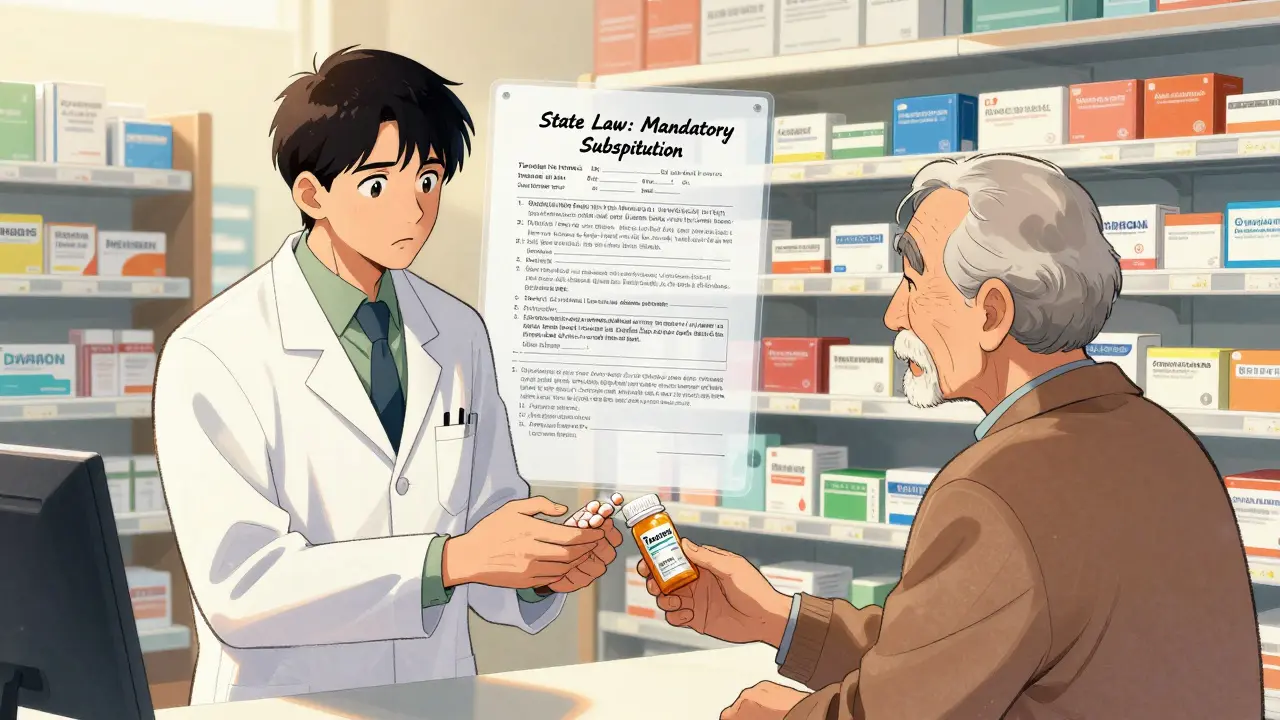
When you pick up a prescription, you might assume the pharmacist will give you the cheapest version of your medicine-unless your doctor says otherwise. But that’s not true everywhere. In some states, pharmacists must switch you to a generic drug. In others, they can only do it if they think it’s okay-and even then, they might need your permission. This isn’t about pharmacy policy. It’s about state law. And the differences between states can change how much you pay, whether you stick with your meds, and even how safe your treatment is.
What’s the Real Difference Between Mandatory and Permissive Substitution?
Mandatory substitution means the law forces pharmacists to give you the generic version of a drug, as long as it’s approved by the FDA and the doctor didn’t block it. Permissive substitution means pharmacists are allowed to switch you to a generic-but they don’t have to. They can choose to give you the brand name instead, even if the generic is cheaper and just as effective. This isn’t a small detail. It’s a legal rule that shapes how millions of prescriptions are filled every year. In 19 states, including Alabama, Colorado, Maine, and West Virginia, pharmacists are legally required to substitute generics unless the prescriber writes “Dispense as Written” or “Brand Medically Necessary” on the prescription. In the other 31 states, substitution is optional. The pharmacist can decide based on their judgment, the patient’s history, or even how busy the pharmacy is that day. The difference isn’t just legal-it’s financial. A 2011 study tracked simvastatin prescriptions right after the brand-name patent expired. In mandatory states, 48.7% of prescriptions were filled with generics. In permissive states? Only 30%. That’s nearly a 20 percentage point gap. And since generics cost 80-85% less than brand names, that gap translates to real money-hundreds of millions saved in Medicaid and Medicare programs every year.Why Do Some States Require Patient Consent?
