Steroid & Ulcer Risk Calculator
Is PPI Needed for Your Steroid Therapy?
This tool uses current medical evidence to help determine if you need a proton pump inhibitor (PPI) when taking corticosteroids. Based on the article, PPIs are not recommended for most patients taking steroids alone but are essential when combined with NSAIDs or other risk factors.
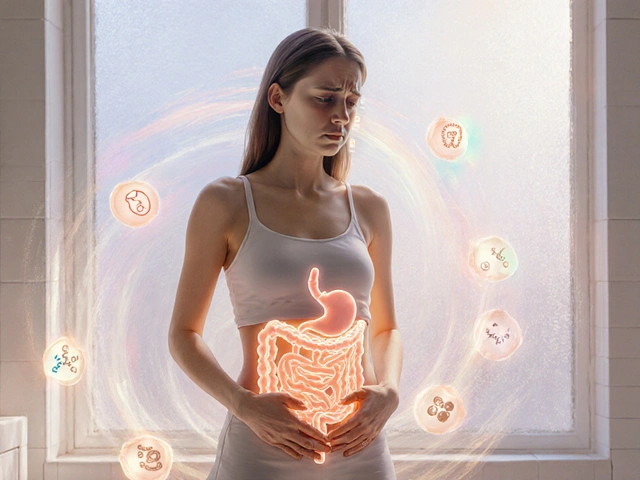
Do Corticosteroids Really Cause Stomach Ulcers?
For decades, doctors have been told to give proton pump inhibitors (PPIs) to anyone on corticosteroids-just in case. But what if that routine isn’t backed by science? The truth is more complicated than the old advice suggests. Corticosteroids like prednisone, dexamethasone, and methylprednisolone are powerful anti-inflammatory drugs used for asthma, rheumatoid arthritis, lupus, and skin conditions. They save lives. But they’ve also been blamed for causing stomach ulcers. The problem? The data doesn’t support that fear for most people.
A 2013 meta-analysis published in Allergy, Asthma & Clinical Immunology looked at dozens of studies involving tens of thousands of patients. It found no significant increase in peptic ulcer disease when corticosteroids were used alone. Even high doses-like 60 mg of prednisone daily-didn’t raise ulcer risk in people not taking other drugs. In fact, only 0.4% to 1.8% of corticosteroid users developed ulcers in those studies. That’s lower than the rate in the general population.
So why do we still hear warnings? Because corticosteroids don’t cause ulcers the way NSAIDs do. They don’t directly damage the stomach lining. Instead, they interfere with healing. If you already have a small ulcer, corticosteroids can keep it from closing. They also mask pain, so you might not notice symptoms until something serious happens-like bleeding or a hole in the stomach wall. That’s why doctors sometimes see dramatic complications in patients on steroids, even if the ulcer started long before.
The Real Danger: When Steroids and NSAIDs Mix
The real risk doesn’t come from corticosteroids alone. It comes from combining them with NSAIDs-drugs like ibuprofen, naproxen, or aspirin. These are the actual ulcer-causers. NSAIDs block protective enzymes in the stomach lining, making it vulnerable to acid. When you add corticosteroids on top, the risk doesn’t just go up-it jumps.
A study of Medicaid patients showed that using both corticosteroids and NSAIDs together increased the risk of peptic ulcer disease by 4.4 times. That’s not a small number. The 95% confidence interval (2-9.7) means this isn’t a fluke. The same study found that patients on both drugs had a much higher chance of bleeding or perforation than those on either drug alone.
Here’s the bottom line: if you’re on a corticosteroid and also taking an NSAID, you need protection. That’s not up for debate. Proton pump inhibitors (PPIs) like omeprazole or pantoprazole are proven to reduce this risk. Misoprostol is another option, though it often causes diarrhea and cramping, which makes it harder for patients to stick with.
Why Most People Don’t Need a PPI on Steroids Alone
Despite the lack of evidence, a 2022 survey of 347 hospitalists found that 78.3% routinely prescribed PPIs to patients on high-dose corticosteroids-even when no NSAIDs were involved. That’s a lot of unnecessary medication. Why? Fear. Tradition. And the fact that doctors don’t want to be the one who misses a bleeding ulcer.
But the tide is turning. In 2023, the Journal of Hospital Medicine published a landmark commentary called “Things We Do for No Reason™,” which specifically called out routine PPI use for steroid monotherapy as unsupported by evidence. The authors pointed out that no major guidelines from the American College of Gastroenterology or the American Gastroenterological Association recommend it.
Real-world results back this up. At Johns Hopkins, a quality improvement project stopped automatic PPI prescriptions for patients on corticosteroids alone. Over 12 months, PPI use dropped by 42.7%-and there was no increase in GI complications. At the University of Wisconsin, a similar program cut inappropriate PPI prescriptions by 35% in just one quarter.
Patients aren’t getting hurt by skipping PPIs when they’re not needed. What they are getting is more side effects from the PPI itself-higher risk of C. diff infection, bone fractures, kidney problems, and nutrient deficiencies like low magnesium and vitamin B12. That’s the hidden cost of unnecessary prophylaxis.
Who Actually Needs Protection?
