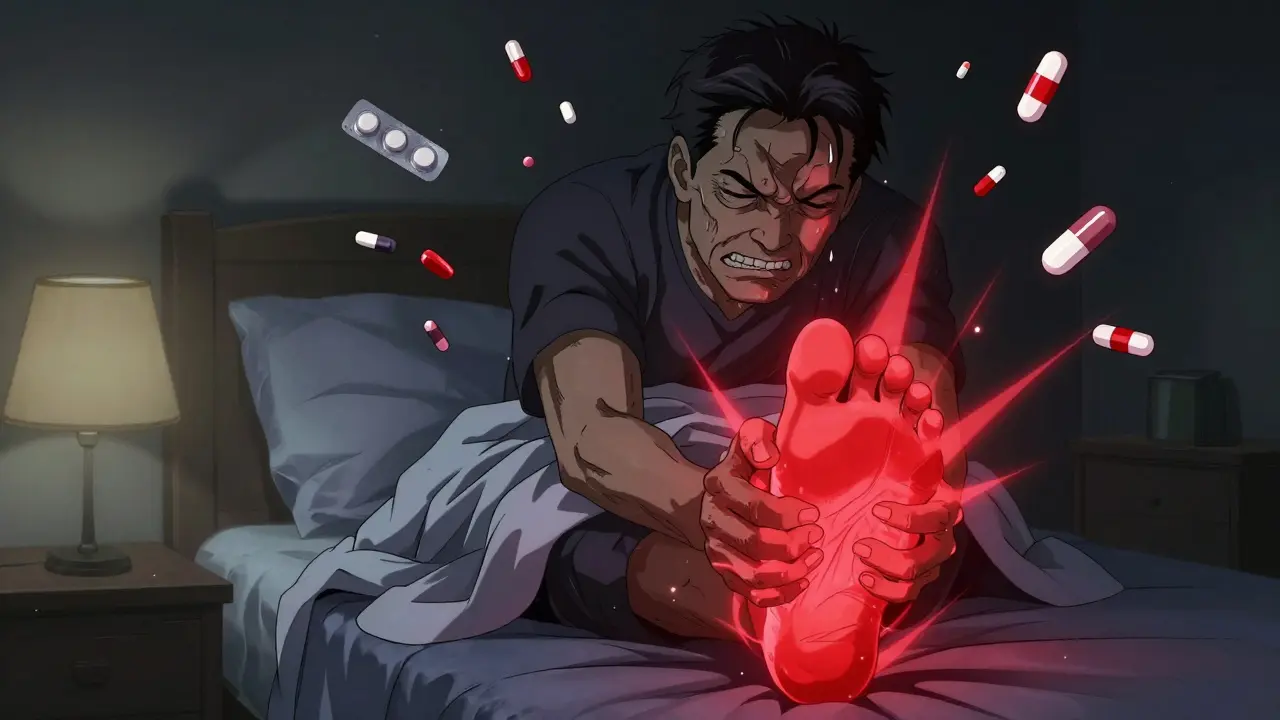
When your big toe explodes in pain, you don’t care about drug classes - you just want it to stop.
You wake up at 3 a.m. Your big toe feels like it’s been smashed with a hammer. The skin is shiny, red, hot to the touch. Even the weight of a bedsheet hurts. This isn’t just a bad day - it’s a gout flare. And if you’ve had one before, you know the clock is ticking. Treatment needs to start within 24 hours, or the pain lasts longer, deeper, and harder to control.
Three drugs dominate the emergency response: NSAIDs, colchicine, and steroids. All three work. But which one is right for you? The answer isn’t about which is strongest. It’s about what your body can handle.
NSAIDs: The Go-To - But Only If Your Body Lets You
NSAIDs - like naproxen, ibuprofen, and indomethacin - are the most common first choice for gout flares. They’re fast, cheap, and widely available. But here’s the catch: you need to take them at full anti-inflammatory doses, not the little pills you use for headaches.