It’s not enough to just allow substitution. Some states add another layer: you have to say yes. Seven states plus Washington, D.C., require pharmacists to get your explicit consent before switching you to a generic. That means the pharmacist has to ask you, “Do you want the cheaper version?” and you have to say “yes.” That sounds fair, right? But here’s the catch: when consent is required, generic use drops to just 32.1%. Without consent? It jumps to 98.1%. Why? Because most people don’t know the difference between brand and generic. They don’t ask. They assume the pharmacist knows best. And if they’re not asked, they won’t say no. But if they’re asked, even once, many say “no” out of habit, fear, or confusion-even when there’s no medical reason to avoid the generic. This is especially true for older adults and people with chronic conditions. A patient on a blood thinner or epilepsy medication might worry that switching brands could cause problems-even though the FDA says generics are just as safe. Pharmacists in these states end up playing it safe: they don’t substitute unless they’re forced to. The result? More expensive prescriptions, more missed doses, and more people falling out of treatment.What About Liability? Are Pharmacists Protected?
If you get sick after a generic drug is switched, who’s responsible? That’s where liability rules come in. In 24 states, pharmacists have no legal protection if something goes wrong after a substitution. That means if a patient has an adverse reaction, the pharmacist could be sued-even if they followed all the rules. That creates a huge disincentive. Pharmacists in those states are more likely to avoid substitution altogether. Especially with drugs that have a narrow therapeutic index-medications where even a tiny change in dosage can cause harm, like warfarin, lithium, or levothyroxine. In mandatory states without consent rules, pharmacists substitute these drugs more often. But in mandatory states with consent rules? Pharmacists are nearly twice as likely to skip substitution, even when it’s safe. The safest approach? States that combine mandatory substitution with clear liability protections. That way, pharmacists know they won’t be punished for doing the right thing. And patients get the cost savings without the fear.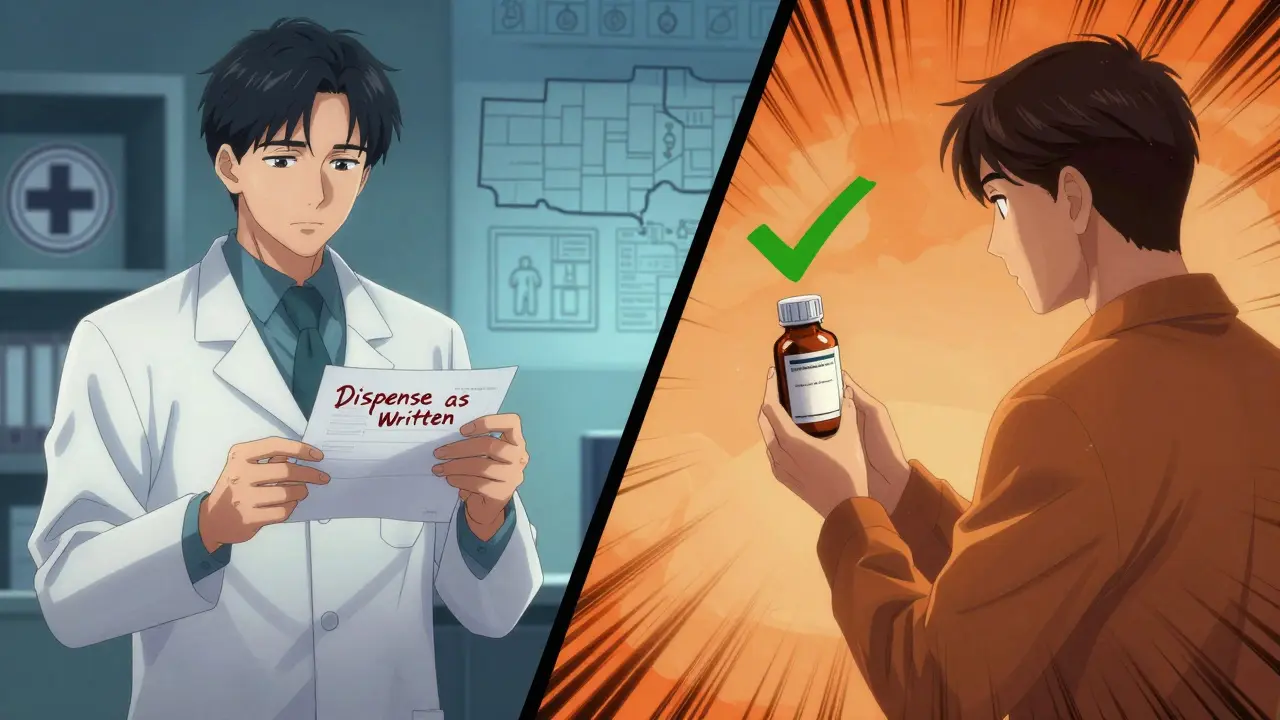
How Do States Decide What Can Be Substituted?
