Erosive Esophagitis Risk Assessment Tool
This tool estimates your risk of developing serious complications from erosive esophagitis based on key factors discussed in the article. Use this as a guide to discuss next steps with your healthcare provider.
Your Risk Assessment
Urgent Warning Signs
If you experience any of these symptoms, seek emergency care immediately:
Key Takeaways
- Erosive esophagitis can lead to serious complications like Barrett’s esophagus, strictures, bleeding, and even cancer.
- Early symptoms often mimic heartburn, but persistent pain, difficulty swallowing, or vomiting blood require urgent care.
- Long‑term acid control with proton pump inhibitors (PPIs) and lifestyle changes dramatically lower complication risk.
- Regular endoscopic surveillance is recommended for patients with severe disease or alarm symptoms.
- Knowing the warning signs helps you act fast and avoid permanent damage.
What Is Erosive Esophagitis?
Erosive Esophagitis is a condition where stomach acid repeatedly damages the lining of the esophagus, causing inflammation and visible erosions. It usually stems from chronic gastro‑esophageal reflux disease (GERD), where the lower esophageal sphincter fails to keep acid out. Over time, the acid‑burned tissue thins, tears, and may bleed.
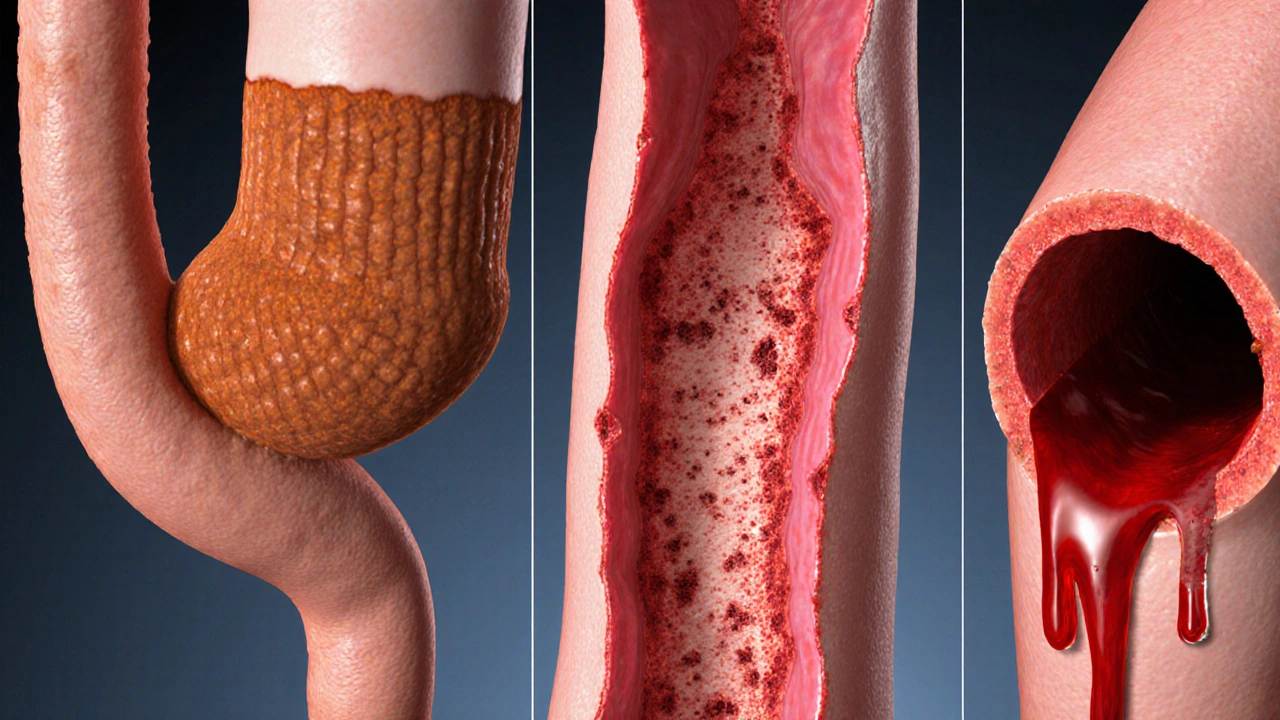
How Complications Develop
When the esophageal lining is constantly assaulted, several pathogenic pathways open up:
- Repeated injury triggers cellular changes that can evolve into Barrett's Esophagus, a precancerous condition where normal squamous cells turn into columnar cells.
- Scar tissue forms as the body tries to heal, leading to Esophageal Stricture, a narrowing that makes swallowing painful.
- Deep erosions may ulcerate and erode into blood vessels, causing Esophageal Bleeding.
- In rare cases, chronic inflammation sets the stage for Esophageal Cancer, especially adenocarcinoma.
Understanding these pathways helps clinicians intervene before damage becomes irreversible.
