It’s easy to assume that if something is labeled natural, it’s safe. But that’s a dangerous myth. Every pill, capsule, or powder you take - whether it’s a prescription drug, an over-the-counter painkiller, or a herbal supplement bought online - carries real, measurable risks. And too many people don’t realize how serious those risks can be until it’s too late.
Supplements Aren’t Tested Like Medications
Prescription drugs go through years of testing before they hit the shelf. They’re evaluated for safety, effectiveness, and how they interact with other drugs. Dietary supplements? Not even close. Under U.S. law, the FDA can’t require supplement makers to prove their products work or are safe before selling them. The burden is on the FDA to prove something is dangerous after people get hurt. That means dangerous products can stay on shelves for months or even years.
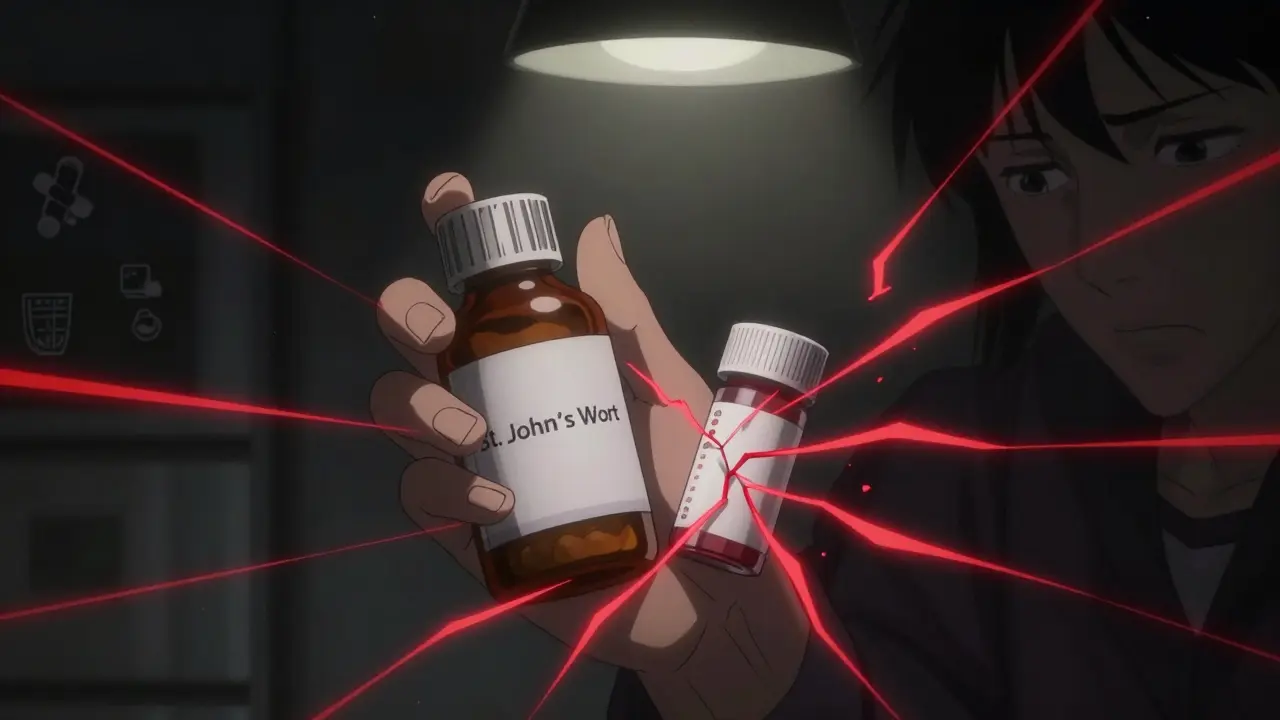
Take St. John’s wort, for example. It’s sold as a natural remedy for mild depression. But clinical studies show it cuts the effectiveness of birth control pills by 13-15%, and drops levels of critical drugs like cyclosporine (used after organ transplants) by up to 60%. That’s not a small risk - it’s life-altering. And because it’s sold as a supplement, you won’t find those warnings on the bottle.
