The U.S. healthcare system runs on generics. About 9 out of 10 prescriptions filled in America are for generic drugs. That’s not luck. It’s the result of a carefully designed legal and scientific process built over 40 years - one that lets safe, affordable medicines reach millions without repeating the billion-dollar trials of brand-name drugs. This system didn’t happen by accident. It was written into law in 1984, and it’s still working today - even as drug complexity grows.
The Hatch-Waxman Act: The Legal Backbone
The foundation of today’s generic drug approval system is the Drug Price Competition and Patent Term Restoration Act of 1984 - better known as the Hatch-Waxman Act. This law, passed on September 24, 1984, created a new path for generic manufacturers to bring drugs to market without starting from scratch. Before Hatch-Waxman, generic companies had to run full clinical trials just to prove their version of a drug worked. That was expensive, slow, and often impossible for smaller firms. The law changed that by letting them rely on the FDA’s prior approval of the original brand drug.The key innovation? The Abbreviated New Drug Application, or ANDA. This isn’t a shortcut. It’s a smart one. Generic companies don’t need to prove the drug works again. They just need to prove their version is the same in every way that matters - active ingredient, strength, dosage form, route of administration, and most importantly, how the body absorbs it. The FDA doesn’t lower its standards. It just avoids redundant work.
What the FDA Actually Requires
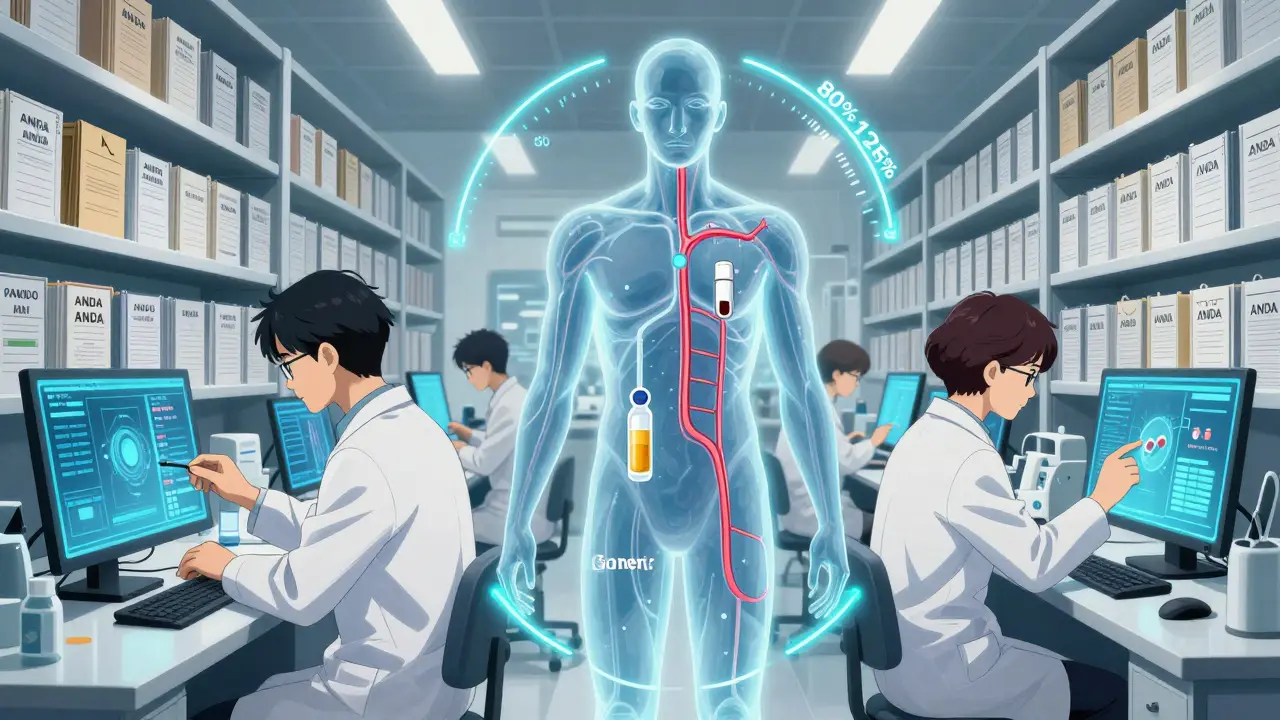
Getting FDA approval for a generic isn’t like copying a recipe. It’s more like reverse-engineering a machine to match its exact output. The FDA demands that a generic drug:- Contains the same active ingredient(s) as the brand-name drug
- Is identical in strength, dosage form, and how it’s taken (pill, injection, inhaler, etc.)