- Naproxen: 500 mg twice daily
- Ibuprofen: 800 mg three times daily
- Indomethacin: 50 mg three times daily
That’s a lot. And it’s not safe for everyone. If you have high blood pressure, kidney problems, heart disease, or a history of stomach ulcers, NSAIDs can make things worse - not better. They’re the reason so many older adults end up in the ER with bleeding ulcers or kidney failure.
Only three NSAIDs have FDA approval specifically for gout: indomethacin, naproxen, and sulindac. But doctors often use others like diclofenac or celecoxib at high doses. The truth? Any NSAID, at the right dose, can knock down gout pain. But if your body can’t handle the side effects, it’s not worth the risk.
Colchicine: The Precision Tool - But One Misstep Can Be Dangerous
Colchicine used to be given in massive doses: 4.8 mg over six hours. That caused vomiting, diarrhea, and sometimes worse. Today, the game has changed.
Now, the standard is 1.8 mg total - taken as 1.2 mg at the first sign of pain, then 0.6 mg one hour later. That’s it. Studies show this low-dose version works just as well as the old high-dose regimen - but with far fewer side effects.
Why does this matter? Because colchicine has a razor-thin safety margin. Too much, and you risk rhabdomyolysis (muscle breakdown), seizures, or even organ failure. It’s especially dangerous if you have kidney disease or are taking statins or certain antibiotics.
It’s not the first choice for most people - but for those who can’t take NSAIDs and want to avoid steroids, it’s a solid option. Just don’t mess with the dose. Stick to the low-dose protocol. And if you’re on other meds, check with your doctor before starting.
Steroids: The Quiet Winner for Many Patients
Steroids - like prednisone - are often overlooked. People hear “steroid” and think of bodybuilders or scary side effects. But a short, controlled course for gout? It’s one of the safest, most effective tools we have.
Oral prednisone is typically started at 40-60 mg per day for two to three days, then slowly tapered over 10-14 days. Why taper? Because if you stop too fast, the flare can come back harder than before.
For gout in just one joint - say, your knee or ankle - an injection right into the joint is even better. No pills. No stomach upset. No kidney stress. Just targeted relief. And because it’s local, the systemic side effects are minimal.
Here’s why many rheumatologists now prefer steroids as first-line: they’re easier on the stomach, kidneys, and heart than NSAIDs. They’re safe for people with diabetes if blood sugar is monitored. They work just as well as NSAIDs at reducing pain - and in some cases, better.
Medical guidelines say it plainly: if you can’t take NSAIDs or colchicine, steroids are your best bet. But increasingly, they’re being used even when you can take the others - because they’re just that reliable.

Comparing the Three: Efficacy, Safety, and Who Should Use What
Let’s cut through the noise. Here’s what the science says about how these three stack up.
| Feature | NSAIDs | Colchicine (Low-Dose) | Steroids (Oral/Intra-articular) |
|---|---|---|---|
| Pain Relief (72 hours) | 73% of patients | 70-75% of patients | 73% of patients |
| Typical Dose | Naproxen 500 mg BID, Indomethacin 50 mg TID | 1.2 mg + 0.6 mg (1.8 mg total) | Prednisone 40-60 mg/day, then taper |
| Best For | Healthy patients with no kidney, heart, or stomach issues | Patients who can’t take NSAIDs and want to avoid steroids | Patients with kidney disease, heart failure, ulcers, or single-joint flare |
| Major Risks | GI bleeding, kidney damage, high blood pressure | Diarrhea, muscle toxicity (if overdosed or with drug interactions) | Rebound flare (if not tapered), high blood sugar |
| Cost | $5-$15 for a 5-day course (generic) | $10-$25 for low-dose course | $5-$20 for oral prednisone; injection adds $50-$150 |
| Speed of Relief | 24-48 hours | 24-48 hours | 12-36 hours (injection faster) |
Here’s the surprising truth: all three work about the same. No one drug is clearly better at reducing pain. The deciding factor isn’t effectiveness - it’s safety.
