When your shoulder starts to hurt and won’t move-no matter how hard you try-it’s not just a bad day. It could be frozen shoulder, also known as adhesive capsulitis. This isn’t a simple muscle strain. It’s a slow, painful stiffening of the shoulder joint capsule, the tissue that wraps around the ball-and-socket joint. You can’t reach behind your back, lift your arm overhead, or even sleep on that side without waking up in pain. And here’s the worst part: it doesn’t just go away on its own in a few weeks. Left untreated, it can last two years or more.
What Exactly Is Adhesive Capsulitis?
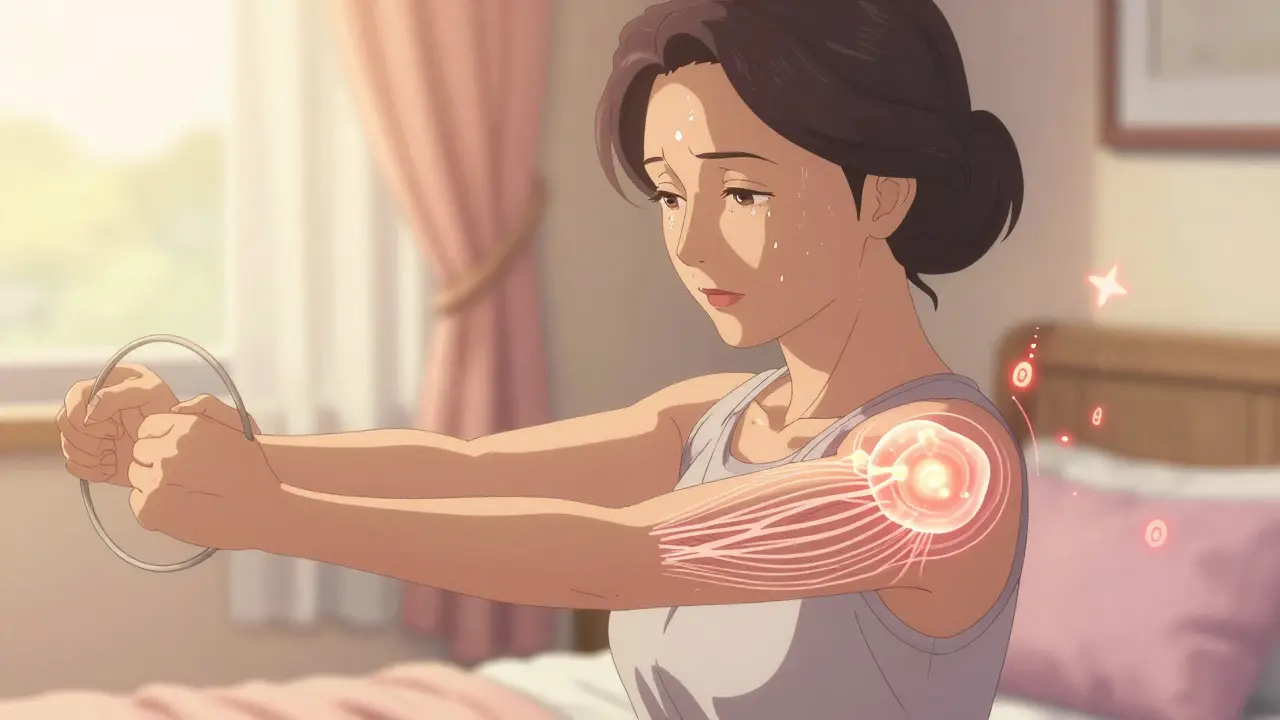
Adhesive capsulitis doesn’t mean your shoulder is glued shut. That’s a myth. The real problem is thickening and tightening of the joint capsule. Normally, this capsule holds about 30-35 milliliters of fluid and allows smooth, full motion. In frozen shoulder, it shrinks to 10-15 mL. The lining becomes inflamed, then scarred. This isn’t caused by a fall or a sports injury. It creeps up slowly-often without warning.
People with diabetes are at much higher risk. Up to 20% of those with diabetes develop frozen shoulder, compared to just 2-5% of the general population. Other risk factors include thyroid disorders, heart disease, and long periods of shoulder immobility after surgery or injury. It’s more common in women between 40 and 60 years old.
