When someone in your family has had cancer young-breast cancer before 45, ovarian cancer, colon cancer in their 30s-it’s natural to wonder: could this be genetic? The answer isn’t simple, but genetic testing has made it possible to find out. For many people, knowing their risk isn’t just about fear-it’s about taking control. Tests for BRCA1, BRCA2, and Lynch syndrome genes can change the course of your health, and even save your life.
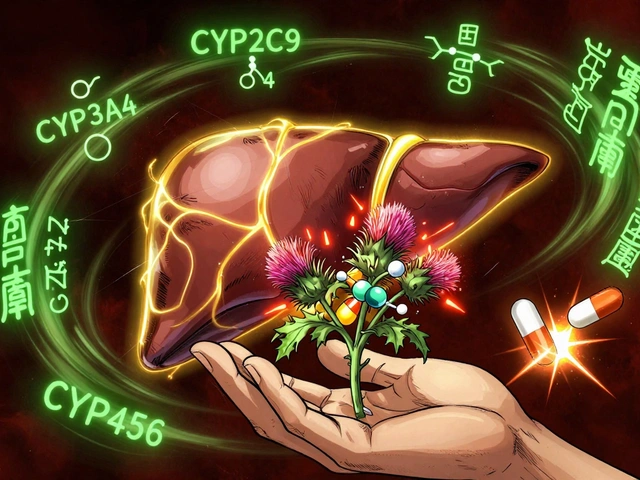
What BRCA and Lynch Actually Mean for Your Risk
BRCA1 and BRCA2 aren’t just names. They’re genes that help repair damaged DNA. When they’re broken by an inherited mutation, cells can’t fix errors properly. That’s when cancer starts to grow. Women with a BRCA1 mutation have up to a 72% chance of developing breast cancer by age 80. For BRCA2, it’s around 69%. Ovarian cancer risk jumps to 44% for BRCA1 and 17% for BRCA2. Compare that to the general population: about 13% for breast cancer and less than 2% for ovarian. That’s not a small difference.
Lynch syndrome is different. It’s caused by mutations in MLH1, MSH2, MSH6, PMS2, or EPCAM genes. These affect how your body handles DNA mistakes during cell division. People with Lynch have a 10% to 80% lifetime risk of colorectal cancer, depending on which gene is affected. Endometrial cancer risk can hit 60% for women. That’s why colonoscopies start as early as age 20-25 for these individuals-instead of 45 like for most people.
Why Multigene Panels Are Now the Standard
Testing just for BRCA used to be the norm. But in 2025, that’s outdated. A single-gene test misses up to half of the people who carry dangerous mutations. That’s because other genes-like PALB2, ATM, CHEK2, and RAD51C-are now known to raise cancer risk too. The current standard is a multigene panel test. These analyze 30 to 80 genes at once using next-generation sequencing. The detection rate for single-letter DNA errors is 99.5%. For larger deletions or duplications, it’s 95%.
One popular test, MyRisk by Myriad Genetics, checks 63 genes recommended by the National Comprehensive Cancer Network. It’s accurate to 99.8% and used in most major cancer centers. But here’s the catch: the more genes you test, the more likely you are to get a result you can’t easily understand-a Variant of Uncertain Significance, or VUS.
The VUS Problem-And How It’s Getting Better
A VUS means a DNA change was found, but scientists don’t know yet if it causes cancer. Five years ago, about 12% of BRCA test results were VUS. That caused panic. People would get scared, make drastic decisions, or delay care. But in February 2025, a landmark study from Mayo Clinic changed everything. Researchers used CRISPR to test nearly 7,000 different BRCA2 variants in the lab. They found that 91% of the previously unclear ones were actually harmless or clearly dangerous. That dropped the VUS rate in that region from 12.7% to just 1.1%.
