Diarrhea Severity Assessment Tool
When you start a new medication, you expect relief-not a new problem. But for many people, especially those on chemotherapy, antibiotics, or immunotherapy, one of the most common and disruptive side effects is medication-induced diarrhea. It’s not just an inconvenience. Left untreated, it can lead to dehydration, hospital stays, or even force you to stop life-saving treatments. The good news? With the right steps, you can often stop it before it gets serious.
What Causes Medication-Induced Diarrhea?
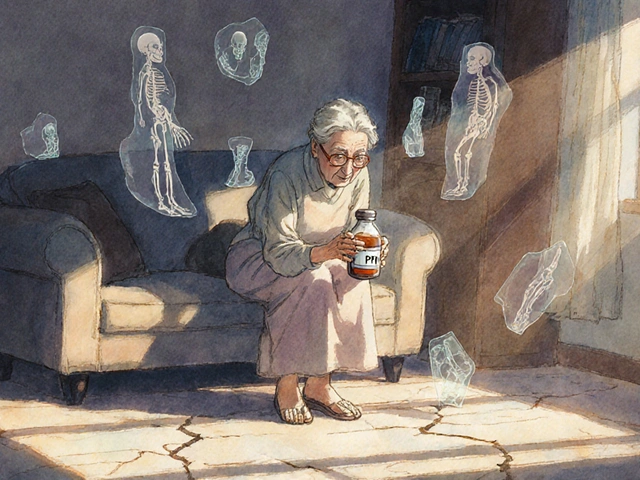
Medication-induced diarrhea (MID) happens when a drug disrupts the normal balance of your digestive system. It’s not one-size-fits-all. Different drugs cause different types of diarrhea, and knowing which one you’re dealing with changes how you treat it.Chemotherapy drugs like irinotecan and 5-fluorouracil are the biggest culprits. Up to 80% of patients on these drugs get diarrhea, and about 1 in 4 develop severe cases. Antibiotics are another major trigger-especially broad-spectrum ones like clindamycin or ciprofloxacin. They kill off good gut bacteria, letting harmful ones like Clostridioides difficile take over. Immunotherapy drugs, newer cancer treatments that boost your immune system, can also trigger inflammation in the colon, leading to watery stools and cramping.
It’s not just cancer drugs. Even common prescriptions like metformin (for diabetes), NSAIDs (like ibuprofen), and certain heart medications can cause loose stools. The key is timing. If diarrhea starts within days of beginning a new medication, it’s likely linked.
How Bad Is It? Grading the Severity
Not all diarrhea is the same. Doctors use a simple grading system to decide how urgent treatment needs to be:- Grade 1: 1-3 more bowel movements than usual per day. Mild, manageable.
- Grade 2: 4-6 movements per day. Noticeable discomfort, may interfere with daily life.
- Grade 3: 7 or more movements per day, incontinence, or hospitalization needed. Requires immediate medical attention.
- Grade 4: Life-threatening-severe dehydration, shock, or organ failure. Needs emergency care.
Most people start at grade 1 or 2. But if you wait too long to act, it can jump to grade 3 or 4 in less than 24 hours. That’s why early intervention is everything.
First-Line Treatment: Loperamide (Imodium)
For mild to moderate diarrhea from chemotherapy or non-infectious causes, loperamide is the go-to. It slows down your gut, letting your body absorb more fluid and reduce stool frequency.The standard dose? Take 4 mg right away when you notice your first loose stool. Then take 2 mg after every unformed stool, up to a maximum of 16 mg per day. For irinotecan-induced diarrhea, the limit can go up to 24 mg per day under medical supervision.
Studies show loperamide works in 60-75% of grade 2 cases. But here’s the catch: it only works if you start early. A 2021 analysis found that patients who waited more than 24 hours to take loperamide were over three times more likely to develop severe diarrhea.
Don’t go over the daily limit. Too much loperamide can cause dangerous heart rhythm problems or even intestinal blockage. If you’re still having diarrhea after 48 hours, stop and call your doctor. Prolonged use without supervision increases the risk of ileus-a dangerous slowdown of bowel movement.