The key sign? Both active and passive movement are limited. If you can’t lift your arm yourself, and your doctor can’t lift it for you either-that’s frozen shoulder. In contrast, a torn rotator cuff lets you move the shoulder passively, even if it hurts. That’s a major clue doctors use to tell them apart.
The Three Stages of Frozen Shoulder
This condition doesn’t happen overnight. It follows a clear, predictable timeline:
- Freezing stage (6 weeks to 9 months): Pain gets worse over time, especially at night. Movement becomes harder. You might start avoiding reaching for things because it hurts too much.
- Frozen stage (4 to 6 months): The pain may ease up a bit, but stiffness takes over. Your shoulder feels locked. You can’t reach behind your head, tuck in your shirt, or brush your hair. This is when people often say, “I can’t move it at all.”
- Thawing stage (6 months to 2 years): Slowly, motion returns. But without treatment, this can take over two years. With the right mobilization, it can shrink to six months.
Most people don’t realize they’re in the freezing stage until it’s too late. By then, the capsule has already started tightening. The earlier you start movement, the better your odds.
Why Mobilization Works-And Why Force Doesn’t
For years, the advice was simple: rest and wait. But research has turned that idea upside down. A 2019 review in American Family Physician showed that patients who began gentle movement during the freezing phase recovered in 6-12 months instead of 2-3 years. The key word? Gentle.
Pushing too hard, too soon, makes things worse. One patient reported that forced stretching during the freezing stage turned their pain from a 4 out of 10 to an 8 out of 10 for three weeks. That’s not progress-that’s damage.
What works is progressive, pain-controlled movement. Physical therapy supervised by a professional during the freezing phase leads to 28% faster recovery than doing exercises alone at home, according to the American Academy of Orthopaedic Surgeons. The goal isn’t to stretch the capsule to its limit. It’s to keep it from getting tighter.
Effective Mobilization Techniques
You don’t need fancy equipment. Most of these can be done at home with everyday items.
- Pendulum exercises: Lean over, let your arm hang loose, and gently swing it in small circles. Do this for 5 minutes a day. It’s low-risk and helps maintain some motion without stressing the joint.
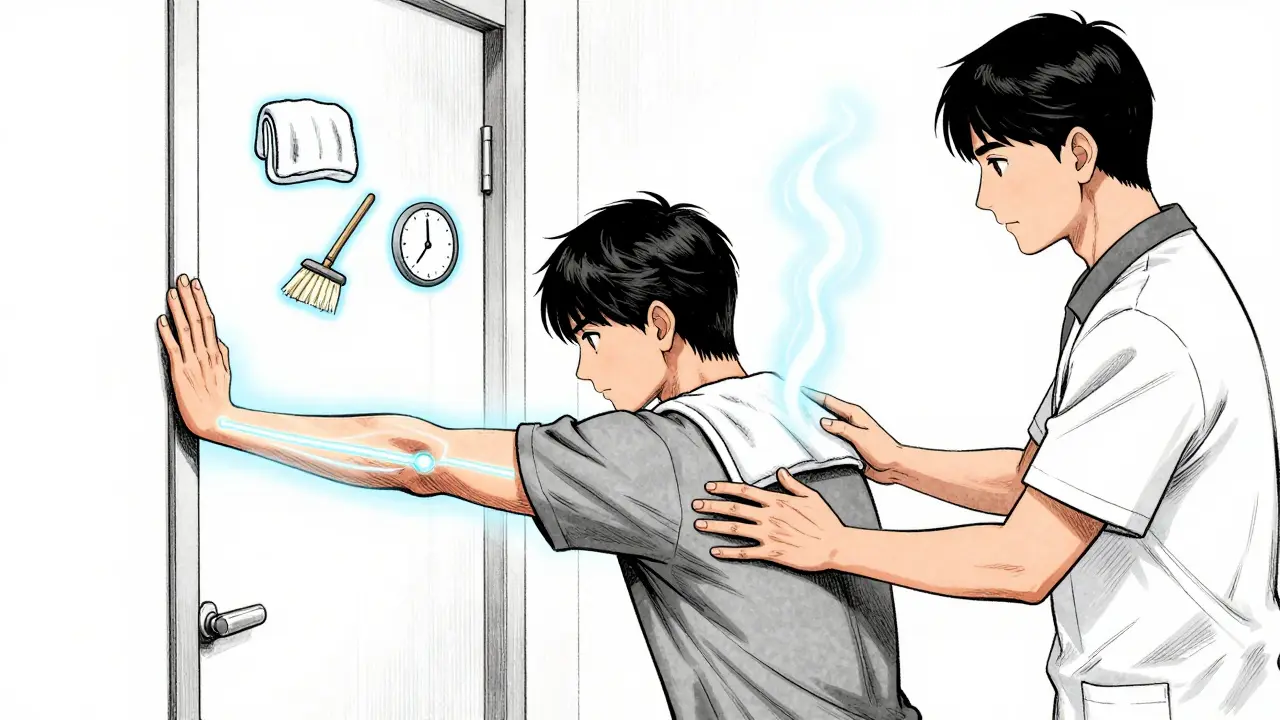
- Towel stretch: Hold one end of a towel in your good hand, drape it behind your back, and grab the other end with your affected hand. Gently pull upward with your good arm to lift the affected arm. This helps with internal rotation.
