When a patient walks into the pharmacy with a prescription for a biologic drug like Neulasta or Humira, they’re not just getting medicine-they’re stepping into a complex system of science, regulation, and trust. And the pharmacist? They’re the one holding the keys to making it all work. Unlike generic pills that are chemically identical to their brand-name versions, biosimilars are made from living cells. They’re incredibly similar to the original biologic-but not exact copies. That’s why counseling isn’t optional. It’s essential.
What Makes Biosimilars Different from Generics?
People often assume biosimilars are just like generics. They’re not. A generic version of a drug like lisinopril is a perfect chemical match to the brand. You can swap it in without a second thought. Biosimilars? They’re like a handcrafted replica of a luxury watch. Same function. Same precision. But made with different tools, materials, and processes. Because they come from living cells-like bacteria or yeast-tiny variations happen naturally. The FDA doesn’t require them to be identical. They just need to show no clinically meaningful difference in safety, purity, or potency. That’s why interchangeability matters. Only a handful of biosimilars in the U.S. have been designated as “interchangeable” by the FDA. That means a pharmacist can swap them for the original drug without calling the doctor. As of late 2023, only a few, like the pegfilgrastim biosimilar for Neulasta, had that status. The rest? Even if they’re approved, substitution still needs the prescriber’s okay. That’s a big reason adoption has been slow.Why Pharmacists Are the Missing Link in Biosimilar Adoption
Biologics make up just 2% of all prescriptions in the U.S.-but they cost half of all prescription drug spending. That’s a massive opportunity to cut costs. Yet, doctors often don’t push biosimilars. Why? They’re busy. They’re not trained in the details. And many still worry about safety, even though the FDA says biosimilars are just as safe. Pharmacists, on the other hand, are the ones who see the whole picture. They know the supply chain. They track batch numbers. They understand state laws. And they’re the ones who actually talk to patients. A 2022 study showed that 87% of pharmacists recommended biosimilars to patients-compared to only 62% of physicians. Why? Because pharmacists get continuing education on biosimilars. Nearly 80% have taken courses on them. Only 43% of doctors have. At the US Oncology Network, when they flipped the script-letting pharmacists handle substitution instead of waiting for doctors to approve each switch-adoption jumped fast. Before, doctors had to manually approve every change. After? Pharmacist-led substitution made the process automatic. Within months, nearly all patients on Neulasta were switched to the biosimilar. And clinic interruptions? Cut to zero.How Pharmacists Counsel Patients-Without Scaring Them
Patients hear “biosimilar” and think “cheaper version.” That’s not wrong-but it’s incomplete. The real fear? “Will this make me sicker?” “Will my body reject it?” “What if I switch back and forth?” Good counseling starts with clarity. Pharmacists explain: “This isn’t a generic. It’s been tested in clinical trials. The FDA says it works the same way. The only difference is the manufacturer.” They point to the data: over 15 years of global use, no new safety issues have shown up with biosimilars. They mention that switching between the original and biosimilar-even multiple times-has been studied. No increased risk of side effects. One pharmacist in Melbourne shared a simple trick: “I show patients the FDA’s 9 Things to Know about Biosimilars. I read it with them. When they see it’s from the same agency that approved their original drug, it clicks.” But there’s a catch. Appearance matters. If the new biosimilar pill is a different color, shape, or size-even if it’s the exact same dose-patients are 21% more likely to stop taking it. That’s why pharmacists don’t just hand over the box. They say: “I know this looks different. Let me explain why it’s safe.”
The Rules: What Pharmacists Must Know Before Substituting
Not every state lets pharmacists substitute biosimilars on their own. As of October 2023, 48 states have laws on biosimilar substitution-but the rules vary wildly. Some require the prescriber to opt out in writing. Others require the pharmacist to notify the doctor within 24 hours. A few still don’t allow substitution at all unless the drug is officially interchangeable. Here’s what every pharmacist needs to check before swapping:- Is the biosimilar designated as “interchangeable” by the FDA?
- Does my state law allow automatic substitution?
- Has the prescriber marked “dispense as written” on the prescription?
- Can I trace the batch number? (This isn’t optional-it’s required for safety tracking.)
