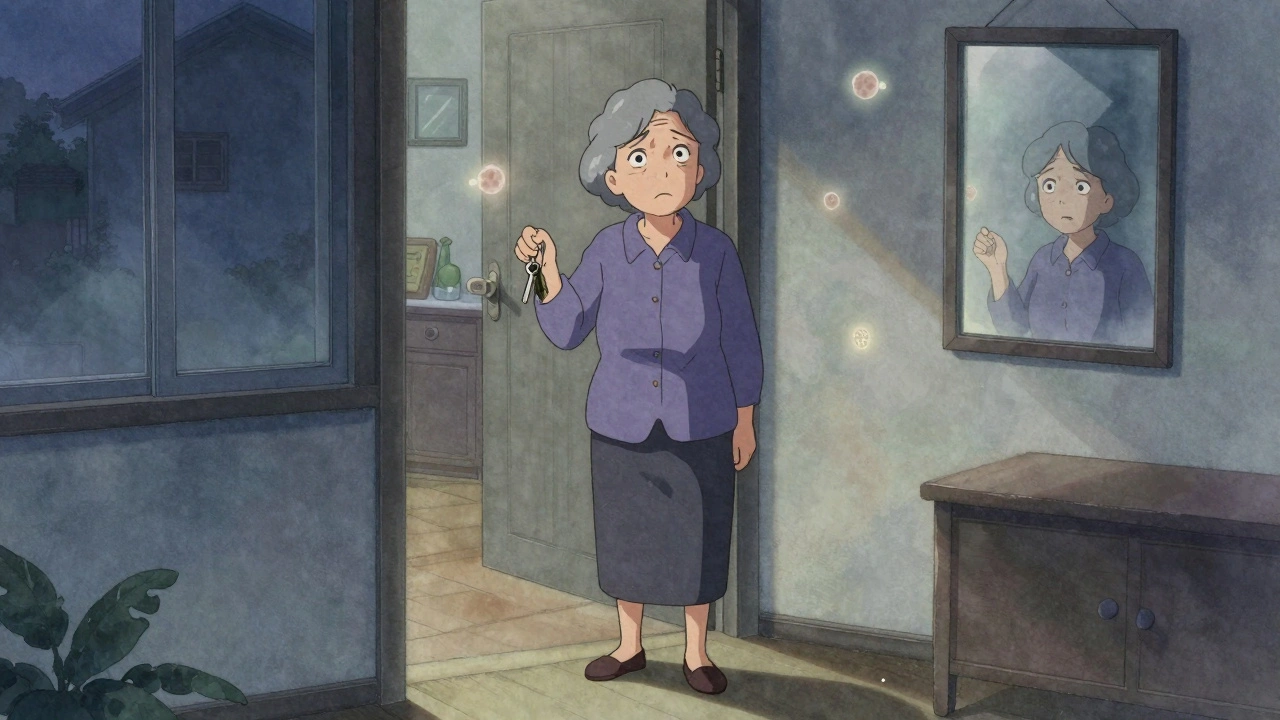
Alzheimer’s disease doesn’t start with confusion. It starts with forgetting where you put your keys-again. Or walking into a room and not remembering why. For many, these moments are dismissed as normal aging. But when they keep happening, when names vanish mid-sentence, when familiar streets feel strange, it’s not just forgetfulness. It’s the early signal of a brain slowly losing its grip.
What Happens in the Brain?
Alzheimer’s isn’t just memory loss. It’s a physical breakdown in the brain. Two abnormal proteins build up: amyloid-beta forms sticky plaques between nerve cells, and tau twists into tangles inside them. These gunk piles block communication between neurons, starve them of nutrients, and eventually kill them. The hippocampus-the brain’s memory center-is hit first. That’s why forgetting recent conversations or appointments is the earliest red flag. Over time, the damage spreads, swallowing areas responsible for language, reasoning, and even basic movement.By the time symptoms show up, the brain has been changing for 15 to 20 years. That’s why scientists now talk about Alzheimer’s as a biological process, not just a set of symptoms. Blood tests are coming that can detect these proteins years before memory problems appear. But right now, diagnosis still relies on tracking how someone thinks, remembers, and behaves over time.
The Five Stages of Alzheimer’s
Alzheimer’s doesn’t jump from sharp to silent. It creeps. Most experts break it into five stages, though not everyone fits neatly into them. Progression varies. One person may decline fast. Another might live 20 years after diagnosis. What stays consistent is the pattern of loss.Stage 1: Preclinical - No symptoms yet. But brain scans or blood tests show amyloid buildup. This stage can last a decade or more. People feel fine. They drive, work, remember birthdays. But inside, the damage is quietly spreading.