Who Gets Which Drug? Real-World Decisions
Let’s say you’re 68, have high blood pressure, take a blood thinner, and had a stomach ulcer last year. NSAIDs? Out. Colchicine? Risky if your kidneys aren’t perfect. Steroids? Your best option.
Or you’re 52, healthy, no other meds, and your knee swells up. NSAIDs are fine. But if you’re on a statin? Colchicine becomes dangerous. Even if you’re young, you might still get a steroid injection - especially if it’s just one joint. Why? Because it avoids the whole body from getting flooded with drugs.
And what if you’re diabetic? Steroids can spike your blood sugar. But that’s manageable. You check your levels more often for a week. It’s a trade-off - but far safer than a bleeding ulcer from NSAIDs.
Here’s the reality: most gout patients are older. Most have other conditions. That’s why guidelines now say: match the drug to the patient, not the other way around.
Combination Therapy: Sometimes, You Need More Than One
Not every flare responds to just one drug. Some people get partial relief - then the pain creeps back. That’s when doctors reach for combinations.
One common approach: a short course of steroids plus a low dose of colchicine. It’s like using two tools instead of one. The steroid hits inflammation fast. The colchicine helps prevent it from coming back.
Another: NSAID plus colchicine - but only if the patient has no kidney issues and no stomach problems. This combo is powerful, but it’s also risky. It’s not for beginners.
Combination therapy isn’t first-line. But when one drug fails, it’s often the next step. And it works.
Timing Is Everything - Start Within 24 Hours
It doesn’t matter which drug you pick. If you wait too long, none of them work as well.
Studies show: if you start treatment within 24 hours of the first pain, you cut the flare duration in half. Wait 48 hours? You’re looking at a week of misery.
That’s why doctors say: start within 24 seconds of pain onset. It’s not a joke. It’s a rule. The moment you feel that sharp, burning, swollen pain - reach for your medication. Don’t wait to see if it gets worse. Don’t hope it’ll go away. Act.
Keep your prescription handy. Tell your partner where it is. Set a reminder on your phone. This isn’t optional. Timing saves you from months of pain.
What About Long-Term Prevention?
Flare treatment is just half the battle. If you’re on uric acid-lowering drugs like allopurinol or febuxostat, you need to protect yourself from new flares - especially in the first few months.
When your uric acid drops, crystals start shifting. That triggers flares. So even if you’re on a preventive drug, you still need protection.
Guidelines say: take NSAIDs, colchicine, or low-dose steroids for at least three months after your uric acid hits target. If you’ve had tophi (those lumpy deposits under the skin), go six months.
Skipping this step is why so many people get repeated flares. You’re treating the symptom - not the cause. And the cause is still active.
Bottom Line: No One-Size-Fits-All
There’s no magic bullet for gout. No single drug that’s best for everyone. NSAIDs, colchicine, and steroids all work - but they’re not interchangeable.
Choose based on your body. Your kidneys. Your stomach. Your heart. Your other meds. Your lifestyle.
And never delay. Start treatment the moment you feel it. That’s the real game-changer.




Josh McEvoy
January 22, 2026 AT 18:08Tiffany Wagner
January 24, 2026 AT 04:59Viola Li
January 25, 2026 AT 08:57Jenna Allison
January 26, 2026 AT 09:18Vatsal Patel
January 28, 2026 AT 04:28Helen Leite
January 29, 2026 AT 12:37Sharon Biggins
January 30, 2026 AT 12:17Himanshu Singh
January 31, 2026 AT 16:14Jamie Hooper
January 31, 2026 AT 23:29Husain Atther
February 2, 2026 AT 19:11Elizabeth Cannon
February 4, 2026 AT 10:46Marlon Mentolaroc
February 4, 2026 AT 12:17Phil Maxwell
February 4, 2026 AT 14:38Karen Conlin
February 6, 2026 AT 02:13asa MNG
February 7, 2026 AT 10:35