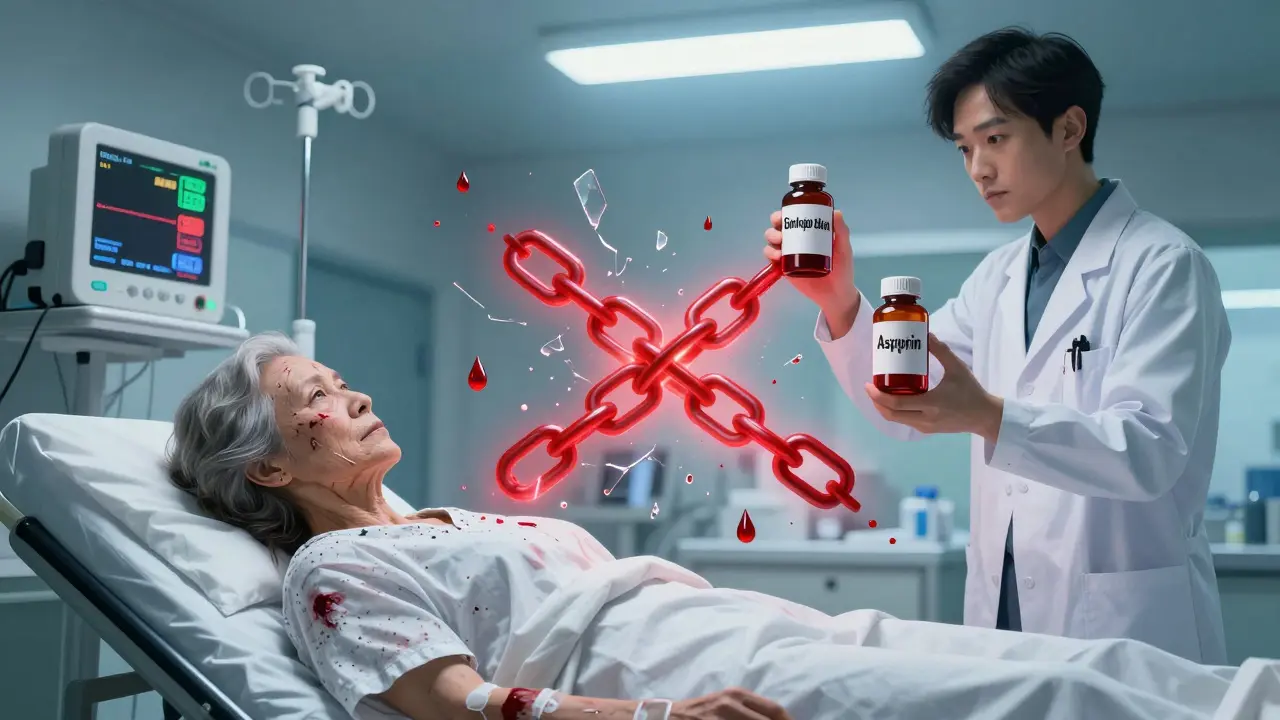
Interactions Can Be Deadly
The real danger isn’t just what a supplement does on its own - it’s what happens when it mixes with your meds. Your body uses enzymes, especially the CYP3A4 system, to break down drugs. Some supplements trick these enzymes into working too fast or too slow.
Asian ginseng speeds up the breakdown of statins, blood pressure meds, and even chemotherapy drugs. That means your treatment might not work. Goldenseal does the same thing. And then there’s ginkgo biloba, garlic, and fish oil - all common supplements that thin the blood. When taken with warfarin or aspirin, they can turn a minor cut into a life-threatening bleed. One woman in her 60s ended up in the ER after taking ginkgo with daily aspirin. She lost so much blood she needed a transfusion.