- Has the same medical uses and labeling
- Is bioequivalent - meaning it delivers the same amount of medicine into the bloodstream at the same rate
- Meets the same strict quality standards for identity, purity, and strength
- Is made in a facility that passes the same inspections as the brand’s factory
The bioequivalence requirement is where the rubber meets the road. For most drugs, this means testing in 24 to 36 healthy volunteers. Scientists measure how quickly and how much of the drug enters the blood. The generic’s results must fall within 80% to 125% of the brand’s. That’s not a wide range - it’s a tight window. If a generic falls outside that, it’s rejected. No exceptions.
The ANDA Submission: What’s Inside the Package
A complete ANDA isn’t just a few pages. It’s a thick dossier. Manufacturers must include:- Full Chemistry, Manufacturing, and Controls (CMC) data - every step of how the drug is made, tested, and packaged
- Details on all manufacturing, packaging, and testing sites - including foreign facilities
- Proposed labeling that matches the brand drug exactly
- Proof of bioequivalence from clinical studies
- Patent certifications - which can trigger legal delays
The FDA’s Division of Filing Review checks the application first. If anything’s missing - say, a missing stability study or unclear manufacturing map - they issue a Refuse-to-Receive letter. No review happens. No fee is refunded. You have to fix it and resubmit. That’s why experienced generic companies hire teams of regulatory specialists. One mistake can cost months.
Patents, Exclusivity, and the 30-Month Stay
Here’s where things get messy. The Hatch-Waxman Act lets generic companies challenge brand patents. If they file a Paragraph IV certification - claiming a patent is invalid or won’t be infringed - the brand company has 45 days to sue. If they do, the FDA can’t approve the generic for 30 months. That’s not a review delay. That’s a legal hold.This has led to what some call “patent thickets” - brands stacking multiple patents on minor changes to block generics. The FDA’s Drug Competition Action Plan tries to cut through this. But it’s still a major bottleneck. In 2023, over 40% of first-time generic approvals were delayed by litigation.
There’s also exclusivity. If a brand company is the first to prove a drug works for a new use, they get 3 years of market protection. If they’re the first to file an ANDA for a drug with no prior generic, they get 180 days of exclusive rights - a huge financial incentive. That’s why companies race to be first.
Review Timelines and GDUFA
Before 2012, FDA review times were unpredictable. Sometimes it took years. The Generic Drug User Fee Amendments (GDUFA) changed that. Under GDUFA III, which runs through 2027, the FDA commits to:- Reviewing standard ANDAs within 10 months
- Reviewing priority ANDAs - like those for drugs in shortage or first generics - within 8 months
These aren’t suggestions. They’re binding performance goals. If the FDA misses them, they pay the company back. That’s a powerful incentive. In 2023, the FDA approved 90 first-time generic drugs. That’s up from 79 in 2022. First-cycle approval rates have climbed to over 60%, meaning most applications get approved on the first try - a huge improvement from a decade ago.
Complex Generics: The New Frontier
Not all drugs are easy to copy. Inhalers, topical creams, injectable suspensions, and extended-release pills are harder. Why? Because how the drug behaves in the body isn’t just about blood levels. It’s about how it’s released, absorbed, or delivered. For these, bioequivalence studies aren’t enough. The FDA now requires additional data - like in vitro testing, imaging studies, or even patient outcomes.The FDA’s Complex Generic Drug Product Development Resources initiative helps manufacturers navigate this. But it’s still a challenge. In 2023, only 12% of approved ANDAs were for complex products. The agency admits it’s playing catch-up. That’s why they launched a new pilot program in October 2025: faster reviews for companies that test and manufacture their generics in the U.S. It’s a direct push to rebuild domestic supply chains.

