Have you ever opened a bottle of eye drops or a cream and noticed it changed color? Maybe it turned yellow, cloudy, or smells off? That’s not normal. It’s not old age - it’s light damage. Light-sensitive medications, including many eye drops, antibiotics, and hormone treatments, can lose half their strength in just a few weeks if left on a bathroom counter or near a window. And if they degrade, they don’t just stop working - they can become unsafe.
Why Light Matters More Than You Think
Not all medications are created equal when it comes to light. Some are fine in a bright cabinet. Others? They’re like film - expose them to sunlight or even bright indoor lighting, and they break down. This isn’t theory. It’s science. The U.S. Pharmacopeia (USP) lists 470 injectable drugs that must be protected from light. For eye drops alone, studies show that clear containers can cause up to 35% loss in potency within two weeks. That means your glaucoma drops, which you rely on daily, might be working at only 65% capacity. And you wouldn’t even know.Dr. Emily Chew from the National Eye Institute says it plainly: “Ophthalmic solutions are especially vulnerable because they’re water-based. Light hits them like a spotlight.” The same goes for tetracycline antibiotics, birth control pills, chemotherapy agents, and even vitamin D drops. When these drugs break down, they don’t just weaken - they can form toxic byproducts. One Reddit user reported throwing out $120 worth of tretinoin cream after it turned yellow from being stored in a steamy bathroom. That’s not just money lost - it’s health risk.
What Counts as Light-Sensitive?
Look at your medicine cabinet. Now, look at the labels. If you see “Protect from Light,” “Store in Original Container,” or a small sun-with-a-slash symbol, that’s your cue. About 78% of light-sensitive medications have this warning, according to USP data. But here’s the catch: many people don’t notice it. They assume all bottles are the same.Common light-sensitive items include:
- Eye drops (latanoprost, bimatoprost, timolol)
- Antibiotics (tetracycline, doxycycline, nitrofurantoin)
- Chemotherapy drugs (bleomycin, cisplatin)
- Hormonal treatments (birth control pills, testosterone gels)
- Anti-seizure medications (phenytoin)
- Vitamin D and other liquid supplements
- Insulin (though temperature is the bigger issue, light still matters)
Even if your bottle looks dark, don’t assume it’s safe. Some clear bottles have UV-blocking coatings. Others are just tinted plastic that lets through enough light to ruin the drug. The only way to be sure? Stick with the original packaging - unless you’re replacing it with a proper amber container.
Amber Bottles: The Gold Standard
The best storage for light-sensitive meds is an amber (brown) glass bottle. These aren’t just colored - they’re engineered to block UV and blue light below 470 nanometers. USP standards say they must let through less than 10% of that light. Amber glass blocks 98% of harmful rays. High-end opaque plastic blocks about 85%. That 13% gap matters when you’re talking about life-saving drugs.Here’s the thing: amber bottles aren’t perfect. You can’t see how much is left. That’s why some people transfer eye drops to clear droppers. Don’t. That’s one of the top mistakes. The American Academy of Ophthalmology says 18% of eye drop failures happen because patients poured them into non-protective containers. If your original bottle is broken or lost, replace it with a USP-compliant amber bottle - not a random jar from the drugstore.
For eye drops specifically, newer designs from companies like Bausch + Lomb use dual protection: amber glass inside, opaque plastic shell outside. These last 25% longer than standard amber bottles after opening. They’re pricier, but if you’re on lifelong glaucoma treatment, it’s worth it.

Temperature and Humidity: The Hidden Enemies
Light isn’t the only threat. Heat and moisture wreck meds too. Most pills and liquids should be kept between 59°F and 77°F (15°C-25°C). That’s room temperature - not your bathroom, not your car, not the kitchen counter next to the stove.Bathrooms are the worst place. Steam from showers raises humidity. Hot water heats the air. That’s why 68% of people store meds in bathrooms - and 42% report discoloration or texture changes. The Arthritis Foundation says even short bursts of heat can reduce effectiveness. If you live somewhere hot, like Melbourne in summer, your kitchen cabinet might get too warm. A small digital thermometer and hygrometer (to measure humidity) can help. Keep it under 60% humidity.