Even something as simple as vitamin K can be risky. If you’re on warfarin, vitamin K directly counters the drug’s effect. A single high-dose supplement can spike your clotting risk, leading to stroke or heart attack. And if you’re undergoing cancer treatment? Antioxidants like vitamins C and E can reduce chemotherapy effectiveness by 25-30%. That’s not just a theory - oncologists see it happen.
Toxicity Isn’t Just for Overdoses
People think, “I’m just taking a multivitamin,” but even vitamins can be toxic. Vitamin A isn’t harmless. Chronic doses over 10,000 IU a day can damage your liver, cause vision loss, and trigger severe headaches from increased pressure in your skull. Vitamin D isn’t safe either. Taking more than 300,000 IU in a month - which some people do thinking it’ll boost immunity - raises your risk of falls and fractures in older adults by 15-20% because of calcium overload.
Vitamin E at doses above 400 IU a day increases your chance of a hemorrhagic stroke by about 10%. Green tea extract, often taken for weight loss, is now linked to over 20% of all supplement-related liver injuries in the U.S. And bitter orange, found in many weight-loss supplements, can raise blood pressure by 10-15 mmHg and trigger irregular heartbeats. One Reddit user reported severe insomnia and heart palpitations after taking ashwagandha with his blood pressure medication. He didn’t tell his doctor - and nearly ended up in the hospital.
What You Don’t Know Can Kill You
Half of American adults take dietary supplements. But only one in three tells their doctor about it. That’s the biggest problem. Doctors can’t protect you from interactions if they don’t know what you’re taking. A 2022 FDA survey found that 67% of dangerous interactions happen because patients didn’t disclose supplement use.
And it’s not just pills. Many supplements are sold online with no quality control. A 2023 analysis found that 45% of adverse events came from products bought on Amazon, eBay, or shady websites. Some contain hidden pharmaceuticals - like erectile dysfunction drugs or steroids - not listed on the label. Others have inconsistent doses. One batch of turmeric might have 50mg of curcumin; the next might have 500mg. No one’s checking.
High-Risk Groups Are Most Vulnerable
Older adults are at the highest risk. They’re more likely to take multiple medications, have slower metabolism, and use supplements for joint pain, sleep, or memory. A 72-year-old woman on blood thinners and a beta-blocker started taking ginkgo for “brain health.” Within weeks, she had bruising all over her legs and dizzy spells. Her doctor found her INR level - a measure of blood clotting - had tripled.