Why This Matters to Patients
The impact is real. Generic drugs cost, on average, 80% to 85% less than brand-name versions. That’s not a small savings. It’s life-changing for people on insulin, blood pressure meds, or antidepressants. In 2023, the FDA approved the first generic version of Vivitrol - a long-acting injectable for opioid addiction. The agency called it “of prime importance” given the ongoing overdose crisis.When a brand drug loses exclusivity, prices often drop by 50% within months. When multiple generics enter, prices can plunge further. That’s competition. That’s the system working. The FDA doesn’t just approve drugs. It helps keep healthcare affordable.
Who’s Making These Drugs?
The market is dominated by a few big players: Teva, Sandoz, Viatris (which merged Mylan and Upjohn), and Amneal. But hundreds of smaller companies are pushing into complex generics. Many are based outside the U.S., but the FDA is pushing for more domestic production. The new pilot program rewards U.S.-based manufacturing with faster reviews. That’s a shift - and it’s already changing where companies build factories.What’s Next?
The future isn’t just about more generics. It’s about smarter ones. The FDA is working on better tools to evaluate complex products. Biosimilars - generic versions of biologic drugs like Humira - are growing fast, but they follow a different law (BPCIA) and are more expensive to develop. For now, small-molecule generics remain the backbone of affordability.The system isn’t perfect. Patent games still delay access. Complex drugs still take too long. But the core framework - Hatch-Waxman plus GDUFA - has delivered over 10,000 generic approvals since 1984. It’s saved U.S. patients over $3 trillion in drug costs. That’s not just policy. That’s public health.
How long does it take for the FDA to approve a generic drug?
Under current rules, the FDA aims to review a standard generic drug application (ANDA) within 10 months. For priority applications - like those for drugs in short supply or first-time generics - the goal is 8 months. These timelines are part of the Generic Drug User Fee Amendments (GDUFA), which set binding performance goals. Before GDUFA, reviews could take years. Now, over 60% of applications are approved on the first try.
Are generic drugs really as safe and effective as brand-name drugs?
Yes. The FDA requires that generic drugs meet the same strict standards as brand-name drugs for active ingredients, strength, dosage form, and quality. They must also be bioequivalent - meaning they deliver the same amount of medicine into the bloodstream at the same rate. The FDA tests batches from both brand and generic drugs to ensure consistency. Millions of patients use generics every day with the same results as the brand versions.
Why do some generic drugs cost more than others?
Price differences come down to competition. If only one or two companies make a generic, prices stay higher. When five or more manufacturers enter the market, prices often drop dramatically - sometimes by over 90%. Complex generics, like inhalers or injectables, cost more to make and have fewer competitors, so they’re pricier. Also, generics made in the U.S. may cost more than those imported, but new FDA incentives are encouraging domestic production.
Can a generic drug be approved even if the brand-name drug has patents?
Yes, but with conditions. Generic manufacturers can challenge brand patents by filing a Paragraph IV certification. If the brand company sues for infringement, the FDA can’t approve the generic for up to 30 months - a legal delay known as a 30-month stay. This gives the brand time to defend its patent. If the court rules the patent is invalid or not infringed, approval can proceed. Many generics are approved after litigation ends.
What’s the difference between a generic and a biosimilar?
Generics are copies of small-molecule drugs - like pills made from chemical compounds. Biosimilars are copies of large, complex biologic drugs - like injectables made from living cells, such as insulin or rheumatoid arthritis treatments. Biosimilars require more testing than generics because they’re harder to replicate exactly. They follow a different approval pathway under the Biologics Price Competition and Innovation Act (BPCIA), not the Hatch-Waxman Act. Biosimilars are more expensive to develop and less common than traditional generics.