When Loperamide Isn’t Enough: Octreotide
If you’re on grade 3 or 4 diarrhea, or if loperamide doesn’t help after 24 hours, the next step is octreotide. This is a shot you give under the skin. It’s not a first-choice drug-it’s for serious cases.Octreotide works differently than loperamide. Instead of slowing your gut, it reduces the amount of fluid your intestines pump out. It’s especially effective for chemotherapy-induced diarrhea. Studies show it works in 60-95% of severe cases.
The usual dose is 100-150 micrograms injected under the skin three times a day. Some patients get a continuous infusion through a pump if the shots aren’t enough. It’s not pleasant-many report pain or bruising at the injection site-but it can prevent hospitalization.
Doctors recommend starting octreotide within 4 hours of severe diarrhea to cut hospitalization risk by 35%. If you’re on chemotherapy, ask your nurse to show you how to give the shot at home. Pre-mixing doses ahead of time helps avoid mistakes during a crisis.

What to Avoid: When Diarrhea Is an Infection
Here’s a critical warning: never use loperamide or octreotide if you suspect an infection. If you have a fever over 38.5°C, bloody stools, or diarrhea that started after taking antibiotics, you might have Clostridioides difficile (C. diff). This is a serious gut infection.Antimotility drugs like loperamide can trap toxins in your colon, leading to toxic megacolon-a life-threatening condition. The CDC and IDSA guidelines say: test for C. diff before using any anti-diarrheal if you’re on antibiotics.
If it’s C. diff, you need antibiotics like vancomycin (125 mg four times a day for 10 days), not loperamide. Vancomycin cures 97% of cases. Metronidazole used to be the go-to, but it’s less effective now and only used if vancomycin isn’t available.
Diet and Hydration: Your Secret Weapons
Medication-induced diarrhea drains your body of fluids and electrolytes. Dehydration can hit fast, especially in older adults or those with other health conditions.Drink oral rehydration solutions (ORS). These aren’t just sports drinks-they’re specially balanced with 75 mmol/L sodium, 75 mmol/L glucose, and 20 mmol/L potassium. Mix one packet with 200 mL of clean water. Sip slowly, even if you don’t feel thirsty.
Watch what you eat. Avoid dairy, fatty foods, spicy meals, and high-fiber items like beans or raw vegetables. Stick to bland, low-residue foods: white rice, bananas, applesauce, toast, boiled chicken. The European Society for Medical Oncology recommends this diet for at least 48 hours after diarrhea starts.
Some people find relief with bismuth subsalicylate (Pepto-Bismol), especially if there’s inflammation. But don’t use it if you’re allergic to aspirin or have kidney problems. Stick to 524 mg every 30-60 minutes, no more than 8 doses in 24 hours.
Probiotics: Helpful or Hype?
You’ve probably heard that probiotics can prevent antibiotic diarrhea. The truth? It’s mixed.The American Gastroenterological Association says probiotics can cut the risk of antibiotic-associated diarrhea by half. But not all probiotics work. Only two strains have strong evidence: Lactobacillus rhamnosus GG and Saccharomyces boulardii. If you’re on antibiotics, ask your doctor if one of these is right for you. You need to take it daily, starting the same day as your antibiotic.
Other probiotics? The evidence is weak. Don’t waste money on generic brands claiming to “restore gut health.” Stick to the proven ones.
What to Do When It Starts: A Simple Action Plan
If you’re on a medication that can cause diarrhea, have a plan ready:- At first loose stool: Take 4 mg of loperamide immediately.
- Keep tracking: Write down how many stools you have each day. Use a notebook or phone app.
- Hydrate: Drink ORS every 2-3 hours. Don’t wait until you’re thirsty.
- Watch for red flags: Fever, blood in stool, dizziness, or no improvement after 24 hours? Call your oncologist or doctor right away.
- If it gets worse: If diarrhea hits grade 3 (7+ stools/day), start octreotide as directed-don’t wait.
Many patients who manage this well keep a small kit ready: loperamide pills, ORS packets, alcohol wipes, and pre-filled octreotide syringes. It saves time and stress during a flare-up.
When to Get Help Immediately
Don’t try to tough it out. Call your healthcare team if you have:- Diarrhea lasting more than 48 hours
- More than 6 stools in a day
- Fever above 38.5°C
- Bloody or black stools
- Signs of dehydration: dry mouth, dark urine, dizziness, rapid heartbeat
- Abdominal swelling or severe pain
These aren’t just “bad days.” They’re warning signs that your body is under stress-and treatment may need to be paused or changed.
