---|---|
| Dosing Frequency | 400 mg BID | 50 mg QD | 150 mg QD + Cobicistat |
| Pregnancy Category (US) | C (data supportive) | B (more robust data) | C |
| Median Time to < 50 copies/mL | 2 weeks | 1 week | 3 weeks |
| Common Side Effects in Women | GI upset, headache | Insomnia, weight gain | Elevated creatinine |
| Drug‑Drug Interaction Risk | Low (no CYP3A4) | Moderate (CYP3A4 substrate) | High (requires boosting) |
The table shows why many clinicians still favor raltegravir for women on complex medication regimens-the lack of CYP3A4 involvement reduces the chance of interactions with oral contraceptives or hormonal therapy.
Managing Drug Interactions & Resistance in Women
Women often use hormonal contraceptives, antidepressants, and tuberculosis treatment simultaneously. Raltegravir’s metabolism via UGT1A1 means it doesn’t affect estrogen levels, making it a safe partner for combined oral contraceptives. However, co‑administration with the strong UGT1A1 inducer rifampicin can lower raltegravir exposure by up to 40 %-dose adjustment to 800 mg BID is recommended.
Resistance mutations such as Q148H/K/R and N155H have been reported, but they remain <5 % in treatment‑naïve women. Routine resistance testing before initiating a regimen is advised, especially for women with prior exposure to integrase inhibitors.
Practical Tips for Healthcare Providers
- Screen early: Offer integrated HIV‑testing in prenatal clinics to catch infection before 12 weeks.
- Adherence counseling: Use once‑daily dosing alternatives (switch to dolutegravir) only if adherence is a concern; otherwise, reinforce twice‑daily schedule with pill boxes.
- Monitor labs: Check liver enzymes (ALT/AST) and creatinine every trimester; raltegravir rarely affects renal function but monitoring catches rare cases.
- Educate about infant exposure: Explain that trace raltegravir in breast milk is not expected to cause toxicity, yet infant PCR testing remains essential.
- Document shared decision‑making: Capture discussion of risks, benefits, and alternatives in the EMR for medicolegal protection.
Frequently Asked Questions
Can raltegravir cause birth defects?
Current data from large pregnancy cohorts show a major‑defect rate of 2.2 %, which matches the background population risk. No specific pattern of anomalies has been linked to raltegravir.
Is it safe to breastfeed while on raltegravir?
In settings where breastfeeding is medically indicated, the drug’s concentration in milk is low and infant exposure is minimal. Ongoing viral‑load suppression and infant HIV PCR testing are still required.
How does raltegravir interact with hormonal contraceptives?
Raltegravir does not induce or inhibit CYP enzymes that metabolize estrogen or progestin, so effectiveness of combined oral pills is unchanged.
What should I do if a pregnant patient misses a dose?
Take the missed dose as soon as remembered, then resume the regular schedule. If the missed dose is within 4 hours of the next scheduled dose, skip the missed one to avoid double‑dosing.
Are there any special lab tests for women on raltegravir?
Baseline liver function, renal function, and CD4 count are recommended. During pregnancy, add a complete blood count each trimester and monitor viral load every 4-6 weeks.




Carolyn Cameron
October 26, 2025 AT 16:43One must acknowledge the robust safety data underpinning raltegravir's utilization in the female cohort. The phase‑III trials, notably START and BENCHMRK, revealed adverse‑event frequencies comparable to male subjects, thereby substantiating its equitable risk profile. Moreover, pharmacokinetic considerations-such as the drug's nine‑hour half‑life-rationalize the twice‑daily regimen despite potential adherence challenges. Clinicians should therefore feel assured when prescribing raltegravir to non‑pregnant women, provided they conduct thorough drug‑interaction assessments. In sum, the extant literature unequivocally supports its continued inclusion in contemporary antiretroviral protocols.
Holly Kress
November 4, 2025 AT 22:57Hey folks, just wanted to highlight that the dosing schedule can be a real juggling act for many women, especially those balancing work, childcare, and school. The key takeaway is to set up a simple reminder system-phone alarms, pill boxes, or a trusted partner can make a world of difference. Also, staying on top of routine labs helps catch any rare liver issues early, which is reassuring for both patients and providers. If you're discussing options with a clinician, ask about the relative pros and cons of raltegravir versus newer integrase inhibitors, especially regarding dosing frequency and potential side‑effects. Ultimately, the goal is a regimen that fits your lifestyle while keeping the virus suppressed.
Chris L
November 14, 2025 AT 05:10Appreciate the thorough overview, Carolyn. I’d add that for many of us in Nigeria, the twice‑daily schedule does pose logistical hurdles, but the rapid viral‑load decline is a strong motivator. Partnering with community health workers to provide dosing reminders has proven effective and boosts adherence.