Stage 2: Mild Cognitive Impairment (MCI) - This is where families start noticing. The person forgets recent events, repeats questions, misplaces things often, or struggles to find the right word. They might get lost driving to a familiar store. They know something’s off, but they can still manage bills, cook meals, and get dressed. Many are diagnosed here. Not everyone with MCI develops Alzheimer’s-but most who do, show these early signs.
Stage 3: Mild Dementia - Memory loss becomes obvious. They forget personal history: their address, their children’s phone numbers. They can’t plan or organize. Simple tasks like paying bills or using a microwave become confusing. Mood changes kick in-irritability, anxiety, depression. They may accuse loved ones of stealing their things. Wandering starts. They might leave the house and not remember how to get back. This is often the longest stage. Caregivers begin helping with daily routines: choosing clothes, managing medications, reminding them to bathe.
Stage 4: Moderate Dementia - The person can no longer live alone. They forget how to brush their teeth or tie their shoes. Incontinence becomes common. Speech gets choppy. They repeat phrases or use wrong words. Hallucinations or delusions may appear-thinking someone is breaking in, or that a mirror image is another person. Sleep flips: they’re awake all night, napping during the day. Agitation spikes. They might scream, hit out, or try to run away. Safety becomes critical. Door alarms, locks on cabinets, removing sharp objects-these aren’t just precautions. They’re lifelines.
Stage 5: Severe Dementia - The body shuts down. The person can’t speak. They may not recognize family. They can’t walk without help, then not at all. They lose control of swallowing. Eating becomes risky-food can go into the lungs, causing pneumonia, the most common cause of death. They sleep most of the day. They respond to touch, music, or a familiar voice-but not words. They need 24/7 care for everything: feeding, turning in bed, managing skin sores. This stage is physically exhausting for caregivers. Emotionally, it’s different. The fight is over. The person is quiet. Sometimes, that’s a kind of peace.
Memory Decline: How It Changes Across Stages
Memory doesn’t just fade. It unravels in a specific order.In the early stage, only new memories are affected. They forget what they had for breakfast, but still remember their wedding day. They can’t learn a new phone number, but recall their childhood pet’s name. This is because the hippocampus, which records new experiences, is the first to fail.
By the middle stage, both short-term and long-term memory are crumbling. They forget their own address. They don’t recognize their grandchildren. They ask the same question 20 times in an hour. The brain isn’t just losing data-it’s losing the ability to retrieve it. Even when given clues, they can’t piece it together.
In late stage, memory is gone. But something else remains: emotion. They may not know who you are, but they calm when you hold their hand. They smile when they hear a song from their youth. That’s why music therapy works. It bypasses broken memory circuits and taps into deeper, older pathways.
It’s important to know: not all memory loss is Alzheimer’s. Frontotemporal dementia, for example, starts with personality changes or language problems-not memory loss. That’s why proper diagnosis matters. Treating the wrong condition can make things worse.

What Caregivers Need to Know
Caring for someone with Alzheimer’s isn’t a job. It’s a full-time, emotionally draining, physically exhausting life shift. The Alzheimer’s Association says caregivers spend an average of 27 hours a week providing unpaid care. Nearly 4 in 10 say their emotional stress is high or very high. One in three report physical strain.Early stage: Support independence. Use calendars, reminder apps, labeled cabinets. Don’t correct them when they forget. Say, “Let’s look at the calendar together,” instead of, “You just asked me that.”
Middle stage: Structure is everything. Keep routines-same meals, same bedtime, same walk route. Reduce choices: “Do you want the blue shirt or the gray one?” not “What do you want to wear?” Install door alarms. Remove rugs. Lock up medications and sharp objects. Use validation therapy: if they think they need to go to work, don’t argue. Say, “Let’s get you dressed for your shift.” Then gently redirect.
Late stage: Focus on comfort. Turn them every two hours to prevent bedsores. Use soft foods, thickened liquids if swallowing is hard. Play their favorite music. Hold their hand. Talk in calm, slow tones. Even if they don’t respond, they still feel your presence.
Many caregivers feel guilty for being angry, tired, or wanting a break. That’s normal. You’re not failing. You’re human.
Support for Caregivers Isn’t Optional-It’s Essential
Caregivers burn out. And when they do, the person with Alzheimer’s suffers too.Respite care is critical. Medicare covers up to five days of inpatient respite care per benefit period for those enrolled in hospice. Local Area Agencies on Aging often offer free or low-cost in-home help, day programs, or adult day care. Don’t wait until you’re exhausted to ask. Reach out now.