Some meds need cold. Unopened insulin? Refrigerate at 36-46°F (2-8°C). Once opened, most eye drops can stay at room temp for 4-6 weeks - but check the label. Some require refrigeration even after opening. Never freeze them. Never leave them in a hot car. If you travel, use an insulated bag with UV-blocking lining. These keep meds stable for 8-12 hours, even in 90°F heat.
What to Avoid
Here’s what not to do:- Don’t transfer meds to clear containers - even if they’re labeled “for eye drops.”
- Don’t store near windows, even if they’re closed. Sunlight filters through glass.
- Don’t leave them in the car, even in the glovebox. Temperatures can hit 120°F in minutes.
- Don’t use foil pouches unless you’re traveling. They block 100% of light, but you have to take the med out each time. That leads to 32% of people skipping doses.
- Don’t ignore expiration dates. Degraded meds expire faster.
And if you see signs of damage? Discoloration (yellow, brown, cloudy), odd smells (vinegar-like for aspirin), or pills that crumble? Throw them out. The FDA recorded over 1,800 adverse events in 2022 linked to improper storage. Don’t be a statistic.
Smart Solutions for Real Life
You don’t need to buy a fancy box to protect your meds. But if you want peace of mind, here are practical options:- Amber glass bottles: Buy from a pharmacy or medical supplier. Cost: $2-$5 each. Best for long-term use.
- UV-blocking storage boxes: These are like lockers with dark interiors. $20-$60. Good for families with multiple light-sensitive meds.
- Insulated travel bags: With UV lining. $15-$30. Essential for trips or if you work outdoors.
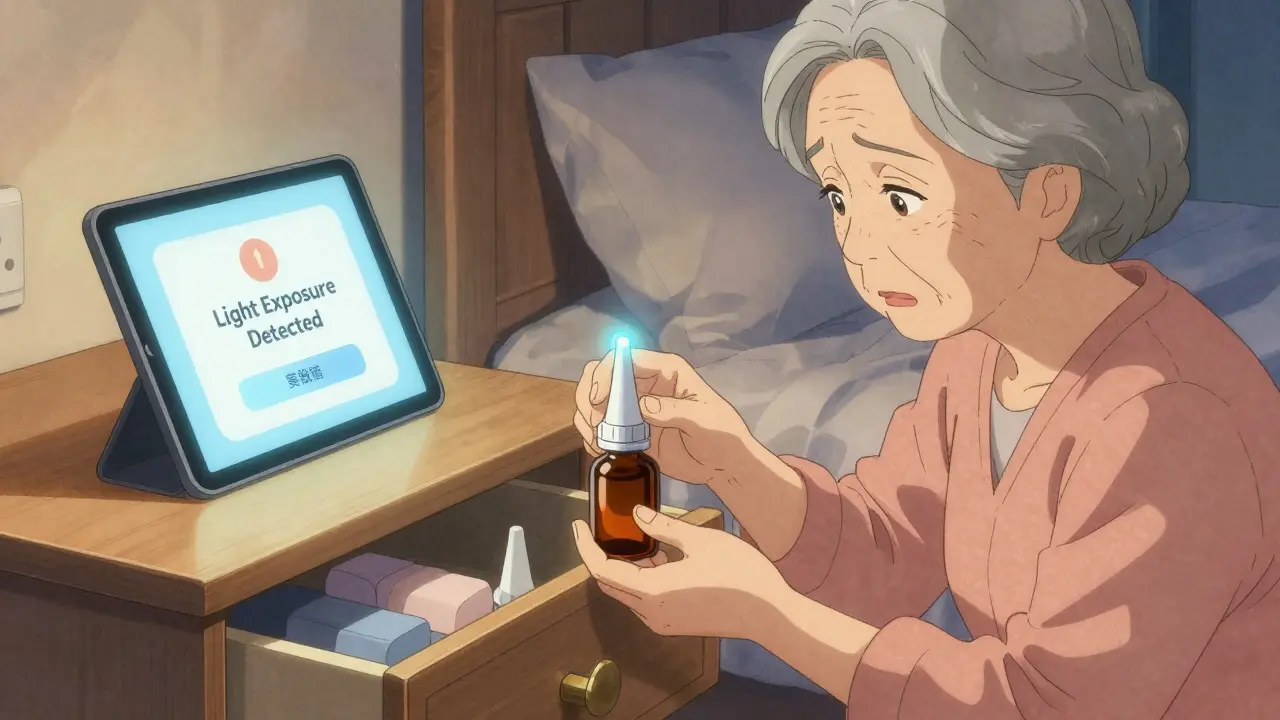
- Smart containers (coming soon): MedMinder and others are testing bottles with UV sensors that alert your phone if light exposure is too high. FDA review expected in late 2023.