Cancer patients are another high-risk group. Many believe supplements will help them recover faster. But studies show 40% of common supplements interfere with chemo or radiation. One patient’s radiation treatment was delayed for three weeks because vitamin E caused severe skin burns during therapy. Her oncologist told her: “If you want to take something, let me approve it. Otherwise, stop everything.”
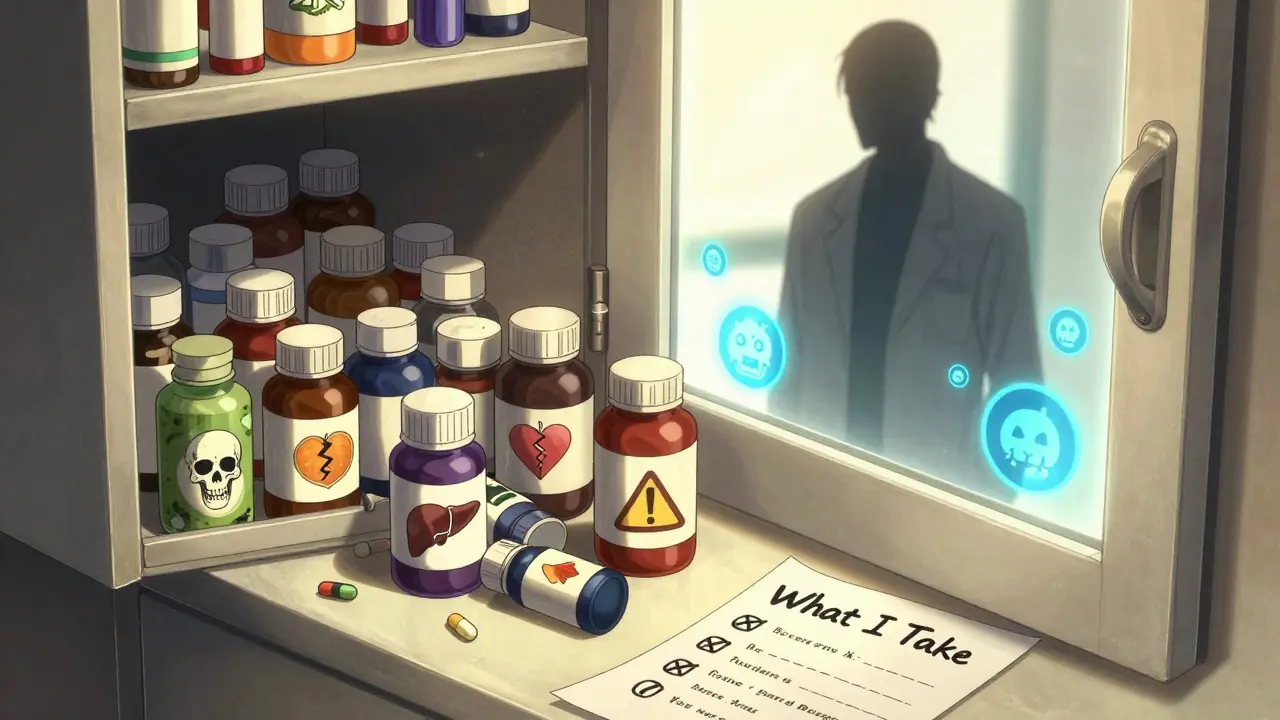
What You Can Do to Stay Safe
There are clear steps you can take - right now - to reduce your risk.
- Make a full list of everything you take. Include prescriptions, OTC meds, vitamins, herbs, probiotics, and even topical creams. Update it every time you see a doctor.
- Bring the list to every appointment. Don’t assume your doctor knows what you’re taking. Show them the bottles. Take photos if needed.
- Ask: “Could this interact with my meds?” Don’t just ask if it’s safe. Ask specifically about interactions. If your doctor doesn’t know, ask them to check.
- Avoid supplements during cancer treatment, surgery, or pregnancy. Unless your specialist says it’s okay, stop everything.
- Buy from reputable brands. Look for third-party testing seals like USP, NSF, or ConsumerLab. Avoid products with “proprietary blends” - they hide ingredient amounts.
- Report bad reactions. If you feel sick after taking something, stop it and report it to the FDA through MedWatch Online. Your report could help save someone else’s life.
The Bottom Line
There’s no such thing as a risk-free supplement. Every active ingredient has a biological effect - and that effect can clash with your body’s chemistry. The FDA doesn’t regulate supplements like drugs because of outdated laws. That means you’re the last line of defense.
You wouldn’t mix cleaning chemicals without reading the labels. Why treat your body any differently? Your health isn’t a gamble. Don’t assume safety because something is labeled “natural.” Ask questions. Be specific. Document everything. And never, ever take a supplement without telling your doctor.
Are dietary supplements safer than prescription drugs?
No. Prescription drugs go through years of clinical trials to prove safety and effectiveness before approval. Supplements are not required to prove anything before being sold. The FDA can only act after harm occurs, which often means dangerous products stay on shelves for years. Many supplements contain potent compounds that can cause serious side effects or deadly interactions with medications.
Can I take supplements while on blood pressure medication?
Some can be dangerous. Ginseng, garlic, ginkgo, and bitter orange can interfere with blood pressure control. Ginseng may reduce the effectiveness of calcium channel blockers. Bitter orange can raise blood pressure by 10-15 mmHg and trigger irregular heart rhythms. Always consult your doctor before taking any supplement if you’re on blood pressure medication - even if it’s labeled “natural.”
