Every year in the U.S., over 1.3 million medication errors happen in hospitals and pharmacies. Most of them aren’t caused by careless staff-they’re caused by human fatigue, rushed workflows, and simple misreads. One wrong digit in a dosage, one mislabeled bottle, one patient confused with another-and the consequences can be deadly. But there’s a tool that’s quietly stopping thousands of these mistakes before they happen: barcode scanning.
How Barcode Scanning Stops Errors Before They Start
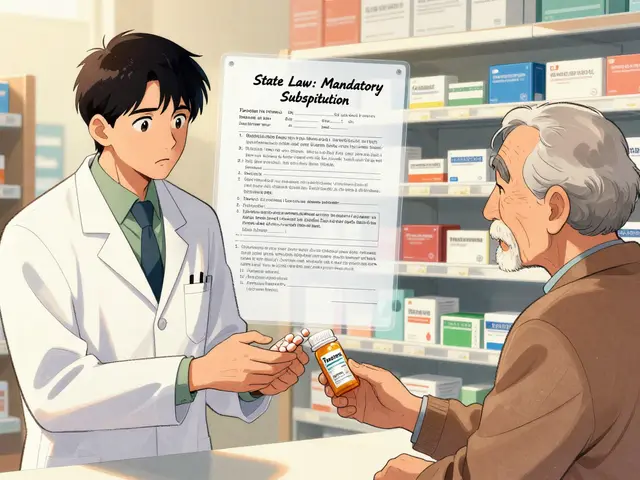
Barcode scanning in pharmacies isn’t just a tech upgrade. It’s a safety checkpoint built into the workflow. Here’s how it works: when a pharmacist pulls a medication, they scan the barcode on the pill bottle or vial. At the same time, they scan the patient’s wristband. The system instantly checks: Is this the right drug? Is this the right dose? Is it for the right patient? Is it the right time and route? If anything doesn’t match, the system stops everything. It won’t let the medication leave the counter. That’s not a suggestion-it’s a hard block. In one Pennsylvania hospital, before barcode scanning, pharmacists correctly dispensed meds about 86.5% of the time. After implementation? That number jumped to 97%. That’s not a small gain. That’s a life-saving shift. This isn’t magic. It’s the Five Rights: right patient, right medication, right dose, right route, right time. Barcode scanning verifies all five automatically. Manual double-checks? They catch only about 36% of errors. Scanning catches 93.4%. That’s not even close.What Barcodes Actually Contain
Not all barcodes are the same. Most pharmacy barcodes are 1D linear codes-those long black-and-white stripes you’ve seen on groceries. But they’re not just any barcode. They’re encoded with the National Drug Code (NDC), a unique 11-digit number assigned by the FDA to every prescription and over-the-counter drug. This code tells the system exactly what drug it is, who makes it, and the strength and package size. Newer systems are moving to 2D matrix barcodes (like QR codes). These can hold more data: lot numbers, expiration dates, even batch info. That’s huge for tracking recalls or identifying contaminated meds. The FDA started requiring NDC barcodes on all unit-dose packages back in 2006. Since then, every new medication sold in the U.S. has to have one. But here’s the catch: barcodes aren’t foolproof. If the label is smudged, torn, or printed poorly, the scanner can’t read it. That’s why scanning isn’t the only step-it’s part of a layered system. Pharmacists are still trained to visually check the medication against the prescription when a barcode fails. The system doesn’t replace judgment-it supports it.Why Manual Checks Still Fail
You might think, “Why not just have two pharmacists check every prescription?” It sounds safe. But human brains get tired. In a busy pharmacy, a technician might grab a bottle of levothyroxine instead of levothyroxine sodium. The names look similar. The bottles look similar. The doses are close. Without a scan, the error slips through. A real case from the Pennsylvania Patient Safety Authority: a patient was supposed to get 50 mcg of levothyroxine. The pharmacy accidentally pulled a 500 mcg dose. The label was correct. The barcode was correct. But the actual pill inside the bottle was wrong. The barcode didn’t catch it because the label was misapplied. That’s why experts stress: never scan a label without visually confirming the drug inside matches the order. Manual checks rely on memory, attention, and timing. When it’s 3 p.m. on a Friday, the pharmacy is backed up, and you’ve been on your feet for six hours? Your brain starts skipping steps. Scanning doesn’t get tired. It doesn’t get distracted. It doesn’t assume.