Major Complications Overview
| Complication | Typical Prevalence | Key Symptoms | Usual Management |
|---|---|---|---|
| Barrett's Esophagus | 5‑10% of severe GERD patients | Persistent heartburn, occasional sour taste | Endoscopic surveillance, radiofrequency ablation |
| Esophageal Stricture | 2‑4% of chronic erosive cases | Difficulty swallowing solids, food getting stuck | Dilation procedures, ongoing acid suppression |
| Esophageal Ulcer | 1‑3% of untreated patients | Sharp chest pain, night-time pain, possible vomiting blood | High‑dose PPIs, protective sucralfate, avoid NSAIDs |
| Esophageal Bleeding | ~0.5% but can be life‑threatening | Hematemesis, melena, sudden severe pain | Endoscopic hemostasis, blood transfusion, intensive care |
| Esophageal Cancer | ~0.2% in long‑standing Barrett’s | Weight loss, dysphagia, persistent pain | Surgery, chemoradiation, targeted therapy |
Red‑Flag Symptoms That Need Immediate Attention
If you notice any of these signs, call emergency services or head to the nearest hospital:
- Vomiting blood or material that looks like coffee grounds. \n
- Black, tarry stools (melena) indicating digested blood.
- Sudden, severe chest pain that doesn’t improve with antacids.
- Inability to swallow any food or liquids.
- Unexplained weight loss or persistent vomiting.

Prevention & Management Strategies
Most complications can be avoided with a two‑pronged approach: medication and lifestyle tweaks.
Medication: Proton Pump Inhibitors
Proton Pump Inhibitors (PPIs) such as omeprazole, esomeprazole, or lansoprazole reduce acid production by up to 90%. For patients with erosive esophagitis, a once‑daily high dose for 8‑12 weeks is the standard regimen, followed by maintenance therapy if symptoms recur.
Endoscopic Surveillance
When erosions are severe (grade C‑D on the Los Angeles classification) or Barrett’s has developed, an endoscopy every 2‑3 years helps catch dysplasia early. Biopsies taken during the procedure confirm cellular changes.
Lifestyle Modifications
Simple daily habits cut reflux dramatically:
- Keep the head of the bed raised 6‑8 inches.
- Eat smaller meals; avoid large meals within 3hours of bedtime.
- Limit acidic or spicy foods, caffeine, chocolate, and mint.
- Quit smoking; tobacco weakens the sphincter.
- Maintain a healthy weight-each 5% of excess body weight raises reflux risk by ~25%.
When to Seek Medical Help
Even if you don’t have a red‑flag, schedule a doctor’s visit when:
- Heartburn persists despite over‑the‑counter antacids for more than two weeks.
- You experience frequent regurgitation or a sour taste in the mouth.
- Swallowing becomes uncomfortable or you notice food sticking.
- You need to use acid‑blocking medication for more than four weeks.
Early evaluation allows a gastroenterologist to order an endoscopy, prescribe the right PPI dose, and set up a surveillance schedule if needed.
Frequently Asked Questions
Can erosive esophagitis heal completely?
Yes, with proper acid suppression and lifestyle changes the lining can regenerate in weeks to months. However, severe cases may leave scar tissue that needs monitoring.
Is Barrett’s esophagus inevitable after erosive esophagitis?
No. Only a minority (about 5‑10%) of patients with long‑standing, untreated reflux develop Barrett’s. Early treatment dramatically lowers that risk.
Do antacids work for severe erosive esophagitis?
Antacids provide short‑term relief but don’t heal erosions. PPIs are the gold‑standard for healing and preventing complications.
How often should I get an endoscopy?
If you have Barrett’s, surveillance every 2‑3years is typical. Without Barrett’s, repeat endoscopy is usually reserved for persistent symptoms or alarm signs.
Can diet alone cure erosive esophagitis?
Diet helps control reflux, but most patients need medication to allow the tissue to heal fully.
What is the link between obesity and esophageal complications?
Excess abdominal pressure pushes stomach contents upward, increasing reflux frequency and the chance of erosive damage, strictures, and Barrett’s.
erosive esophagitis complications can be frightening, but with the right knowledge and early action you can keep your esophagus healthy and avoid long‑term damage.





Mariah Dietzler
October 12, 2025 AT 01:57this risk tool looks kinda useless lol.
Nicola Strand
October 14, 2025 AT 09:30While the article enumerates several complications, it fails to appreciate the nuanced interplay between acid exposure duration and mucosal healing, thereby presenting an oversimplified risk model.
Jackie Zheng
October 16, 2025 AT 11:30I must point out that the term "erosive esophagitis" is frequently misspelled as "erosive oesophagitis" in many lay articles; the correct spelling is essential for accurate literature searches.