Why do some supplements cause liver damage?
Many herbal supplements contain complex plant chemicals that the liver must process. Some, like green tea extract, kava, and comfrey, are directly toxic to liver cells. Others cause immune reactions that inflame the liver. The NIH’s LiverTox database lists 45 supplement ingredients linked to liver injury. Green tea extract alone accounts for 22% of reported cases. Symptoms include yellow skin, dark urine, nausea, and fatigue - often mistaken for the flu.
Is it safe to take vitamins in high doses?
No. Vitamins are not harmless at high doses. Vitamin A can cause liver damage and vision loss at doses over 10,000 IU daily. Vitamin D can lead to dangerous calcium buildup, causing kidney stones, confusion, and heart rhythm problems. Vitamin E above 400 IU daily increases stroke risk. Even water-soluble vitamins like B6 can cause nerve damage at doses over 100 mg per day. More is not better - it’s riskier.
What should I do if I think a supplement is making me sick?
Stop taking it immediately. Contact your doctor or go to the ER if you have symptoms like chest pain, trouble breathing, severe rash, jaundice, or bleeding. Then report the reaction to the FDA through MedWatch Online. Your report helps track dangerous products and may prevent others from being harmed. Don’t wait - adverse events are underreported, and your input matters.
Do I need to tell my doctor about supplements I’ve stopped taking?
Yes. Supplements can linger in your system. St. John’s wort can affect drug metabolism for up to two weeks after you stop taking it. Ginkgo can increase bleeding risk for days. Even if you think you’re no longer using something, your doctor needs to know your full history - especially before surgery, starting a new medication, or during cancer treatment.
Are “organic” or “non-GMO” supplements safer?
No. These labels refer to how ingredients are grown or processed, not safety or effectiveness. An organic supplement can still contain toxic herbs, hidden drugs, or dangerously high doses. Labels like “organic,” “non-GMO,” or “all-natural” have no regulatory meaning when it comes to drug interactions or toxicity. Always check the ingredient list and dose - not the marketing.
What to Do Next
Start today. Pull out your medicine cabinet. Write down every pill, capsule, and powder you take - even the ones you only use occasionally. Bring that list to your next doctor’s visit. Ask one question: “Could any of these interact with my other meds?” Don’t wait for a problem to happen. Prevention is simple - but only if you act.




Bob Cohen
January 31, 2026 AT 15:28Look, I get it - ‘natural’ sounds like a free pass to feel good about popping pills. But honestly? I used to think that too. Then my grandma ended up in the ER because she was taking garlic pills with her blood thinner. No one warned her. Not the store, not the label, not even her ‘wellness coach.’
Bottom line: if it changes how your body works, it’s medicine. Doesn’t matter if it comes in a bottle labeled ‘herbal harmony’ or ‘ancient wisdom.’
Thanks for laying this out. Someone needed to say it without the corporate fluff.
Ishmael brown
February 2, 2026 AT 15:20😂😂😂 ohhhhh so now the FDA is the guardian of our ‘natural’ rights? 🤡
Let me guess - next they’ll ban sunlight because ‘too much UV can cause skin cancer’? 😭
Meanwhile, Big Pharma is still selling you cancer drugs that cost $10,000 a pill and come with a 12-page warning label. But hey, at least they’re ‘tested.’ 😌
Meanwhile, I’ll keep my turmeric, ashwagandha, and lemon water. My body’s been telling me it’s fine. The FDA? Not so much.
Aditya Gupta
February 3, 2026 AT 13:06Bro, i took ashwagandha for stress. Then my bp spiked. Didn’t think it’d do that. Told my doc, he said ‘stop it.’ Done. No drama.
Just talk to your doc. Not Reddit. Not Instagram. Not your auntie who ‘heals with crystals.’
Simple. Real. No fluff.