caroline hernandez
February 5, 2026 AT 06:38The Hatch-Waxman Act is the unsung hero of American pharmacoeconomics. ANDA submissions don't cut corners-they optimize rigor. Bioequivalence isn't a suggestion; it's a pharmacokinetic tightrope walk between 80-125% AUC and Cmax thresholds. The FDA's CMC requirements for API synthesis, polymorph control, and excipient compatibility are more granular than most academic theses. GDUFA’s binding timelines transformed what was once a regulatory black hole into a predictable pipeline. This isn’t luck. It’s engineered access.
Jhoantan Moreira
February 7, 2026 AT 05:55This is actually one of the most impressive public health success stories no one talks about 🙌 90% of prescriptions filled = generics. 85% cheaper. Millions of people on insulin, statins, antidepressants-living better because of this system. The FDA didn’t lower standards. They just stopped wasting billions on repeat trials. Respect.
Shelby Price
February 8, 2026 AT 08:47So if a generic passes bioequivalence, it's literally the same drug? Even the fillers and coatings? I always thought they were just 'close enough'-but this makes me rethink that. Interesting.
Sherman Lee
February 10, 2026 AT 03:34They say it’s safe but have you seen the factory inspections? Half these generics come from plants in India and China where the FDA shows up once every 5 years. And the bioequivalence studies? 24 healthy volunteers? That’s not medicine-that’s a lab experiment with no real-world patients. You think your blood pressure med is safe? You’re just lucky.
Lorena Druetta
February 10, 2026 AT 19:04It is with profound gratitude that I acknowledge the rigorous scientific integrity underpinning the generic drug approval framework. The commitment to patient safety, coupled with fiscal responsibility, represents a pinnacle of public policy achievement. This system enables dignity in healthcare access for countless individuals who might otherwise forgo essential therapeutics.
Nathan King
February 12, 2026 AT 14:05One must wonder whether the commodification of pharmaceuticals through this framework has inadvertently eroded innovation incentives. The efficiency of ANDA submissions is undeniable, yet the reductionist approach to bioequivalence ignores pharmacodynamic variability in heterogeneous populations. One cannot reduce human physiology to AUC curves and Cmax tolerances.
Harriot Rockey
February 12, 2026 AT 17:35Can we just take a moment to appreciate how brilliant this system is? 💪 People think generics are 'cheap'-but they’re not. They’re smart. They’re efficient. They’re the reason someone on Social Security can afford their heart meds. And now the FDA’s pushing for U.S.-made generics? YES. Let’s build this here. 👏
rahulkumar maurya
February 13, 2026 AT 05:31Let me be clear: the entire system is a facade. The FDA approves generics based on data provided by corporations who hire consultants to game the bioequivalence protocols. The 80-125% window? That’s a loophole disguised as science. And the 30-month stays? Pure corporate collusion. You think this is about patient access? It’s about market control.
pradnya paramita
February 14, 2026 AT 20:23For complex generics-especially extended-release formulations-the ANDA requires not just PK studies but also in vitro dissolution profiling across multiple pH conditions, and sometimes even in vivo-in vitro correlation (IVIVC) modeling. The FDA’s Complex Generic Program mandates additional analytical characterization: particle size distribution, rheological properties, crystallinity index. Most applicants don’t even know where to start. That’s why only 12% of approvals are for complex products. It’s not lack of demand-it’s lack of technical capacity.
Jamillah Rodriguez
February 15, 2026 AT 18:28So basically, the government let Big Pharma write the rules so they could stretch patents forever and then pretend they’re helping people with generics? 🙄 I’m just waiting for the day someone admits this whole thing is a rigged game.
Wendy Lamb
February 17, 2026 AT 15:55Generics save lives. Period.
Antwonette Robinson
February 17, 2026 AT 19:31Oh wow, the FDA 'aims' to review in 10 months? How noble. I’m sure that’s why the backlog is still 8 months long. And 'first-cycle approval rates up to 60%'? That means 40% of applicants got rejected on the first try-after spending millions. This isn’t efficiency. It’s bureaucratic theater with a side of PR.