Where Barcode Scanning Falls Short
Barcode scanning works best with standard, factory-packaged meds. That’s where the NDC codes are clear and consistent. But real-life pharmacy work isn’t always neat. Ampules? Insulin pens? Compounded medications? These often don’t come with barcodes-or the barcode is too small, too fragile, or gets damaged during handling. In those cases, pharmacists have to rely on visual checks, which brings us back to human error. One hospital pharmacist in Melbourne told me: “We use special trays with built-in lights for ampules. Still, we lose 15 minutes a day just trying to scan them.” Another issue: workarounds. When the scanner freezes, or the network glitches, staff sometimes just skip the scan. A 2023 survey found 41% of pharmacists admit to bypassing scans during rush hours. That’s dangerous. The system only works if it’s used every time. And then there’s automation bias. That’s when people trust the machine too much. If the scanner beeps “OK,” they don’t look at the drug. They assume it’s right. But if the pharmacy printed the wrong label with the right barcode, the system won’t know. That’s why training isn’t optional-it’s critical. Staff must learn: scan first, then verify visually. Never skip the second step.Technology That’s Making It Better
The field is evolving. In 2024, Epic Systems rolled out mobile barcode scanners that attach to tablets pharmacists carry around. That cut scanning failures by 22%. Why? Because now, instead of walking to a fixed scanner, they can scan right at the counter, in the middle of packing a prescription. The FDA is also testing 2D barcodes that can store even more data-like the patient’s allergies or drug interactions. Imagine scanning a vial and the system instantly shows: “This patient is allergic to sulfa.” That’s not science fiction. It’s coming. AI is on the horizon too. Cerner’s 2025 update will include machine learning that predicts which barcodes are likely to fail based on past data. It’ll flag problematic products before they even hit the shelf. That’s proactive safety. And adoption is rising. In U.S. hospitals, 78% now use barcode scanning. That’s up from 42% in 2015. But community pharmacies? Only 35%. Why? Cost. The hardware, software, training, and integration aren’t cheap. A small independent pharmacy might spend $20,000 just to get started. But when you consider that one dispensing error can cost over $100,000 in lawsuits and lost trust? The ROI isn’t even close.
What You Can Do as a Patient
You’re not just a bystander in this system. You can be part of the safety net. When you pick up your prescription, ask: “Was this scanned?” If the pharmacist says yes, good. If they say no, ask why. If they shrug, speak up. You have the right to know your meds were checked. Also, keep your own list of meds. If you’re on levothyroxine, know the dose. If you’ve had a reaction to a drug before, tell the pharmacist every time-even if they’ve seen you before. Technology helps, but human communication saves lives.The Bigger Picture
Barcode scanning isn’t the end of medication safety. It’s a powerful tool in a much larger system. Computerized prescribing, automated dispensing cabinets, smart IV pumps-all of these work together. But without barcode scanning, the chain breaks. The Institute for Safe Medication Practices calls it a “Tier 1” safety practice-meaning it’s one of the most effective tools we have. The ECRI Institute ranks it third overall for preventing errors, behind only computerized prescribing and automated cabinets. It’s not perfect. It’s not magic. But it’s the closest thing we have to a safety net that actually catches mistakes before they reach you.Frequently Asked Questions
Do all pharmacies use barcode scanning?
No. Most hospitals in the U.S. use barcode scanning-about 78% as of 2023. But in community pharmacies, adoption is much lower, around 35%. The main reason is cost. Small independent pharmacies often can’t afford the hardware, software, and training needed. However, as regulations tighten and insurance providers push for safety standards, more community pharmacies are starting to adopt it.
Can barcode scanning prevent all medication errors?
No. Barcode scanning prevents errors caused by mismatched labels, wrong drugs, wrong doses, or wrong patients-but not all errors. It can’t catch a miswritten prescription, a miscommunication between doctors, or a medication that was compounded incorrectly with the wrong ingredients. It also can’t detect if a pill looks wrong (like a white tablet instead of a blue one) if the barcode is correct. That’s why visual verification by a pharmacist is still required, even after scanning.
What happens if a barcode doesn’t scan?
The system should stop the process and alert the pharmacist. At that point, the pharmacist must visually verify the medication against the original prescription. They check the drug name, strength, manufacturer, and physical appearance. Never just re-scan or override the system without checking. If the barcode is damaged or missing, the pharmacy should report it to the manufacturer and the Institute for Safe Medication Practices (ISMP). Many hospitals now have barcode validation teams that test new products before they’re stocked.
Is barcode scanning slower than manual dispensing?
Initially, yes. Staff need training, and scanners can glitch. Some pharmacists report adding 15-20 minutes per shift due to scanning failures. But over time, efficiency improves. Studies show barcode systems reduce overall dispensing time by 12% because they cut down on corrections, returns, and error investigations. The time spent scanning is far less than the time spent fixing a wrong medication that got to a patient.
