Most people don’t realize that nearly 7 in 10 people under 50 carry one type of herpes virus. It’s not rare. It’s not shameful. It’s just common-and often misunderstood. Herpes Simplex Virus (HSV) comes in two forms: HSV-1 and HSV-2. Both are lifelong infections, but they don’t always mean what you think they do. You might have gotten HSV-1 from a kiss as a kid, not from sex. You might have HSV-2 and never had a single outbreak. The truth is, herpes isn’t just about sores. It’s about understanding how it spreads, how it behaves, and how to manage it-especially when it comes to antiviral therapy.
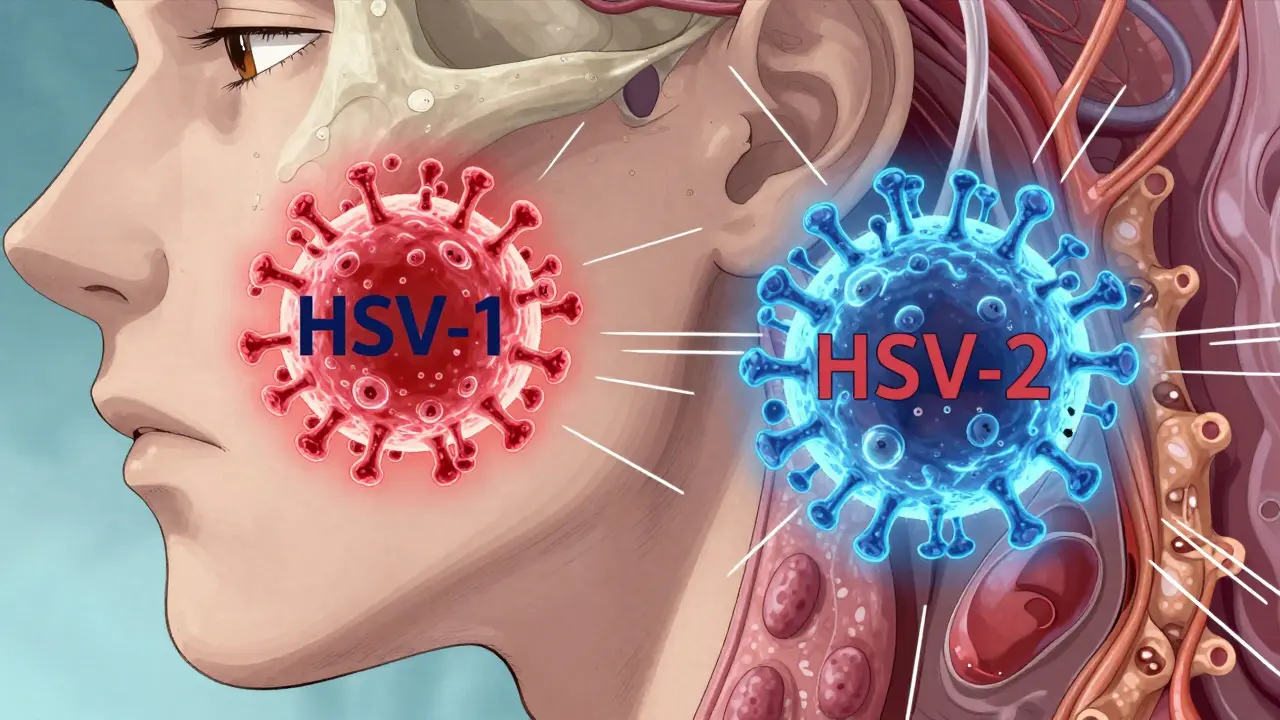
HSV-1 vs. HSV-2: What’s the Real Difference?
HSV-1 and HSV-2 look almost identical under a microscope. Both are double-stranded DNA viruses with a protein shell and a fatty outer layer. But where they live in your body and how they behave are completely different.
HSV-1 usually hangs out in the trigeminal ganglion, a cluster of nerves behind your cheekbone. That’s why it’s best known for cold sores around the mouth. But here’s the twist: today, HSV-1 causes 30-50% of new genital herpes cases in high-income countries. That’s not a mistake. It’s a shift. More young adults are getting genital HSV-1 through oral sex, and it’s now the leading cause of first-time genital herpes in people under 30.