Support groups work. Talking to someone who gets it-someone who’s been accused of stealing their own mother’s jewelry at 3 a.m.-changes everything. Online forums like the Alzheimer’s Association Community or Reddit’s r/dementia are full of real stories, real tips, real relief.
And don’t ignore your own health. Sleep. Eat. Move. See your doctor. If you’re running on caffeine and guilt, you’re not helping anyone.
What’s New in Treatment?
For decades, the only options were drugs like donepezil or memantine. They helped with symptoms for a while, but didn’t slow the disease.That changed in January 2023, when the FDA approved lecanemab (Leqembi). It’s the first treatment that actually targets amyloid plaques. In trials, it slowed cognitive decline by 27% over 18 months. It’s not a cure. It’s not for everyone. It requires monthly IV infusions and regular brain scans to check for swelling or bleeding-a side effect called ARIA. It costs tens of thousands a year. And it’s only for people in the early stages, with confirmed amyloid buildup.
Another drug, donanemab, is expected for approval in 2024. More are in the pipeline, targeting tau proteins, inflammation, and metabolism. Blood tests to detect Alzheimer’s before symptoms hit are coming within five years. But here’s the catch: these treatments are expensive. They’re not available in most countries. And they don’t help those already in late stages.
For now, the best treatment is still care. Compassionate, consistent, patient care.
What Comes Next?
Alzheimer’s is rising. In 2024, 6.9 million Americans had it. By 2060, that number will double. Globally, over 55 million people live with dementia. Costs hit $1.3 trillion a year. The system isn’t ready.But change is happening. More hospitals have memory clinics. More communities offer caregiver training. More research is focused on prevention-sleep, exercise, diet, managing blood pressure and diabetes-all linked to lower risk.
If you’re caring for someone with Alzheimer’s, you’re not alone. You’re part of a quiet army doing the hardest work there is. You don’t need to be perfect. You just need to show up. And sometimes, that’s enough.
Is Alzheimer’s the same as dementia?
No. Dementia is an umbrella term for memory loss and cognitive decline caused by various diseases. Alzheimer’s is the most common type, making up 60-80% of cases. Other types include vascular dementia, Lewy body dementia, and frontotemporal dementia. Each affects the brain differently and has different symptoms.
Can Alzheimer’s be prevented?
There’s no sure way to prevent Alzheimer’s, but research shows certain habits lower risk. Regular physical activity, heart-healthy eating (like the MIND diet), quality sleep, managing blood pressure and diabetes, staying socially active, and challenging your brain with puzzles or learning new skills can help. What’s good for your heart is good for your brain.
When should I seek a diagnosis?
If memory problems are disrupting daily life-forgetting how to use the stove, getting lost in your own neighborhood, or having trouble managing money-it’s time to see a doctor. Early diagnosis gives you time to plan, access treatments, and participate in clinical trials. It also rules out other treatable causes like vitamin deficiencies, thyroid issues, or depression.
Why do people with Alzheimer’s repeat the same questions?
They’ve forgotten they asked it. Their brain can’t store the answer, so the question feels new every time. Correcting them or saying, “You just asked that,” increases frustration. Instead, answer calmly each time, or gently redirect: “Let’s go sit down and have some tea,” or “I’ll write that down for you.”
How do I know if I’m becoming a burnout caregiver?
Signs include constant exhaustion, irritability, withdrawal from friends, neglecting your own health, feeling hopeless, or crying often without knowing why. If you’re thinking, “I can’t do this anymore,” you’re not weak-you’re reaching your limit. Reach out. Use respite care. Talk to a counselor. Your well-being matters as much as theirs.
What happens if I can’t care for them at home anymore?
It’s not failure-it’s a necessary step. Memory care units in assisted living or nursing homes are designed for Alzheimer’s patients. Staff are trained in behavior management, safety, and communication. Many families find their loved one is safer, more engaged, and even happier there. Visit first. Ask about staffing ratios, activities, and how they handle wandering or aggression.
Are there any apps or tools that help caregivers?
Yes. Apps like Caring Village let families share updates and coordinate tasks. Medisafe reminds patients to take pills. Alzheimer’s Association has a 24/7 helpline (1-800-272-3900) and online tools for finding local services. GPS trackers can help if wandering is a risk. Simple tools like large-print calendars, labeled drawers, and night lights make daily life easier.





Gillian Watson
December 1, 2025 AT 18:09Jordan Wall
December 2, 2025 AT 18:57Gareth Storer
December 4, 2025 AT 07:05Pavan Kankala
December 4, 2025 AT 15:26Martyn Stuart
December 4, 2025 AT 17:46Jessica Baydowicz
December 5, 2025 AT 02:59