Nancy Nino
February 4, 2026 AT 16:21While I appreciate the sentiment behind this post, I must emphasize that the underlying assumption-that consumers are somehow ignorant or negligent-is both patronizing and statistically misleading. Many individuals consult with licensed naturopathic practitioners, pharmacists, or integrative medicine specialists who are trained to evaluate herb-drug interactions.
Moreover, the FDA’s regulatory gap is not a failure of consumer awareness but a failure of legislative modernization. Blaming the patient for not knowing the intricacies of CYP3A4 metabolism is like blaming someone for not understanding quantum physics before they take a taxi.
Let’s hold the system accountable, not the people.
Jaden Green
February 5, 2026 AT 22:37It’s amusing how this post treats supplements like they’re some novel, uncharted frontier of medical danger. The truth is, the entire pharmacological industry is a glorified lottery. Every drug approved by the FDA has been linked to fatal adverse events in post-marketing surveillance. The only difference is that pharmaceutical companies have lobbyists who write the laws, while herbalists are just… people who grow plants.
And let’s not forget that ‘clinical trials’ are often funded by the very companies selling the drugs. The data is selectively published. The long-term effects? Buried. The side effects? Minimized in the marketing.
So yes, supplements are unregulated. But so is the entire system. You’re just more comfortable blaming the guy who buys turmeric than the guy who invented statins and then told you to take them for 40 years while ignoring diet, sleep, and stress.
It’s not about safety. It’s about control.
Angel Fitzpatrick
February 7, 2026 AT 10:14They don’t want you to know this - but the FDA and Big Pharma have been suppressing research on natural compounds since the 1950s. Why? Because if people started using turmeric instead of NSAIDs, or magnesium instead of blood pressure meds, the multi-billion dollar drug model collapses.
St. John’s Wort? It’s been shown in 37 peer-reviewed studies to be as effective as SSRIs for mild depression - but they buried it. Why? Because SSRIs are patented. Natural compounds can’t be owned.
And those ‘third-party testing seals’? USP and NSF? They’re funded by supplement companies. The same ones that lobby Congress to keep the DSHEA law intact. You think they’re protecting you? They’re protecting their profit margins.
Meanwhile, the FDA quietly approves new synthetic drugs every week - drugs that cause liver failure, suicidal ideation, and sudden cardiac death - and calls them ‘safe’ because they passed Phase 3 trials that lasted six months.
Wake up. This isn’t about safety. It’s about corporate control over your biology.
Nidhi Rajpara
February 7, 2026 AT 12:23Thank you for this comprehensive and meticulously researched article. I particularly appreciated the emphasis on disclosing supplement use to healthcare providers. As a registered nurse with over 15 years of experience in cardiology, I have encountered multiple cases where patients presented with unexplained bleeding, arrhythmias, or hepatotoxicity-all traceable to undisclosed herbal supplement use.
It is imperative that patients understand that ‘natural’ does not equate to ‘non-pharmacological.’ Every bioactive compound interacts with human physiology, regardless of its origin.
I encourage all readers to maintain a written, updated supplement log and to bring it to every clinical encounter. Your life may depend on it.
Chris & Kara Cutler
February 7, 2026 AT 13:02YES. This. My mom took vitamin E with her chemo and her oncologist had to pause treatment for 3 weeks. She didn’t even realize it was a problem. 😭
Now we have a color-coded chart on the fridge. Pills. Supplements. Herbs. All labeled. All checked. All shared with the team.
You’re not being paranoid. You’re being smart. 💪❤️
Donna Macaranas
February 8, 2026 AT 22:58I used to take everything. Multivitamins, omega-3, magnesium, ashwagandha, melatonin, probiotics… I thought I was being ‘proactive.’
Then I started getting weird migraines and heart flutters. Didn’t think much of it.
My doctor asked me to stop everything for two weeks. Just… nothing.
The migraines vanished. The flutters stopped.
I started back with just one thing at a time. Now I only take vitamin D (because my levels were low) and magnesium glycinate. Everything else? Gone.
Turns out, my body didn’t need all that junk. Just… less.