Most people do fine with just the original amber bottle - kept in a cool, dark drawer. No gadgets needed. Just consistency.
When in Doubt, Ask
If you’re unsure whether your medication is light-sensitive, don’t guess. Call your pharmacist. Or use the American Society of Health-System Pharmacists’ online storage checker - it covers over 12,000 drugs. The FDA also runs a free hotline: 1-855-543-3784. They’ll tell you exactly how to store it.And if you’re caring for someone elderly or with arthritis? Check the caps. Some amber bottles have child-resistant tops that are hard to open. Ask for easy-open versions. Safety isn’t just about light - it’s about access.
Final Rule: One Place, Always
Pick one spot. A kitchen cabinet away from the sink. A drawer in the bedroom. Not the bathroom. Not the nightstand. Not the purse. Keep it there. Every time. That’s how you avoid degradation, wasted money, and health risks.Light-sensitive meds aren’t fragile because they’re expensive. They’re fragile because they’re powerful. A tiny drop of eye drop can lower eye pressure for 24 hours - if it’s still active. If it’s been sitting in the sun? It’s just salt water. And your vision? That’s not something you can afford to gamble with.
Can I store eye drops in the fridge?
Some eye drops need refrigeration after opening, but not all. Always check the label. Unopened eye drops are often stored in the fridge, but once opened, many can be kept at room temperature (40-77°F) for up to 6 weeks. Refrigerating drops that don’t require it can cause them to thicken or form crystals, making them harder to use. If you do refrigerate, keep them in their original amber bottle and let them sit for a few minutes before use to avoid discomfort.
What if my medication bottle is clear but says "protect from light"?
That’s a red flag. The manufacturer likely designed it for short-term use or transport only. If you’re keeping it long-term, transfer it to an amber glass bottle or keep it inside its original opaque box. Never leave it in a clear bottle on a windowsill. Even if the label says "protect from light," the container itself isn’t doing the protecting.
How do I know if my medication has degraded?
Look for changes: creams or ointments that turn yellow or brown, liquids that become cloudy or form particles, pills that crumble or smell strange (like vinegar for aspirin). If you notice any of these, stop using it. Don’t take a chance. Even if it looks “mostly okay,” light damage can reduce potency by 50% without obvious signs.
Are amber bottles safe for children and pets?
Yes - but not because they’re childproof. Amber bottles are for light protection, not safety. Many still have child-resistant caps, but those can be hard for elderly users to open. If you have kids or pets, store all medications in a locked cabinet - regardless of bottle color. Amber doesn’t prevent accidental ingestion; it only protects from light.
Can I reuse amber bottles for different medications?
No. Never reuse a bottle for a different drug, even if it’s the same type. Residue from the first medication can contaminate the second. That’s especially dangerous with eye drops or insulin. Always use a new, sterile amber bottle from your pharmacy if you need to transfer. Cleaning won’t remove all traces.
Is it okay to store medications in the original box instead of the bottle?
If the bottle is clear and the box is opaque, yes - but only if you keep the bottle inside the box at all times. The box alone isn’t enough if the bottle is exposed. The best practice is to keep the medication in its original amber bottle and leave it in the box for extra protection. That’s double-layered safety: light-blocking bottle + light-blocking box.





