Cyclosporine Safety Checker
Check Your Safety Parameters
Enter your current cyclosporine levels and kidney function values to see if they're within safe ranges for your transplant stage.
When you take cyclosporine after a kidney, heart, or liver transplant, it’s not just about keeping your immune system in check-it’s about staying alive without wrecking your kidneys. This drug saves lives, but it’s also one of the most dangerous medications you can take if not monitored closely. About cyclosporine nephrotoxicity affects 25% to 75% of transplant patients, and in some cases, it’s the main reason a new organ fails years down the line. The good news? You can prevent most of it-if you know what to watch for and how to measure it right.
Why Cyclosporine Is So Risky
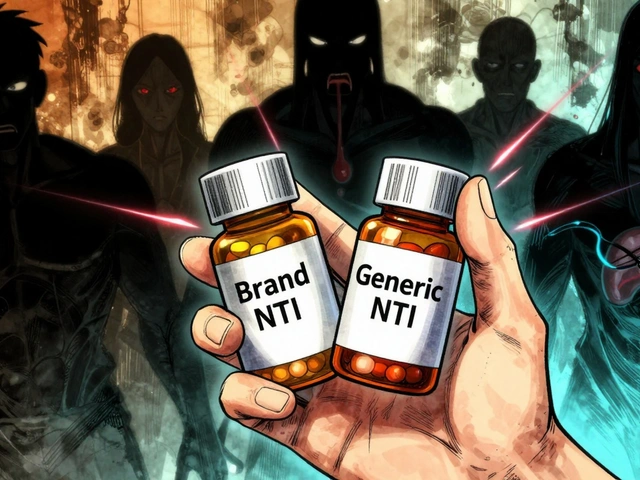
Cyclosporine works by blocking a key immune signal called calcineurin. That stops your body from attacking the new organ. But it also tightens blood vessels in your kidneys, reducing blood flow. Over time, this causes scarring, tubule damage, and stiff arteries inside the kidney. These changes don’t show up on scans. They creep in slowly, often without symptoms until your creatinine levels spike or your blood pressure won’t budge. The problem isn’t just the drug. It’s how little room there is between the dose that works and the dose that harms you. This is called a narrow therapeutic index. A level of 180 ng/mL might keep your transplant safe. But 220 ng/mL could start damaging your kidneys. And that’s just for starters. Your body absorbs and breaks down cyclosporine differently than anyone else’s. Two people on the same dose can have completely different blood levels. That’s why guessing isn’t an option.What Blood Levels You Need to Hit
Monitoring isn’t about checking once and forgetting. It’s a moving target. The right level changes over time. Here’s what current guidelines say:- First week after transplant: 200-400 ng/mL
- Week 2 to 6 months: 125-275 ng/mL
- 7 to 12 months: 100-150 ng/mL
- After 1 year: 75-160 ng/mL
How Blood Levels Are Measured-And Why It Matters
Not all blood tests are created equal. For years, most labs used immunoassays because they were cheap and fast. But these tests can’t tell the difference between cyclosporine and its many metabolites. That means they often report levels that are 10-15% too high. If your lab uses this method, your doctor might lower your dose unnecessarily-putting you at risk for rejection. The gold standard is liquid chromatography-tandem mass spectrometry (LC-MS/MS). It’s accurate to 99.2%, picks up levels as low as 5 ng/mL, and ignores metabolites completely. Since 2021, 92% of U.S. transplant centers have switched to LC-MS/MS. If your lab still uses older methods, ask if they can upgrade. It’s not just better-it’s safer.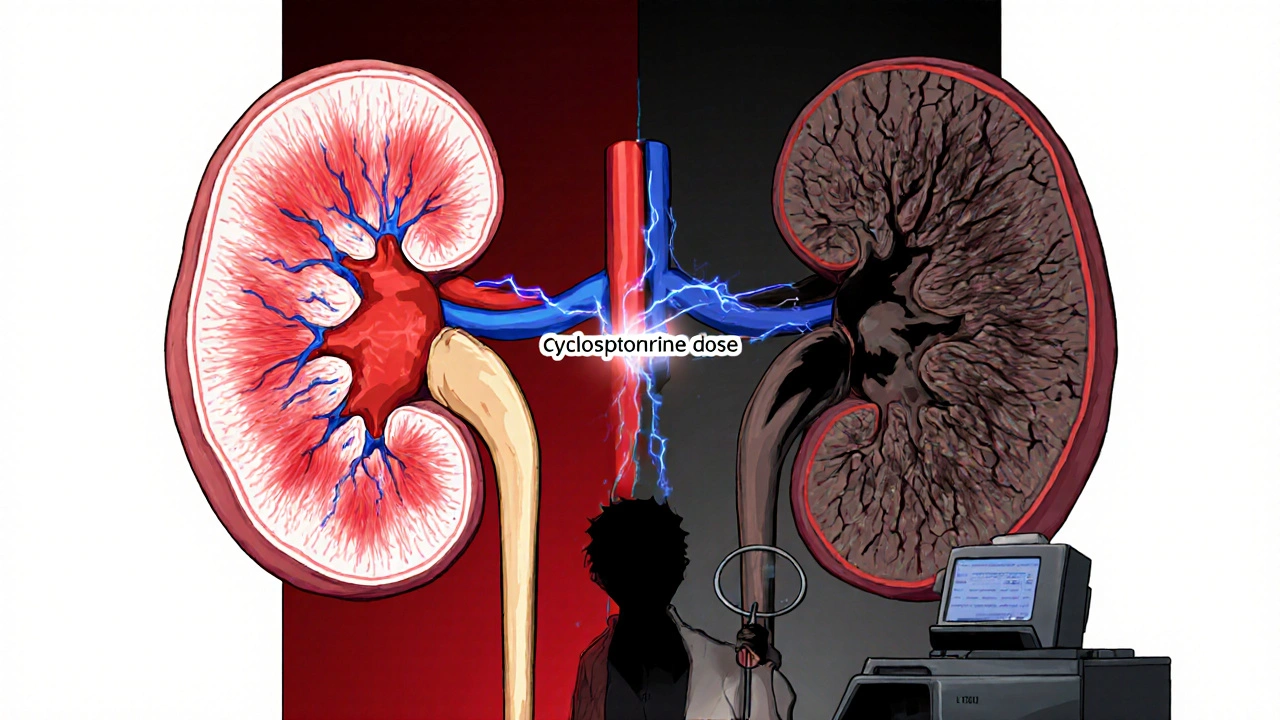
When to Test: Trough vs. C2 Monitoring
Most people think you just check cyclosporine right before your next dose-the “trough” or C0 level. But that’s outdated. Studies show the level two hours after you take your pill (C2) correlates much better with how much drug your body actually absorbed over the whole day. The correlation is 0.87 for C2 versus just 0.63 for C0. That’s a big difference. Centers using C2 monitoring saw a 22.4% drop in kidney damage without increasing rejection rates. That’s huge. Here’s how it works:- Take your dose at 8 a.m.