Barriers Still Standing in the Way
Even with all the evidence, adoption is still slow. Why? First, money. Some pharmacy benefit managers (PBMs) still get bigger rebates from the original biologic makers. That means the cheaper biosimilar isn’t always the most profitable option for the system-even if it’s better for the patient. Second, education gaps. A 2022 survey found that 79% of pharmacists said they needed more training on billing and reimbursement rules. If you don’t know how to code the substitution correctly, the claim gets denied. The patient gets billed. The system breaks down. Third, prescriber resistance. One pharmacist on Reddit shared: “I switched a patient’s Humira to a biosimilar. The doctor called me furious. Now he writes ‘do not substitute’ on every biologic script.” That’s not rare. Some doctors still believe biosimilars are “second-rate.” That’s outdated. But it’s real.
What Works: Real Strategies That Move the Needle
At US Oncology, they didn’t just change the rules. They changed the culture. They made every staff member-doctors, nurses, pharmacists, financial counselors-take a mandatory e-learning module on biosimilars. They got written consent from every prescriber agreeing to automatic substitution. They trained pharmacists to document every switch in the electronic record. And they tracked results. Within a year, biosimilar adoption went from 12% to 89%. The key? They made it easy. No more phone calls. No more delays. No more confusion. The pharmacist did the work. The doctor kept doing what they do best: treating patients.The Future: Pharmacists as Biotherapeutics Specialists
The market for biologics is growing. More biosimilars are coming. More conditions are being treated. And as that happens, the role of the pharmacist is evolving. We’re not just dispensing pills anymore. We’re becoming specialists in complex therapies. The science is clear: biosimilars are safe. The data shows: pharmacists drive adoption. The system needs: clear rules, better education, and trust. The next step? Pharmacy schools should add biosimilar training to their core curriculum. States should update their laws to reflect the science, not the fear. And every pharmacist should feel empowered to say: “I know this works. Let me help you.”Can a pharmacist automatically substitute a biosimilar without the doctor’s permission?
Only if the biosimilar has been officially designated as "interchangeable" by the FDA and your state’s pharmacy laws allow it. As of late 2023, only a few biosimilars-like the pegfilgrastim version of Neulasta-have that status. For all others, the prescriber must either allow substitution or not mark "dispense as written." Pharmacists must follow state-specific rules before making any switch.
Why are biosimilars more expensive than generics?
Biosimilars are made from living organisms, not chemicals. That means the manufacturing process is far more complex and expensive than producing a generic pill. While they still cost less than the original biologic (often 15-35% lower), they can’t be as cheap as generics because you can’t just copy the formula-you have to recreate a living system. The cost savings come from competition, not simplicity.
Is it safe to switch between a biologic and its biosimilar multiple times?
Yes. Multiple clinical studies have shown that switching between a reference biologic and its biosimilar-even more than once-does not increase the risk of side effects or reduce effectiveness. The FDA requires this data before approving any interchangeable biosimilar. Real-world use in Europe and the U.S. over the past decade supports this. Patients who switch multiple times show no worse outcomes than those who stay on the original drug.
What should I do if my patient refuses to take a biosimilar?
Don’t push. Listen. Ask why they’re hesitant. Often, it’s fear of the unknown or misinformation. Use simple language: "This isn’t a cheap copy. It’s been tested just like the original. The FDA says it works the same way, with no meaningful difference in safety or results." Show them the FDA’s official facts. Offer to call the prescriber together. Sometimes, a quick conversation with the doctor is all it takes to ease concerns.
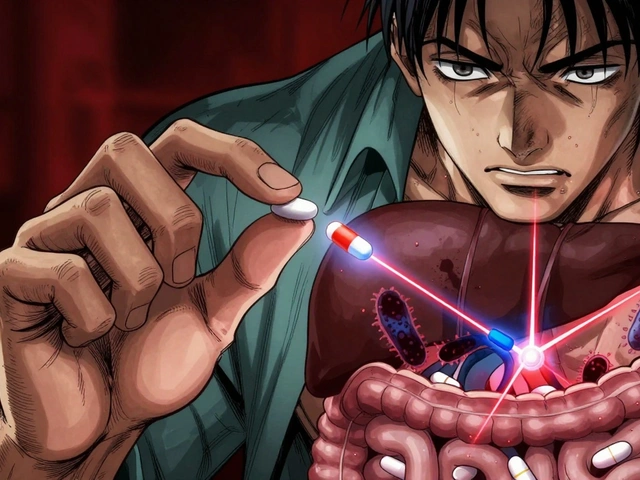
Why is batch number tracking so important with biosimilars?