The Bigger Picture: Why This Matters
Medication-induced diarrhea isn’t just a personal nuisance. It’s a major healthcare issue. In the U.S., it costs over $2 billion a year-mostly from hospital stays and delayed cancer treatments. Patients who get it under control are more likely to finish their full course of chemo or antibiotics, which improves survival rates.There’s also new hope on the horizon. In 2023, the FDA approved onercept, a new drug that reduces severe chemotherapy diarrhea by 63%. In 2024, ASCO updated guidelines to recommend neomycin as a preventive measure for high-risk patients on irinotecan, cutting diarrhea rates from 65% to 32%. And microbiome therapies like SER-109, approved for recurrent C. diff, are showing promise for preventing future episodes.
Personalized medicine is coming too. Doctors are starting to test for the UGT1A1 gene variant, which predicts who’s more likely to have severe reactions to irinotecan. This could mean pre-treatment adjustments to avoid diarrhea before it starts.
Final Thoughts: You’re Not Alone
Managing medication-induced diarrhea is hard. It’s tiring, embarrassing, and disruptive. But it’s also very treatable-if you know what to do and when to do it.Start early. Stay hydrated. Know your limits. Don’t be afraid to ask for help. Whether you’re on chemotherapy, antibiotics, or something else, your medical team wants you to stay on track. And with the right tools, you can keep your treatment going without letting diarrhea take control.
Can loperamide cause constipation?
Yes, loperamide can cause constipation, especially if you take it for more than 48 hours or exceed the recommended dose. About 25% of users report this side effect. If you haven’t had a bowel movement in 2-3 days after starting loperamide, stop taking it and contact your doctor. Constipation can lead to bowel blockage if ignored.
Is it safe to take loperamide with antibiotics?
Only if your doctor confirms it’s not caused by C. difficile. Antibiotic-associated diarrhea can be a sign of a serious infection. Taking loperamide in that case can trap toxins in your colon and lead to toxic megacolon. Always get a stool test before using anti-diarrheals if you’re on antibiotics.
Can I use Pepto-Bismol for medication-induced diarrhea?
Bismuth subsalicylate (Pepto-Bismol) can help with mild, inflammatory diarrhea, but it’s not first-line. Avoid it if you’re allergic to aspirin, have kidney disease, or are on blood thinners. Use no more than 8 doses in 24 hours, and stop if symptoms don’t improve within 48 hours.
How do I prepare oral rehydration solution at home?
Use pre-packaged ORS powders (available at pharmacies) and mix one packet with exactly 200 mL of clean, boiled, and cooled water. Do not use tap water unless it’s been filtered or boiled. Drink small sips every 15-20 minutes. Avoid homemade mixes with sugar and salt-they don’t have the right balance and can make dehydration worse.
Should I stop my medication if I get diarrhea?
Never stop a prescribed medication without talking to your doctor. Many cases of diarrhea can be managed without stopping treatment. Stopping chemo or antibiotics early can reduce effectiveness and lead to worse outcomes. Work with your team to control symptoms while staying on schedule.
Are there any new treatments for medication-induced diarrhea?
Yes. In 2023, the FDA approved onercept, a drug that reduces severe chemotherapy diarrhea by 63%. In 2024, ASCO guidelines added neomycin prophylaxis for high-risk patients on irinotecan, cutting diarrhea rates in half. Microbiome therapies like SER-109 are also now approved for preventing recurrent C. diff infections, offering long-term protection.




Diane Tomaszewski
November 15, 2025 AT 12:13It’s not about the medicine. It’s about your body trying to reset itself. Diarrhea isn’t a bug-it’s a feature. Your gut is cleaning house. You just gotta let it work. Most people panic and suppress it. That’s the real mistake.
Latrisha M.
November 16, 2025 AT 14:39Start with loperamide only if you’re sure it’s not C. diff. Always test first. Hydration is non-negotiable. ORS beats Gatorade every time. Keep a log. Simple. Effective.
David Rooksby
November 18, 2025 AT 01:13Let me tell you something they don’t want you to know-pharma companies *want* you to have diarrhea because then you need more drugs. Loperamide? Made by a subsidiary of a company that also makes antibiotics. Octreotide? Pricey as hell. Meanwhile, probiotics like Saccharomyces boulardii have been used in Europe since the 70s-banned in the US for decades until they patented it. Coincidence? I think not. They profit from chaos. You’re not sick-you’re being exploited.