HSV-2, on the other hand, prefers the sacral ganglion near your lower spine. It’s the classic cause of genital herpes-recurring, painful, and more likely to shed virus without symptoms. About 1 in 8 people aged 15-49 have HSV-2 globally. Women are more likely to be infected than men, and Black Americans are affected at nearly three times the rate of white Americans.
Here’s the key difference: HSV-1 genital infections recur about 0.2 to 0.5 times a year. HSV-2? 4 to 5 times a year. And while HSV-1 sheds virus on the skin about 5-10% of days, HSV-2 sheds on 10-20% of days-even when there are no sores. That’s why transmission risk is higher with HSV-2.
What Do Herpes Outbreaks Actually Look Like?
Not everyone gets the same symptoms. Some people have no signs at all. Others have a nightmare first outbreak.
For a first-time HSV-1 infection in kids, it’s often herpetic gingivostomatitis: fever over 38.5°C, swollen gums, mouth ulcers so painful they can’t eat or drink. About 1 in 10 kids end up in the hospital. Adults with their first oral HSV-1 might just get a single blister on the lip that heals in a week.
Genital outbreaks are more intense. The first HSV-2 outbreak hits hard: 93% of people get painful ulcers, 78% feel burning when they pee, and 65% have swollen lymph nodes in the groin. Fever, muscle aches, and discharge are common. It can last 2-4 weeks. After that, most people get recurrences-but they’re usually milder. A typical HSV-2 recurrence lasts 5-10 days, with just a few small blisters and less pain.
HSV-1 genital outbreaks are even milder. Most people have fewer than one recurrence a year. Some never have another one after the first.
Prodrome-the warning sign-is crucial. Many feel tingling, itching, or burning in the area 1-6 hours before a sore appears. That’s your window to start treatment.
How Antiviral Therapy Works-And When to Use It
There are three main antivirals: acyclovir, valacyclovir, and famciclovir. They don’t cure herpes. But they stop the virus from multiplying. That’s huge.
For a first outbreak, doctors recommend acyclovir 400mg three times daily for 5-10 days. Valacyclovir (1g twice daily) or famciclovir (250mg three times daily) work just as well and are easier to take. Starting within 24 hours of symptoms cuts healing time by half. Delay it 72 hours, and you’re back to 19 days of pain.
For recurring outbreaks, you don’t need to take pills every day. Episodic therapy-taking the drug only when you feel the tingling-works for most people. A single dose of valacyclovir 2g at the first sign can prevent the sore from forming. Or take 500mg twice daily for 3 days. Studies show this reduces outbreak duration from 10 days to 5.
But if you have frequent outbreaks-say, six or more a year-daily suppressive therapy makes sense. Taking valacyclovir 500mg once a day cuts transmission to partners by 48%. It also reduces outbreaks by 70-80%. For people with HIV or weakened immune systems, higher doses are needed. IV acyclovir (5-10mg/kg every 8 hours) is standard for severe cases.
Herpes Beyond the Genitals: Eye, Brain, and Baby Risks
Herpes isn’t just a genital or mouth issue. It can go places you don’t expect.
Herpes keratitis-eye infection-is the leading infectious cause of corneal blindness in the U.S. Almost all cases are HSV-1. It starts with redness, light sensitivity, and blurred vision. Left untreated, it can scar the cornea. Treatment? Trifluridine eye drops every hour while awake. It cuts healing time from 21 days to 14.
Herpes encephalitis is rare-just 2 cases per million people-but deadly. 95% of cases are caused by HSV-1. It attacks the temporal lobe, causing seizures, confusion, and personality changes. Survival depends on starting IV acyclovir within hours. Delayed treatment? Death rate jumps to 70%.
Neonatal herpes is terrifying. It happens in about 1 in 3,200 births. Most cases (70%) come from HSV-2, but HSV-1 is more likely to kill the baby. If a mother has an active outbreak at delivery, a C-section cuts transmission risk from 30-50% to under 3%. That’s why doctors screen for outbreaks near term. New WHO guidelines now recommend universal HSV-2 screening for pregnant women with a history of outbreaks.
Resistance, Side Effects, and What’s Next
Most people tolerate antivirals fine. Headache and nausea are the most common complaints. But in people with advanced HIV (CD4 under 100), 10% of HSV strains are now resistant to acyclovir. That’s not rare-it’s a growing problem. When that happens, foscarnet or the newer drug pritelivir are used. In March 2023, the FDA approved pritelivir for acyclovir-resistant HSV. It cuts viral shedding by 87% in just 48 hours.