Hariom Godhani
October 19, 2025 AT 08:57When I first noticed that burning sensation after meals, I dismissed it as mere heartburn, thinking it would fade away on its own. Over months, the pain grew more relentless, and I began to fear swallowing even water. A friend suggested that I might be developing erosive esophagitis, and I reluctantly booked an endoscopy. The results confirmed my worst fears: inflammation, erosions, and a looming risk of Barrett's esophagus. The doctor offered me a risk assessment tool, promising a clearer picture of future complications. I filled it out with a mixture of hope and dread, watching each factor-duration of symptoms, smoking status, BMI-tick the boxes. The tool placed me in a high‑risk category, and suddenly the abstract statistics became a personal alarm bell. I was instructed to start a high‑dose proton pump inhibitor regimen, adopt dietary changes, and quit smoking immediately. Within weeks, the burning receded, but the psychological weight of a possible progression lingered. I started tracking my diet meticulously, avoiding spicy foods, citrus, and late‑night meals. My physician scheduled quarterly follow‑ups, each appointment a reminder of the delicate balance between control and relapse. Friends often ask why I’m so meticulous; I tell them it’s the fear of irreversible damage that keeps me disciplined. Over a year, inflammation scores improved, yet the tool’s risk profile nudged me to remain vigilant. I now view this assessment not as a fatalistic prediction but as a roadmap, guiding lifestyle choices and medical adherence. The journey taught me that early detection, coupled with sustained effort, can indeed tilt the odds in our favor, even when the odds initially seemed bleak.
Jackie Berry
October 21, 2025 AT 22:04Reading through the risk assessment, I was struck by how interconnected the variables are-duration of GERD symptoms, smoking habits, and even body mass index create a tapestry of risk that isn’t captured by a simple yes/no answer. For example, a three‑year history of symptoms combined with a modest BMI might place you in a moderate zone, but throw in a current smoking habit and the risk jumps noticeably. It reminds me of how lifestyle factors can amplify each other, a concept that’s often glossed over in short articles. I’ve seen patients who reduced their smoking but didn’t address weight gain, and their risk profile barely shifted. Conversely, a patient who lost ten pounds and stopped smoking saw a dramatic dip in predicted complications, even though the GERD duration remained the same. The tool’s visual risk scores-low, moderate, high-are helpful for quick conversations, but it’s essential to remember they’re a snapshot, not a crystal ball. Regular reassessment is key; as habits change, so does the risk. I’d also suggest that clinicians use this as a springboard for deeper education, rather than a definitive verdict. In practice, I find that patients who understand the “why” behind each factor are more motivated to make sustainable changes. So, while the calculator is a solid starting point, the real work happens in the ongoing dialogue between patient and provider, adjusting the variables over time and watching the risk level respond.
Mikayla May
October 24, 2025 AT 08:24If you have been symptomatic for more than three years, your risk score will likely fall into the moderate or high category, so schedule an endoscopy soon.
Jimmy the Exploder
October 26, 2025 AT 12:10this thing is just a gimmick no real use
Robert Jackson
October 28, 2025 AT 14:10Contrary to your assertion, the risk assessment algorithm is grounded in peer‑reviewed epidemiological data and has demonstrated predictive validity in multiple cohort studies.
Robert Hunter
October 30, 2025 AT 13:24From a global health perspective, such tools must be adapted to local dietary patterns and H. pylori prevalence to ensure relevance.
Shruti Agrawal
November 1, 2025 AT 09:50good summary but needs more data.
Katey Nelson
November 3, 2025 AT 03:30Wow, this tool actually makes me think about my own GERD journey 😊. It's weird how a simple questionnaire can feel so personal.
Joery van Druten
November 4, 2025 AT 18:24I appreciate the sentiment, though the tool's limitations should be highlighted to avoid false reassurance.
Melissa Luisman
November 6, 2025 AT 06:30Stop sugarcoating the fact that untreated erosive esophagitis can lead to Barrett's esophagus!
Akhil Khanna
November 7, 2025 AT 15:50Let's not forget that access to endoscopy isnt universal, so risk scores might not translate into actionable care for everyone.
Zac James
November 8, 2025 AT 22:24Interesting read, especially the BMI stratification; I wonder how obesity interacts with smoking in this context.
Arthur Verdier
November 10, 2025 AT 02:10Sure, the pharma companies designed this tool to push PPIs on everyone, right? 🙄
Breanna Mitchell
November 11, 2025 AT 03:10Remember folks, early detection and lifestyle changes can dramatically reduce complications!
Alice Witland
November 12, 2025 AT 01:24Ah, another risk calculator-because we needed more numbers in our lives.
Chris Wiseman
November 12, 2025 AT 20:50One could argue that quantifying suffering reduces the human experience to mere percentages, yet we persist in this numerical obsession.
alan garcia petra
November 13, 2025 AT 13:30Bottom line: talk to your doc, follow the plan, stay safe.