- Doorway stretch: Stand in a doorway, place your hand on the frame at shoulder height, and gently lean forward. Hold for 30 seconds. This targets external rotation-the most restricted movement.
- Wand exercises: Use a broomstick or yoga strap. Hold it with both hands and slowly lift it overhead, letting your good arm guide the stiff one. Keep movements small and controlled.
Heat helps. Apply a warm towel or heating pad for 10-15 minutes before stretching. It loosens the capsule and reduces pain. Do these exercises daily. Consistency matters more than intensity.
What Doesn’t Work (And Why)
Not all treatments are created equal.
Corticosteroid injections can give short-term pain relief (4-8 weeks), but studies show no lasting benefit in function or range of motion after 12 weeks. They might help you get through the worst of the pain so you can start moving-but they don’t fix the stiffness.
Manipulation under anesthesia sounds like a quick fix: the doctor forces your shoulder into motion while you’re asleep. But the American Academy of Orthopaedic Surgeons says this should only be considered after six months of failed conservative treatment. It carries risks-fractures, torn tendons, nerve damage. Don’t rush into it.
Rest alone is outdated advice. The 2023 update from the American Academy of Family Physicians now recommends moving within pain tolerance during the freezing phase. Waiting for pain to disappear before moving means you’re giving the capsule time to tighten even more.
How to Track Progress
Progress isn’t always obvious. You might not notice you’re lifting your arm 5 degrees higher until you try to reach for a high shelf and realize you can do it without wincing.
Keep a simple log: write down your range of motion each week. Use a ruler to measure how far you can reach behind your back. Or use a smartphone app like ShoulderROM, which got FDA clearance in 2023 and gives real-time feedback on movement. In clinical trials, users using this device recovered 32% faster than those relying on standard exercises.
Also track pain levels on a scale of 1-10. If your pain spikes after stretching and lasts more than 2 hours, you’re pushing too hard. Back off. Recovery isn’t a race.

Sleep and Daily Living Tips
Seven out of ten patients say nighttime pain is their biggest struggle. Here’s what helps:
- Sleep on your back with a pillow under the affected arm to keep it slightly elevated.
- If you sleep on your side, hug a pillow to your chest to prevent the shoulder from rolling inward.
- Wear loose-fitting shirts with buttons or zippers in the front. Avoid pullovers.
- Use a long-handled brush or dressing aid for hair and hygiene tasks.
These small adjustments reduce strain and help you stay consistent with your exercises-even when you’re tired.
When to See a Specialist
Most cases improve with physical therapy and time. But red flags mean you need more than mobilization:
- Fever, night sweats, or unexplained weight loss (could signal infection or cancer)
- Sudden weakness or numbness in the arm (could be nerve-related)
- History of trauma or recent surgery
- No improvement after 6 months of consistent therapy
If you’ve tried everything and your shoulder still won’t move, an orthopedic specialist might consider arthroscopic capsular release-a minimally invasive surgery to cut the tightened tissue. But this is needed in only about 13% of cases, according to a 2023 Cochrane Review.
What the Future Holds
Research is moving toward personalized rehab. Scientists at the NIH are studying IL-6, a protein linked to inflammation, to predict who will respond best to stretching vs. injections. In the next five years, we may see blood tests guiding treatment plans.
Telehealth physical therapy is already growing. Over 40% of large U.S. employers now cover virtual shoulder rehab programs. That means you can get expert guidance from home-no commute, no wait.