Not all drugs are treated the same. The FDA’s Orange Book is the official list of drugs that are considered therapeutically equivalent. Most states use this as their guide: if the generic is listed there, substitution is allowed. But some states go further. A few use “positive formularies”-lists of drugs that pharmacists are allowed to substitute. Others use “negative formularies,” which list drugs that can’t be switched. For example, some states block substitution for drugs like insulin, seizure meds, or certain cancer treatments-even if the FDA says they’re interchangeable. And then there’s the big wildcard: biosimilars. These are generic versions of complex biologic drugs like Humira or Enbrel. They’re expensive, hard to make, and tricky to switch. Forty-five states have stricter rules for biosimilars than for regular generics. Most require the doctor to give explicit permission before switching. Some even require the pharmacist to notify the doctor after the switch. Only nine states treat biosimilars the same as regular generics. That’s a problem. Biosimilars can cut costs by up to 70%. But if doctors and pharmacists are scared to switch because of confusing rules, patients pay more-and insurers pay more. The result? Slower adoption of cheaper, equally effective treatments.What Does the Prescription Say? The Hidden Rules
Even if your state allows substitution, the way your doctor writes the prescription matters. In some states, prescriptions have two lines: one for the drug name, and another where the doctor checks a box that says “Substitution Permitted.” If that box isn’t checked, the pharmacist can’t switch. In other states, the doctor has to write “Dispense as Written” or “Do Not Substitute” by hand. If they don’t, substitution is allowed. That sounds simple-but doctors don’t always know the rules. A study found that in states without clear prescription formats, up to 40% of doctors didn’t know how to block substitution correctly. This creates chaos. A patient gets a prescription in California, then fills it in Texas. The rules change. The pharmacist doesn’t know what the doctor meant. The patient gets confused. And the drug they need might not be covered-or might cost 10 times more.
Why This Matters for You
If you take a generic drug, you probably don’t think about the law behind it. But if you’ve ever been told, “We can’t give you the cheaper version,” or “We need your permission to switch,” that’s because of state law. And if you’ve ever skipped a refill because the price was too high? That might be because your state doesn’t require substitution. The data is clear: mandatory substitution without patient consent leads to higher generic use, lower costs, and better adherence. States that make it easy for pharmacists to substitute save money. Patients take their meds longer. Health outcomes improve. But when states add layers-consent forms, liability risks, physician notifications-they slow things down. And in a system where every day without medication can lead to hospitalization, that delay costs lives.What’s Changing? The Trend Toward Mandatory Substitution
The number of states with mandatory substitution has grown. In 2014, only 14 states required it. By 2020, that number jumped to 19. That’s not an accident. It’s a response to rising drug prices and pressure from Medicaid programs and public health advocates. Experts like Dr. Aaron Kesselheim from Harvard say the best way to cut costs and improve care is to make substitution the default. “Optimizing state laws to facilitate generic drug substitution as the default option is an important lever,” he says. The next frontier? Biosimilars. As more biologic drugs lose patent protection, states will need to update their rules. But if they keep treating biosimilars like risky experiments instead of proven alternatives, the savings won’t happen. The fix? Simpler rules. Clearer prescriptions. Better education. And a system that trusts pharmacists to make the right call-unless a doctor has a real medical reason to stop them.Can a pharmacist substitute my brand-name drug without telling me?
In 31 states and Washington, D.C., pharmacists are required to notify you that a substitution was made-even if it’s not on the prescription label. In 19 states, substitution is mandatory and notification is not required. In the remaining states, pharmacists may substitute without telling you unless your state has a consent rule. Always check your receipt or ask if you’re unsure.
Why does my doctor say “Dispense as Written” on my prescription?
That phrase means your doctor wants you to get the brand-name drug, not the generic. It’s usually because they believe the brand is safer or more effective for your condition-especially for drugs with a narrow therapeutic index like blood thinners or seizure meds. In mandatory substitution states, this note blocks the pharmacist from switching. In permissive states, it’s a recommendation, not a rule.
Are generic drugs really as good as brand names?
Yes. The FDA requires generics to have the same active ingredient, strength, dosage form, and route of administration as the brand name. They must also be bioequivalent-meaning they work the same way in your body. The only differences are in inactive ingredients like fillers or dyes, which rarely affect how the drug works. Most patients experience no difference at all.
Can I refuse a generic substitution even if my state allows it?
Yes. Even in mandatory substitution states, you can ask for the brand name. The pharmacist may charge you the full price if the generic is cheaper, but they must honor your request. In permissive states, you can always ask for the brand. Just make sure you understand the cost difference before you say yes.
Do these laws apply to biosimilars the same way as regular generics?
No. Most states treat biosimilars differently. Forty-five states require additional steps like physician notification or written consent before switching to a biosimilar. Only nine states allow automatic substitution like they do with regular generics. That’s because biosimilars are more complex, and regulators are being cautious. But experts warn that overly strict rules are slowing access to cheaper, life-saving treatments.