Unlike generic drugs, biosimilars come from living cells, so tiny variations can happen between batches. If a patient has a reaction, we need to know exactly which batch they received to track safety issues. That’s why every biosimilar container must have the lot number printed on it. Pharmacists must record that number in the patient’s file. It’s not just paperwork-it’s a safety net for everyone.
If you’re a pharmacist, your role is more critical now than ever. You’re not just filling prescriptions-you’re building trust, cutting costs, and saving lives. The science is there. The data is there. All that’s left is for you to step in-and make the switch.




Kaushik Das
November 27, 2025 AT 07:24Man, I’ve seen this play out in Mumbai pharmacies - patients stare at the new blue pill like it’s a trap. I tell ‘em: ‘This ain’t some knockoff chai. It’s the same engine, just built in a different garage.’ One guy cried because he thought he was getting ‘fake medicine.’ We sat down, showed him the FDA sheet, and now he’s got a tattoo of the biosimilar logo on his forearm. No joke. Trust is built one conversation at a time.
And yeah, the color change? Huge. I had a woman stop her insulin biosimilar because it was ‘too yellow.’ We switched her to the same drug in a white vial - same dose, same everything - and she’s been stable for a year. Appearance isn’t cosmetic. It’s psychological.
Pharmacists are the unsung heroes here. Docs are swamped. Nurses are stretched thin. But we’re the ones holding the bottle, reading the label, and looking the patient in the eye. That’s power. And responsibility.
Also, batch tracking? Non-negotiable. I once traced a reaction back to a single lot. Saved three people. That’s why I write the lot number in the patient’s notebook, not just the EHR. If the system crashes, they still know what they took.
Stop calling them ‘cheap alternatives.’ They’re precision-engineered marvels. Just because they’re made from living cells doesn’t mean they’re less scientific. It means they’re more complex. And we’re the ones who get to explain that.
PS: If your PBM’s pushing the brand because it’s more profitable, you’re part of the problem. Not the solution.
Amanda Wong
November 28, 2025 AT 11:37Let’s be clear: the FDA’s definition of ‘no clinically meaningful difference’ is a legal loophole dressed up as science. The fact that you need 15 years of global data to prove safety means the original biologics were never properly vetted in the first place. Biosimilars aren’t safer - they’re just cheaper, and we’re being sold a lie that this is progress.
And don’t get me started on pharmacists substituting without consent. That’s not empowerment - it’s erosion of patient autonomy. If a doctor prescribes Humira, the patient has a right to Humira. Not some lab-grown copy that’s ‘close enough.’
87% of pharmacists recommend biosimilars? Of course they do. They’re incentivized. The system rewards volume, not vigilance. This isn’t healthcare innovation. It’s corporate cost-cutting with a PR facelift.
Stephen Adeyanju
November 28, 2025 AT 13:06So let me get this straight you’re telling me I can’t just swap out my biologic for a cheaper one because the pill is a different shape and the doc didn’t sign a piece of paper and the pharmacist has to write down a number that no one ever checks and now I have to sit through a 20 minute lecture about living cells and batch numbers and I just want my damn medicine
Also why is everyone acting like pharmacists are saints now they’re just doing their job stop making them heroes they’re not saving lives they’re just following rules that make the system less broken
Deborah Williams
November 29, 2025 AT 14:40It’s funny how we’ve turned healthcare into a bureaucratic obstacle course where the person who knows the most - the pharmacist - is the one who’s supposed to be the gatekeeper, not the guide.
We’ve created a system where the expert is forced to fight against inertia, misinformation, and profit-driven policy just to give a patient the same medicine they were supposed to get.
And yet, we still act surprised when people don’t trust the system.
Maybe the problem isn’t that patients are afraid of biosimilars.
Maybe the problem is that we’ve made them feel like guinea pigs in a cost-saving experiment dressed up as medical progress.
Empower pharmacists? Sure. But first, empower patients with transparency, not just pamphlets from the FDA.
And stop calling them ‘cheaper versions.’ That language isn’t neutral. It’s a psychological trigger. We’re not just dispensing drugs. We’re dispensing identity. And if you tell someone their medicine is ‘second-tier,’ they’ll believe it - no matter what the data says.
Asia Roveda
November 30, 2025 AT 07:25US pharmacists are getting too much credit here. This is just another way for big pharma to offload liability. The FDA lets them substitute because they don’t want to deal with the lawsuits if something goes wrong with the original. And now they’re pushing it on us like it’s patriotic.