This isn’t just science-it’s life-changing. Over 14,300 people who got a VUS result in the past will now get a clearer answer. Still, VUS rates for broader panels hover around 7.8%. That’s why genetic counseling isn’t optional. You need someone who knows how to interpret these results before you make any medical decisions.
Who Should Get Tested?
You don’t need to have cancer to qualify. The National Comprehensive Cancer Network says you should consider testing if:
- You were diagnosed with breast cancer before age 50
- You have ovarian, pancreatic, or metastatic prostate cancer at any age
- Multiple relatives on the same side have breast, ovarian, colon, or endometrial cancer
- A family member tested positive for a known cancer gene mutation
- You’re of Ashkenazi Jewish descent and have any personal or family history of breast, ovarian, or pancreatic cancer
Even if you don’t meet all these criteria, if you’re worried, talk to your doctor. Testing is covered by Medicare and most private insurers if you meet NCCN guidelines. The approval rate is 98.7%.
What DTC Tests Like 23andMe Don’t Tell You
23andMe offers a BRCA test for $99. It sounds tempting. But here’s the truth: it only checks for three specific mutations common in people of Ashkenazi Jewish descent. That’s it. If you’re not from that background, it misses over 97% of harmful BRCA mutations. A 2024 study in the New England Journal of Medicine found that 9 out of 10 people with a dangerous BRCA variant got a false “negative” from 23andMe.
These tests also don’t include Lynch syndrome genes, PALB2, or any of the other 60+ genes on clinical panels. And they don’t offer counseling. If you get a positive result, you’re on your own. That’s dangerous. A false sense of security can be worse than no test at all.
What Happens After a Positive Result?
A positive result isn’t a death sentence. It’s a roadmap. For BRCA carriers, risk-reducing surgeries can cut cancer risk by up to 80%. A 2023 study of over 12,000 women showed that those who had their breasts and ovaries removed lived longer and had far fewer cancers. Many choose to start annual breast MRIs and mammograms every six months instead. Some take tamoxifen or other drugs to lower risk.
For Lynch syndrome, colonoscopies every 1-2 years starting at age 20-25 catch polyps before they turn cancerous. Some people take aspirin daily-studies show it cuts colorectal cancer risk by 50% in Lynch carriers. In one case at Fred Hutchinson Cancer Center, a 42-year-old with Lynch syndrome and colon cancer responded completely to immunotherapy because their tumor had the specific genetic signature that made it vulnerable.
The Hidden Costs-Insurance, Emotion, and Access
There’s a myth that GINA, the Genetic Information Nondiscrimination Act, protects you completely. It doesn’t. GINA stops health insurers from using your genetic data to deny coverage or raise rates. But it doesn’t cover life insurance, disability insurance, or long-term care. Some people have been denied life insurance after testing positive-even if they never had cancer.
Emotionally, results can be overwhelming. A 2024 survey found that 22% of people who got a VUS result had severe anxiety. One Reddit user wrote: “I got a VUS. I couldn’t sleep. I started Googling every symptom I had.”
Access is uneven. In academic hospitals, 48% of eligible patients get tested. In community clinics, it’s just 21%. Black patients are tested at less than half the rate of white patients. That’s not just a gap-it’s a crisis.
The Future: Polygenic Scores and Universal Testing
Researchers at Stanford just mapped 380 DNA variants that control how genes turn on and off across 13 cancer types. These aren’t single-gene mutations. They’re subtle changes that, when combined, can nudge your risk up or down. That’s the next frontier: polygenic risk scores. In five to ten years, your cancer risk might be calculated from hundreds of tiny genetic signals-not just one broken gene.
Meanwhile, oncologists are pushing for universal germline testing for everyone diagnosed with cancer. Why? Because if you have cancer, your genes might affect your treatment. BRCA mutations make tumors more sensitive to PARP inhibitors. Lynch tumors respond better to immunotherapy. Testing everyone means more people get the right drugs.