Are there any risks to using barcode scanning?
Yes. The biggest risk is automation bias-when staff trust the scanner too much and skip visual checks. Another risk is workarounds: skipping scans during busy times. Both lead to errors. Also, if the barcode is printed incorrectly on the label (even if the drug inside is right), the system will approve it. That’s why pharmacies must verify the physical medication matches the label every time. Regular audits and staff training are essential to prevent these risks.





Keasha Trawick
December 13, 2025 AT 00:37Okay but let’s be real-barcodes are the only thing standing between me and a lethal dose of levothyroxine sodium instead of plain levothyroxine. I’ve seen the bottles. They look identical. The only thing that stops me from becoming a human case study is that little black-and-white stripe. It’s not sexy, it’s not glamorous, but it’s the unsung hero of my survival. 🙌
Bruno Janssen
December 13, 2025 AT 21:15...I just read this. I’m quiet now.
Deborah Andrich
December 15, 2025 AT 11:04My aunt almost died because a tech grabbed the wrong bottle. She’s fine now but she won’t take anything without watching them scan it. I used to think she was paranoid. Now I get it. We all need that second set of eyes-even if it’s a machine. Don’t shame the tech. Use it. And if your pharmacy doesn’t scan? Ask why. Loudly.
Tommy Watson
December 17, 2025 AT 00:28barcods r just a scam to make pharms look good. i mean who even reads these things? i got my meds and im alive so who cares?? 🤷♂️
Sheldon Bird
December 17, 2025 AT 01:03You’re all right but let’s not forget the humans behind the scanners. I’ve seen pharmacists work 12-hour shifts with no break, scanning 300+ scripts a day. They’re not robots. They’re tired. The system helps-but it doesn’t replace compassion. A little ‘are you sure this is right?’ from a patient? That’s gold. ❤️
Karen Mccullouch
December 17, 2025 AT 02:33USA is the only country that gives a damn about this stuff. In Europe? They just hand you pills like candy. No scans, no checks. We’re lucky. Stop complaining about the 15 extra seconds. It’s saving lives. 🇺🇸💪
nithin Kuntumadugu
December 18, 2025 AT 20:58barcodes? lol. theyre tracking us. the fda and big pharma are putting chips in your pills through the barcode. next thing you know, your meds will activate a gps tracker in your body. they want to know if you took your antidepressants. they want to control your mind. 🤖💊 #mindcontrol
sharon soila
December 20, 2025 AT 19:55Every life matters. Every pill matters. Every scan matters. We must never stop fighting for systems that protect the vulnerable. Even if it takes one extra minute. Even if it costs money. Even if it’s inconvenient. This isn’t about efficiency. It’s about dignity.
Constantine Vigderman
December 22, 2025 AT 03:46Love this! Just got my meds scanned yesterday and honestly? Felt safer. Like my pharmacist was my superhero with a barcode gun 💪😄. Also, side note: if your scanner glitches, don’t just skip it-tell them. They need to know. We’re all in this together! 🙏
Cole Newman
December 23, 2025 AT 03:43you guys are overthinking this. if you’re worried about your meds, just take a picture of the bottle and google it. done. barcode scanning is just corporate theater. they want you to feel safe so you don’t ask questions about the $400 pill you got.
kevin moranga
December 23, 2025 AT 07:01I’ve worked in a pharmacy for 18 years. Before barcodes? We’d have 3-4 errors a week. After? One every three months. It’s not perfect. Yeah, sometimes the label’s smudged. Yeah, sometimes the scanner freezes. But when you’ve seen a kid get the wrong dose because someone misread ‘500mcg’ as ‘50mcg’? You don’t skip the scan. You don’t make excuses. You scan. You check. You breathe. And you thank the machine for doing the boring part so you can do the human part. That’s the balance. And it works.
Alvin Montanez
December 23, 2025 AT 22:34People think technology fixes everything. It doesn’t. It just hides the real problem: pharmacies are understaffed, underpaid, and overworked. Barcodes don’t fix burnout. They just make it look like you’re doing your job while your soul is evaporating. And now we’re supposed to be grateful because the machine didn’t let you kill someone? That’s not progress. That’s a Band-Aid on a hemorrhage.
Lara Tobin
December 25, 2025 AT 20:01My dad passed away because of a wrong med. I don’t talk about it much. But when I see someone scanning their prescription? I smile. I don’t say anything. I just smile. Because maybe, just maybe, someone else won’t have to lose their person too. 🫂