Teresa Smith
November 18, 2025 AT 01:48For anyone starting chemo or antibiotics-have your loperamide and ORS packets ready before day one. Don’t wait for disaster. Proactive care saves lives. And yes, you can still do your treatment. You just need a plan. Talk to your nurse. Ask for a diarrhea management kit. They’ll give you one if you ask.
John Mwalwala
November 19, 2025 AT 02:10Did you know that the UGT1A1 gene variant increases irinotecan toxicity by 400%? That’s not just genetics-that’s pharmacogenomics. Most docs don’t test for it. But if you’re of African or Ashkenazi descent, you’re statistically more likely to carry it. They’re giving you the same dose as everyone else. That’s not medicine. That’s roulette. Demand the test. It’s covered by Medicare.
Oyejobi Olufemi
November 20, 2025 AT 22:17They say 'start early'-but who's monitoring you? Who's checking your electrolytes? Who's telling you when to stop loperamide? Nobody. The system is designed to push you through. They'll say 'take 16mg' then when you get constipated they'll say 'oh that's normal'-but you're not normal, you're in ileus. They don't care. You're a number. Your colon? Just a side effect.
Deepak Mishra
November 22, 2025 AT 11:25OMG I JUST GOT ON IRINOTECAN AND I’M HAVING 10 STOOLS A DAY 😭😭😭 I TOOK 2 IMODIUM AND NOW I’M STUCK IN THE BATHROOM AND CAN’T MOVE 😭😭😭 HELP!!
Latrisha M.
November 23, 2025 AT 04:26Call your oncology team immediately. Do not wait. If you’re at 10 stools/day, you’re grade 3. Start octreotide if you have it. If not, go to the ER. Hydration is critical. Don’t eat anything solid. Just ORS. You’re not alone. This happens. But you need help now, not later.
Dan Angles
November 23, 2025 AT 14:25While the management protocols outlined are clinically sound, it is imperative to emphasize that patient autonomy and informed consent must remain central. The decision to initiate pharmacologic intervention-particularly with agents such as octreotide-must be preceded by a comprehensive risk-benefit analysis, including consideration of comorbidities, renal function, and cardiac history. The FDA’s approval of onercept represents a significant advancement; however, access disparities remain a systemic concern.
Rachel Wusowicz
November 23, 2025 AT 21:53They say 'test for C. diff'... but have you seen the wait times? 72 hours? I had to beg for a stool test. They said 'it's probably just meds'... then I ended up in ICU with toxic megacolon. They don't test because they don't want to admit they gave you the wrong drug. They'd rather you die quietly than admit their protocol is broken. And now they're selling 'SER-109' for $30K a dose. That's not medicine. That's extortion.
Jamie Watts
November 25, 2025 AT 02:50Probiotics are a scam unless you’re taking LGG or S. boulardii. I’ve seen people waste hundreds on ‘gut health’ blends that are just sugar and dead bacteria. Stick to the science. And no, kefir won’t fix your chemo diarrhea. I know, I tried it.
ZAK SCHADER
November 25, 2025 AT 03:38why do y’all care so much about diarrhea? in america we got free hospitals. just go to er. theyll give you fluids and a new drug. problem solved. stop overthinking. its just poop.
Danish dan iwan Adventure
November 26, 2025 AT 20:16Baseline: Diarrhea = gut dysbiosis. Loperamide = symptomatic suppression. Octreotide = neuroendocrine modulation. ORS = fluid-electrolyte homeostasis. Probiotics = strain-specific microbial reconstitution. C. diff = toxin-mediated colitis. Standard of care: Rule out infection before antimotility. Failure to comply = increased morbidity. QED.
Melanie Taylor
November 27, 2025 AT 07:43OMG this is SO important!! I just started chemo last week and I was terrified 😭 thank you for writing this!! I already printed it out and taped it to my fridge!! 💕💕💕 and I got my ORS packets ready!! 🥰
Daniel Stewart
November 29, 2025 AT 07:10It’s curious how we treat the body as a machine to be fixed, rather than a system to be understood. Diarrhea is not an enemy-it is a signal. We have forgotten how to listen. We reach for drugs before we ask why. The real question is not how to stop it-but what is the body trying to tell us? And why, in our haste, do we silence it?