- Get blood drawn at 10 a.m.-exactly two hours later.
- Don’t eat, drink, or take other meds during that window.
What Else to Monitor-Beyond the Drug Level
Cyclosporine doesn’t just mess with your blood levels. It throws your whole body off balance. You need to track more than just the drug:- Serum creatinine: Keep it under 1.5 mg/dL. A rise of 0.3 mg/dL in a week is a red flag.
- BUN-to-creatinine ratio: Should be below 20:1. Higher numbers suggest reduced kidney blood flow.
- Blood pressure: Target is under 130/80 mmHg. Cyclosporine causes high blood pressure in nearly half of users.
- Magnesium: Low levels (below 1.7 mg/dL) are common and can cause muscle cramps or irregular heartbeat.
- Drug interactions: Ketoconazole, grapefruit juice, and some antibiotics can spike cyclosporine levels by 30-50%. Rifampin and St. John’s wort can slash them by 40-60%. Always tell every doctor you see that you’re on cyclosporine.
How Often Should You Get Tested?
Frequency depends on how long you’ve been on the drug:- First month: Twice a week
- Months 2-6: Once a week
- Months 7-12: Every two weeks
- After year one: Monthly or as needed

What If Your Kidneys Are Already Damaged?
The good news: early kidney damage from cyclosporine is often reversible. If caught in time, lowering the dose or switching to another immunosuppressant can let your kidneys recover within 3 months. That’s why regular monitoring isn’t optional-it’s your best defense. If your creatinine has been climbing for months and your doctor hasn’t acted, ask for a kidney biopsy. It’s the only way to confirm if the damage is from cyclosporine or something else, like rejection or infection.What’s Coming Next
The future of cyclosporine monitoring is moving fast. Point-of-care devices that give results in under 15 minutes are in Phase 3 trials and could be approved by late 2025. These will let you test at home-no more long waits for lab results. AI tools are also being tested to predict your ideal dose using 17 different factors: your weight, age, genetics, diet, other meds, even your sleep patterns. One trial showed 89.7% accuracy in predicting the right dose without frequent blood draws. That could mean fewer needles and better outcomes.What You Can Do Today
You don’t need to wait for the future to protect your kidneys. Here’s what to do now:- Ask your transplant team: "Do you use LC-MS/MS for cyclosporine testing?" If not, ask why.
- Request C2 monitoring if you’re in the first six months post-transplant.
- Keep a log: Write down your dose, time taken, and any symptoms (headache, swelling, fatigue).
- Never take new meds or supplements without checking with your transplant pharmacist.
- Get your blood pressure checked at every visit. Don’t assume it’s fine if you feel okay.




Jim Oliver
November 4, 2025 AT 22:49William Priest
November 6, 2025 AT 16:54Ryan Masuga
November 8, 2025 AT 15:54Jennifer Bedrosian
November 10, 2025 AT 13:25Lashonda Rene
November 10, 2025 AT 22:24Andy Slack
November 11, 2025 AT 00:06Rashmi Mohapatra
November 11, 2025 AT 17:24Abigail Chrisma
November 12, 2025 AT 01:31Ankit Yadav
November 12, 2025 AT 19:07Meghan Rose
November 12, 2025 AT 23:44Steve Phillips
November 13, 2025 AT 20:27Rachel Puno
November 13, 2025 AT 20:44