The bottom line? Frozen shoulder isn’t a life sentence. It’s a slow process-but one you can speed up. Start early. Move gently. Stay consistent. And don’t wait for the pain to go away before you start healing.




Aliza Efraimov
December 29, 2025 AT 04:53Oh my GOD, I thought I was going crazy when I couldn’t reach my back zipper for months. My PT said it was ‘just aging’-until I found this post. I’m in stage two right now, and the towel stretch? LIFE CHANGER. I cried the first time I touched my opposite shoulder. Please, if you’re reading this and stuck-don’t give up. It gets better.
Manan Pandya
December 29, 2025 AT 16:08Well-articulated and clinically accurate. The distinction between active and passive range of motion as a diagnostic differentiator is often overlooked by primary care providers. I’d add that proprioceptive neuromuscular facilitation (PNF) techniques, particularly contract-relax for external rotation, show promising outcomes in phase two when combined with low-load sustained stretching. Consistency over intensity remains the cornerstone.
Emma Duquemin
December 31, 2025 AT 10:41THIS. This is the post I needed three years ago when I was sobbing in my pajamas trying to put on a shirt. I did the pendulum thing while waiting for my coffee to brew-five minutes a day-and now I can reach the top shelf again. No magic. Just tiny, stubborn movements. You don’t need a gym. You just need to not quit.
Henriette Barrows
January 1, 2026 AT 19:57I’m so glad someone finally said it: rest doesn’t help. I waited six months because I was scared to hurt myself more. Big mistake. The second I started the doorway stretch-even just 10 seconds a day-I felt like I was getting my life back. You’re not weak for needing help. You’re brave for trying.
Alex Ronald
January 2, 2026 AT 11:21For anyone using ShoulderROM: I’ve been tracking my progress for 11 weeks. My external rotation improved from 22° to 78°. The app’s feedback on movement smoothness was way more useful than just measuring degrees. Also, heat before stretching? Non-negotiable. Warm towel + 10 minutes = game over for stiffness.
Tamar Dunlop
January 3, 2026 AT 00:07While the clinical insights presented are commendable, one must not overlook the socio-cultural dimensions of chronic pain management. In many Western societies, the emphasis on individual resilience and self-driven rehabilitation may inadvertently exacerbate psychological distress among patients who lack socioeconomic support structures. Access to consistent physical therapy remains a privilege, not a right.
Teresa Rodriguez leon
January 4, 2026 AT 09:00Everyone’s so obsessed with stretching. But what about the fact that 70% of people who get this have diabetes? Nobody talks about managing blood sugar to reduce inflammation. You can stretch all day, but if your HbA1c is 8.5, you’re fighting a losing battle.
Paige Shipe
January 4, 2026 AT 12:17Ummmm so… did you even read the study you cited? The Cochrane review said ‘insufficient evidence’ for most of these techniques. And ‘ShoulderROM’? That’s a $9.99 app made by a guy in Ohio. You’re all just repeating TikTok advice.
Jim Rice
January 4, 2026 AT 14:06Everyone’s acting like this is some new discovery. I had this in 2015. The only thing that worked was manipulation under anesthesia. All this ‘gentle stretching’ nonsense just delays the inevitable. You’re wasting 2 years when you could’ve had it fixed in 15 minutes under sedation.
David Chase
January 5, 2026 AT 00:47OMG I CAN’T BELIEVE YOU GUYS ARE STILL TALKING ABOUT THIS 😭😭😭 I had frozen shoulder and I did EVERYTHING-PT, injections, yoga, cryotherapy, even a crystal healer (no joke). The ONLY thing that worked? I started lifting weights again. Heavy. Like, 50lb dumbbells. Pain is just weakness leaving the body. 💪🔥🔥🔥
Nisha Marwaha
January 6, 2026 AT 03:08From a biomechanical standpoint, the fibroblast-mediated collagen remodeling phase during the thawing stage is critically modulated by mechanical loading thresholds. The described mobilization protocols align with the mechanotransduction principles outlined in the 2022 JOSPT guidelines, particularly in the context of TGF-β1 downregulation. However, adherence metrics remain suboptimal in outpatient populations due to lack of real-time biofeedback integration. Consider augmenting with wearable inertial measurement units for quantifiable progression.