Not everyone on corticosteroids needs a PPI. But some people do. Here’s who should be protected:
- Patients taking both corticosteroids and NSAIDs
- Those with a history of peptic ulcer or GI bleeding
- Patients on anticoagulants like warfarin or apixaban
- People with Helicobacter pylori infection (test and treat before starting steroids if possible)
- Hospitalized patients on high-dose steroids-especially if they’re critically ill, on mechanical ventilation, or have sepsis
For everyone else-outpatients on steroids alone, no prior ulcers, no NSAIDs, no other risk factors-PPIs aren’t recommended. The absolute risk of bleeding in this group is about 0.12 events per 100 person-years, according to a 2014 BMJ Open review. That’s lower than the risk of a car accident on a daily commute.
How to Monitor for Problems
Even if you’re not on a PPI, you still need to watch for signs of trouble. Corticosteroids can hide symptoms. A patient might have a slow bleed and feel fine until they’re pale, dizzy, and their hemoglobin drops by 4 points.
Here’s what to do:
- Ask about symptoms at every visit: Are you having stomach pain? Nausea? Feeling full quickly? Black, tarry stools? Vomiting blood? These are alarm signs. Don’t wait.
- Check for anemia: A simple CBC test every 3-6 months if on long-term steroids can catch slow bleeding early.
- Don’t rely on endoscopy for screening: Routine scopes aren’t needed unless there are symptoms or signs of bleeding. Endoscopy should be reserved for patients with alarm features.
- Test for H. pylori: If you have a history of ulcers or are planning long-term steroid use, test for this bacteria. Eradicate it with antibiotics before starting steroids if positive.
- Watch for other side effects: Steroids raise blood sugar, cause fluid retention, and weaken bones. Monitor glucose levels after meals, not just fasting. Check blood pressure and weight regularly.
Many patients don’t realize their stomach pain is linked to their steroid. They think it’s just “indigestion.” That’s why doctors need to ask directly. A simple question: “Have you had any new stomach pain, black stools, or vomiting since you started the steroid?” can prevent disaster.

What’s Changing in 2025?
Guidelines are finally catching up to the science. The American Gastroenterological Association is currently reviewing its stance on corticosteroid-related GI risk, with a new update expected in late 2025. A clinical trial registered on ClinicalTrials.gov (NCT05214345) is tracking GI outcomes in patients on high-dose steroids with and without PPIs-results are due by the end of this year.
More hospitals are adopting “PPI stewardship” programs-like the one at Johns Hopkins-where automatic prescriptions are turned off unless specific risk factors are present. Pharmacists are now part of the team, reviewing every steroid prescription for unnecessary PPIs.
What’s clear now is that blanket prevention doesn’t work. Personalized care does. You don’t protect every patient on steroids-you protect the ones at real risk.
What to Do Next
If you’re on corticosteroids:
- Ask your doctor: “Am I taking any NSAIDs? Do I have a history of ulcers or bleeding? Am I on blood thinners?”
- If you’re on NSAIDs or have any of those risk factors, ask about PPIs.
- If you’re on steroids alone and have no other risks, ask: “Is this PPI really necessary?”
- Report any new stomach pain, black stools, or vomiting immediately.
- Don’t stop your steroid suddenly. Work with your doctor to taper safely.
If you’re a clinician:
- Stop prescribing PPIs automatically for steroid monotherapy.
- Use a checklist: NSAIDs? Prior ulcer? Anticoagulants? H. pylori? Hospitalized?
- Test for H. pylori in high-risk patients before starting steroids.
- Monitor for anemia and symptoms-not just labs.
The era of guessing is over. We have data now. Use it.



ryan smart
November 13, 2025 AT 05:09Stop the fearmongering. Let the body heal itself.
Sanjoy Chanda
November 14, 2025 AT 18:59It's not about being cheap-it's about being smart. We need to stop treating patients like they're all the same. Just ask the right questions. Simple. Human.
Sufiyan Ansari
November 15, 2025 AT 20:37One must interrogate the ethics of prescribing without evidence. The burden of proof has been inverted: instead of demonstrating harm, we now demand proof of safety. This inversion, though well-intentioned, erodes the integrity of evidence-based medicine. The data, as presented, compels a return to praxis grounded in observation, not fear.
megha rathore
November 16, 2025 AT 12:31prem sonkar
November 18, 2025 AT 07:06Michal Clouser
November 18, 2025 AT 16:56It’s heartening to see institutions like Johns Hopkins and Wisconsin leading the charge. I’ve already revised our hospital’s protocol-no more automatic PPIs for steroid monotherapy. We now use a simple checklist.
Patients are grateful. And yes, we’re seeing fewer C. diff cases already. The data speaks. We just needed to listen.
Earle Grimes61
November 19, 2025 AT 08:30And don’t get me started on the ‘H. pylori’ testing. That’s a scam too. They test you, then charge you $800 for antibiotics you don’t need. The whole GI system is a money pit.
They want you to believe you’re broken. You’re not. Your body’s fine. They just want your money.
Corine Wood
November 20, 2025 AT 22:17Every time we prescribe unnecessarily, we expose patients to risk without benefit. And every time we listen, we restore trust.
Thank you for writing this. It’s not just a clinical update-it’s a moral reminder.