Cost is another barrier. Valacyclovir 500mg costs $35-$60 a month with insurance. Without it? $300-$400. Many skip doses because of price. Only 65% stick with daily therapy for a full year.
What’s coming? New drugs are in trials. Helicase-primase inhibitors like pritelivir and amenamevir work faster than acyclovir. Therapeutic vaccines (GEN-003, Simplirix) are showing promise in reducing shedding by 50%. But they’re not ready yet. For now, antivirals remain the gold standard.

Living With Herpes: Real Stories, Real Challenges
Psychological impact is often worse than the physical symptoms. A survey of 1,500 people with herpes found 74% felt stigma-related anxiety. 45% had relationship problems. 32% waited over six months to tell a partner.
On Reddit, one user wrote: “First outbreak lasted 18 days with fever to 39.2°C. Couldn’t pee without numbing spray. But daily valacyclovir cut my next outbreaks to 2-3 days with just one tiny sore.” Another said: “I switched from acyclovir to famciclovir because the nausea was unbearable. No side effects now.”
Support matters. ASHA’s hotline handles 12,000 calls a year. CDC’s online resources get 3.2 million visits annually. Knowledge reduces fear. Talking reduces shame.
You don’t have to be defined by herpes. You don’t have to be silent. You don’t have to suffer in silence. With the right treatment, you can live a full, healthy, intimate life.
Can you get herpes from sharing towels or toilet seats?
No. Herpes doesn’t survive long outside the body. Transmission requires direct skin-to-skin contact with an active area-usually during an outbreak or asymptomatic shedding. Towels, toilet seats, and swimming pools are not transmission routes. The virus dies quickly in dry, cool environments.
If I have HSV-1, can I still get HSV-2?
Yes. Having HSV-1 gives you some partial protection against HSV-2, but it’s not complete. About 30-40% of people with oral HSV-1 still get genital HSV-2 if exposed. The immune response from HSV-1 reduces severity and frequency of HSV-2 outbreaks, but it doesn’t block infection.
How accurate are herpes blood tests?
Modern type-specific blood tests (like HerpeSelect or EUROIMMUN recomLine) are over 97% accurate for detecting HSV-1 and HSV-2 antibodies-but only after 12-16 weeks post-infection. Testing too early gives false negatives. They can’t tell you when you got it or if you’re currently shedding. They only show past exposure.
Is it safe to have sex if I’m on antiviral therapy?
Yes, but with precautions. Daily antiviral therapy reduces transmission risk by 48-70%. Using condoms adds another 30% protection. Avoid sex during outbreaks and when you feel prodromal symptoms. Even with treatment, shedding can still happen-so open communication with partners is essential.
Can herpes cause infertility?
No. Herpes doesn’t affect sperm or egg quality. It doesn’t cause scarring in reproductive organs. The only risk to fertility is indirect: if someone avoids sex or relationships due to fear of transmission, that can delay family planning. But the virus itself does not impair reproductive function.
Are there natural remedies that work for herpes?
Lysine supplements, tea tree oil, or zinc creams might help soothe symptoms, but none have been proven to reduce outbreaks or transmission. Only FDA-approved antivirals-acyclovir, valacyclovir, famciclovir-have strong clinical evidence. Relying on unproven remedies can delay effective treatment and increase risk of complications.
What to Do Next
If you think you have herpes, get tested. Don’t wait. PCR swabs from active sores are 95-98% accurate. Blood tests confirm type after 16 weeks. If you’re diagnosed, talk to your doctor about treatment options. Episodic or suppressive therapy? Both work. The choice depends on how often you break out and your comfort with transmission risk.
If you’re in a relationship, talk to your partner. Share your diagnosis. Use protection. Take your meds. You’re not a burden-you’re someone managing a common virus with proven tools.
Herpes isn’t a life sentence. It’s a condition. And like high blood pressure or diabetes, it’s manageable-with knowledge, medication, and support.






Elizabeth Cannon
January 26, 2026 AT 03:26ok but like… herpes is just a vibe now?? i got cold sores from my cousin at thanksgiving in 2012 and i never thought twice about it. now i’m just waiting for someone to tell me i’m ‘high risk’ bc i kissed someone once. chill.