Meanwhile, in India, they’re giving out biosimilars like candy - no counseling, no tracking, no paperwork. And guess what? People are dying from untraceable batches. We’re not leading the world. We’re just pretending to be responsible while the rest of the world is playing Russian roulette with their meds.
Sanjay Menon
November 30, 2025 AT 11:32One must acknowledge the epistemological rupture that biosimilars represent in pharmaceutical ontology. The biologic is not merely a molecule - it is a phenomenological artifact of cellular life, rendered into therapeutic form through an intricate dance of protein folding and post-translational modification. To equate its biosimilar counterpart with mere ‘chemical substitution’ is to commit a category error of the highest order.
Pharmacists, in their newfound role as biotherapeutics interpreters, are not merely dispensers - they are hermeneutic mediators between the clinical sublime and the layperson’s anxiety.
Yet, the American healthcare system, in its neoliberal absurdity, reduces this profound epistemic labor to a checkbox on an EHR form. How tragic. How profoundly un-philosophical.
One wonders: if a biosimilar is substituted in a forest, and no patient hears the batch number being logged - does it still have clinical meaning?
Ezequiel adrian
December 1, 2025 AT 11:32Bro this is wild 😎 I seen my cousin in Lagos switch from Remicade to biosimilar and he didn’t even know until he got the receipt. No talk, no forms, no ‘FDA 9 things’. Just swapped. He’s been fine for 3 years. Why we making it so complicated in the US? 🤔
Also the color thing? Yeah my dude thought the new pill was ‘fake’ because it was green instead of white. We laughed. Then he took it. Now he’s back at work. Simple.
Stop overthinking. Just tell people the truth. It works. Same thing. Different maker. End of story.
Ali Miller
December 2, 2025 AT 06:42Let’s not forget the real enemy here: the FDA. They approved these biosimilars too fast. Why? Because they’re under pressure from Congress to lower drug prices. So they lowered the bar. Now we’re playing Russian roulette with patients’ lives.
And don’t even get me started on the ‘interchangeable’ label. That’s a marketing term, not a scientific one. The FDA doesn’t test for long-term immune responses over 20 years. They test for 6 months. That’s not science. That’s politics.
And pharmacists? They’re just the foot soldiers. They don’t know any better. They’re trained to follow rules, not question them. This is how systems collapse. Slowly. Quietly. With good intentions.
And yes I’m still on Humira. And I’m not switching. Not until the FDA admits they made a mistake.
JAY OKE
December 4, 2025 AT 05:52I’ve been a pharmacist for 18 years. I’ve seen generics come and go. But biosimilars? They’re different. Not because they’re riskier. But because people *feel* different about them.
One patient told me, ‘I don’t care if it’s cheaper. I want what my doctor gave me.’ I didn’t argue. I just said, ‘Okay, I’ll call your doctor and ask if they’re open to a conversation.’
Turns out, the doctor was totally fine with it. The patient just needed to feel heard.
That’s the real secret. It’s not about the science. It’s about the story. And we’re the ones who get to rewrite it - one calm conversation at a time.
Joe bailey
December 4, 2025 AT 15:39Love this post. Seriously. As a UK pharmacist, we’ve been doing this for over a decade. No drama. No panic. Just clear communication and good record-keeping.
One thing I’ve learned: patients don’t care about ‘interchangeable’ labels. They care if you sound confident. If you say ‘this is safe’ and mean it, they believe you.
Also - batch numbers? Always write them in the patient’s own notebook. Not just the computer. If the system crashes, they still have proof. And if they travel? They can show it to a foreign pharmacist. Simple. Human.
Keep doing the work. The system will catch up.
james thomas
December 6, 2025 AT 14:39They’re lying to you. Biosimilars are just a Trojan horse. Big Pharma doesn’t want to lose money - so they made a cheaper version, then convinced doctors and pharmacists it’s the same. But the real drug companies still own the patents on the *processes* used to make the biosimilars. So they’re still getting paid. And you? You’re the one taking the risk.
Ever heard of the ‘patent thicket’? That’s what this is. A legal maze to keep you hooked on the same companies.
And now they’re pushing pharmacists to be the face of this scam. ‘Trust us, we know what we’re doing.’
No. I don’t trust you. And I’m not switching.
Also - the FDA? They’re owned by pharma. Just look at the revolving door. Same people. Same companies. Same lies.