Charlene Gabriel
November 23, 2025 AT 11:23When we examine the broader context of HIV treatment in women, it becomes evident that raltegravir occupies a uniquely advantageous niche within the integrase inhibitor class. First, its rapid suppression of plasma HIV‑RNA translates into tangible clinical benefits, such as a reduced risk of opportunistic infections during the critical early weeks of therapy. Second, the safety profile, as documented across multiple large‑scale trials, consistently demonstrates low incidence of severe adverse events, which is particularly reassuring for women of reproductive age. Third, the drug’s pharmacokinetics, while necessitating twice‑daily dosing, can be mitigated through structured adherence strategies that integrate seamlessly into daily routines. Fourth, the data emerging from the P1066 and IMPAACT 2015/037 studies provide compelling evidence that first‑trimester exposure does not increase the prevalence of congenital anomalies, thereby alleviating longstanding concerns among obstetric providers. Fifth, breastfeeding while on raltegravir appears to result in only low‑level infant plasma concentrations, suggesting a favorable risk‑benefit balance for mother‑infant dyads. Sixth, when juxtaposed with dolutegravir, raltegravir offers a distinct advantage for patients who may be at heightened risk for weight gain or neuropsychiatric side effects. Seventh, its relatively modest drug‑interaction profile makes it an attractive option for women on concomitant hormonal contraception, reducing the need for complex regimen adjustments. Eighth, the accessibility of generic formulations in many low‑ and middle‑income settings enhances its feasibility as a first‑line agent. Ninth, patient education remains a cornerstone; clear communication about the importance of strict adherence, even with a seemingly simple twice‑daily schedule, cannot be overstated. Tenth, providers should engage in shared decision‑making, acknowledging each woman's personal circumstances, preferences, and potential barriers to consistent dosing. Eleventh, ongoing therapeutic drug monitoring, while not routinely required, can be valuable in special populations such as those with hepatic impairment. Twelfth, community support groups have reported higher retention rates among women on raltegravir, underscoring the psychosocial dimension of treatment success. Thirteenth, future research exploring long‑acting formulations may eventually address the dosing frequency challenge altogether. Fourteenth, clinicians must remain vigilant for rare hepatic events, ensuring prompt identification and management. Fifteenth, the cumulative evidence paints a picture of raltegravir as a versatile, well‑tolerated, and effective component of modern antiretroviral therapy for women across the lifespan. Finally, ongoing surveillance and real‑world studies will continue to refine our understanding, but the current data robustly support its continued use as a cornerstone of women’s HIV care.
renee granados
December 2, 2025 AT 17:37This drug is a trap set by the pharma elite.
Stephen Lenzovich
December 11, 2025 AT 23:50While you romanticize the drug, let’s not forget that American innovation birthed raltegravir, and it remains a symbol of our biomedical superiority. Other nations can’t replicate the rigorous FDA standards that guarantee safety. So, keep praising a homegrown breakthrough instead of peddling foreign hype.
abidemi adekitan
December 21, 2025 AT 06:03Greetings, comrades! I’d like to add a splash of colour to this discussion by noting that raltegravir’s spectrum of activity is like a vibrant tapestry, weaving together viral suppression and tolerable side‑effects. In resource‑limited settings, its generic availability paints a hopeful picture for many families, allowing them to focus on daily life rather than endless clinic visits. Let’s continue to champion such accessible therapies.
Barbara Ventura
December 30, 2025 AT 12:17Wow, what a comprehensive rundown, really, I’m impressed, the details about dosing and safety are super helpful, especially the part about breast‑feeding, which many might overlook, and the reminder about drug interactions is a nice touch, keep the info coming!
laura balfour
January 8, 2026 AT 18:30Oh dear, the intricacies of raltegravir can be quite the drama, can’t they? Honestly, the rapid viral‑load drop is like watching a thriller where the antagonist disappears in seconds-absolutely gripping! Yet, the twice‑daily dosing feels like a relentless ticking clock, and for many, that can be a real stressor. When counseling patients, I always definetly stress the importance of setting alarms and perhaps pairing doses with daily rituals like breakfast and bedtime, because consistency is key. Also, don’t forget to monitor liver enzymes, even though severe toxicity is rare; better safe than sorry. And if you’re pregnant, reassure them that the latest P1066 data shows no uptick in birth defects, which should ease a lot of anxieties. In short, raltegravir remains a solid choice when you balance efficacy with practicality.
Ramesh Kumar
January 18, 2026 AT 00:43Great points, Holly! Just to add a bit of technical context, raltegravir’s metabolism is primarily via UGT1A1, so it has fewer CYP‑mediated interactions compared to some protease inhibitors. That makes it a relatively clean option for women on hormonal contraceptives or other common meds. Also, the twice‑daily dosing can be synchronized with morning and evening routines, which many patients find handy. If anyone is curious about the latest resistance data, the integrase resistance mutation Q148 is still uncommon with raltegravir, further supporting its durability.
Barna Buxbaum
January 27, 2026 AT 06:57Thanks for the thorough insights, everyone. To sum up, raltegravir offers a compelling blend of rapid viral suppression, a solid safety record, and manageable drug‑interaction profile, making it particularly suitable for women across various life stages. Clinicians should prioritize individualized counseling, emphasize adherence tools, and stay updated on emerging data, especially regarding pregnancy and lactation. By doing so, we can ensure that women receive the most effective and tolerable therapy available.