Helen Leite
January 26, 2026 AT 10:10THEY’RE HIDING THE TRUTH 😱 HSV IS A BIOWEAPON DESIGNED TO CONTROL SEXUAL BEHAVIOR. THEY WANT YOU AFRAID SO YOU’LL BUY MORE DRUGS. 🤫💊 #HerpesGate
Marie-Pier D.
January 27, 2026 AT 17:32hey i just want to say this post was so gentle and informative 🥹 i had my first outbreak last year and i felt like a monster - reading this made me feel seen. you’re not broken, you’re just human. 💛
Alexandra Enns
January 28, 2026 AT 03:28Wow. Just… wow. This article is basically a propaganda piece for Big Pharma. You’re telling me we’re supposed to believe that a $400/month drug is the only solution? In Canada, we’ve had people using ice packs and lysine since the 90s. This isn’t medicine - it’s capitalism with a stethoscope.
And don’t even get me started on the ‘shedding’ myth. If the virus is so contagious without symptoms, why isn’t everyone infected by age 10? It’s all about fear marketing. Wake up.
Also, why are we still calling it ‘herpes’ like it’s a crime? It’s a virus. Like the common cold. But somehow, cold sores are ‘cute’ and genital herpes is ‘dirty’? That’s not science - that’s puritanism.
And who wrote this? Some CDC ghostwriter with a degree in fearmongering? I’ve had HSV-1 since I was 7. Never had a genital outbreak. Never transmitted anything. My partner knows. We’re fine. We don’t need your pills.
Stop pathologizing normal biology. Stop monetizing shame. And for god’s sake, stop pretending this is a ‘public health crisis’ when the real crisis is the stigma you’re reinforcing.
Karen Conlin
January 29, 2026 AT 00:42I’m a nurse and I see this every day - people terrified to even say the word herpes out loud. This post? It’s the exact kind of calm, factual info we need more of. You don’t need to be ashamed. You don’t need to be perfect. You just need to know how to protect yourself and others. And yes, antivirals work. They’re not magic, but they’re not evil either. 💪
Also - if you’re on suppressive therapy and still worried? Talk to your partner. Say: ‘I have this. Here’s what it means. Here’s how we manage it.’ That’s intimacy. Not secrecy.
Sushrita Chakraborty
January 29, 2026 AT 04:36It is imperative to note that the epidemiological data presented herein is largely derived from high-income nations, and may not be representative of global patterns. In many low-resource settings, diagnostic access remains limited, and asymptomatic shedding is underreported due to lack of surveillance infrastructure. Furthermore, the cost of antivirals remains prohibitive for the majority of the global population, rendering the notion of 'manageable' herpes a privilege of economic status. We must not conflate medical efficacy with accessibility.
Sawyer Vitela
January 29, 2026 AT 14:04HSV-2 shedding is 10-20% of days? That’s a lie. CDC’s own 2021 data shows 7-12%. You’re inflating numbers to scare people into taking drugs.
Marlon Mentolaroc
January 30, 2026 AT 13:10Bro, I had HSV-1 as a kid and now I get genital outbreaks from stress. No sex involved. Just my immune system being a drama queen. Valacyclovir saved my dating life. No shame. Just science.
Chloe Hadland
January 31, 2026 AT 21:44thank you for writing this. i didn’t know hsv-1 could be genital and i’ve been feeling guilty for years over something that’s just… biology. i’m gonna stop crying about it now. ❤️
Husain Atther
February 2, 2026 AT 01:53While the medical information provided is largely accurate, I would like to emphasize that cultural perceptions of herpes vary significantly across societies. In many South Asian communities, open discussion of genital health remains taboo, which can delay diagnosis and increase psychological distress. Educational outreach must be culturally adapted to be effective.
Gina Beard
February 3, 2026 AT 00:35Shame is the real virus.
Izzy Hadala
February 3, 2026 AT 19:05Given the documented prevalence of HSV-1 as a causative agent in genital herpes among young adults in high-income countries, one must question the adequacy of current public health messaging, which continues to disproportionately associate genital herpes with HSV-2. This misalignment between epidemiological reality and popular perception may contribute to the persistence of stigma and the underestimation of transmission risk associated with oral-genital contact. Further, the assertion that HSV-1 genital infections are 'milder' requires longitudinal validation, as clinical severity may be confounded by prior immune exposure. A more nuanced public education strategy is warranted.