Right now, only 33% of eligible cancer patients get tested. The goal is 100%. The technology is ready. The cost? Around $450 out-of-pocket if you’re uninsured. That’s still a barrier. But as prices drop and insurance expands, it’s becoming routine.
What to Do Next
If you’re thinking about testing:
- Write down your family history: who had cancer, how old, what type
- Ask your doctor if you meet NCCN testing criteria
- Request a referral to a certified genetic counselor
- Don’t use DTC tests for medical decisions
- Get tested before making any major health choices
Genetic testing isn’t about predicting the future. It’s about changing it. For many, it’s the difference between a diagnosis and prevention. Between fear and control. Between life and death.
Is genetic testing for cancer risk covered by insurance?
Yes, if you meet clinical guidelines from the National Comprehensive Cancer Network (NCCN). Medicare covers testing with a 98.7% approval rate, and most private insurers follow suit. You typically need a family history of early-onset cancer or a known mutation in the family. Out-of-pocket costs for self-pay range from $250 to $500. Some labs offer financial assistance programs if you’re uninsured.
Can I get tested even if I haven’t had cancer?
Absolutely. In fact, most people tested haven’t had cancer yet. Testing is designed to find risk before cancer develops. If you have close relatives with early-onset breast, ovarian, colon, uterine, or pancreatic cancer, you’re a candidate-even if you’re healthy. Preventive steps like earlier screenings or surgery can reduce your risk by up to 80%.
What’s the difference between BRCA and Lynch syndrome testing?
BRCA testing focuses on breast, ovarian, pancreatic, and prostate cancer risk. Lynch syndrome testing looks at genes that raise the risk of colorectal, endometrial, stomach, ovarian, and other cancers. They’re different genes, different cancer types, and different prevention strategies. Most modern panels test for both at the same time.
What if I get a Variant of Uncertain Significance (VUS)?
A VUS means the result isn’t clear yet. Don’t make medical decisions based on it. You’re not high-risk, but you’re not clear either. Most VUS results are reclassified over time as more data becomes available. Follow up with your genetic counselor every 1-2 years. Labs like Myriad and Invitae automatically notify patients if a VUS is reclassified. In 2025, advances in lab research have cut BRCA2 VUS rates by over 90%.
Can I test my children for these mutations?
Generally, no-unless there’s a clear medical benefit in childhood. Most hereditary cancer syndromes don’t cause cancer until adulthood. Testing kids is discouraged unless a child has symptoms or a known high-risk mutation that requires early screening (like in Lynch syndrome, where colonoscopies may start in teens). Genetic counselors recommend waiting until adulthood so the person can make their own informed choice.
Are there risks to getting tested?
Yes. Emotional stress, anxiety from uncertain results, and potential insurance discrimination (for life, disability, or long-term care) are real concerns. Some people feel guilt if they test positive and pass the mutation to their children. But for most, the benefits-early detection, prevention, targeted treatment-far outweigh the risks. Counseling helps manage these emotions.
Final Thoughts
Genetic testing isn’t magic. It won’t tell you exactly when or if you’ll get cancer. But it gives you power. Power to start screenings earlier. Power to choose surgery before cancer forms. Power to know your treatment options if you do get sick. It’s not for everyone. But for those with a family history, it’s one of the most impactful tools in modern medicine.
Don’t wait for a diagnosis to ask the question. Ask it now. Talk to your doctor. Find a genetic counselor. Get the facts. Your future self will thank you.



Patrick Marsh
November 24, 2025 AT 18:25BRCA testing saved my sister’s life. She got screened at 32, had a prophylactic mastectomy, and now she’s cancer-free at 40. Don’t wait for symptoms.
Ravi Kumar Gupta
November 25, 2025 AT 08:28In India, we don’t talk about this-cancer is whispered about like a curse. But this? This is power. My aunt died of ovarian cancer at 38. I just got tested. If I’m positive, I’m not waiting. I’m acting. This isn’t fear-it’s defiance.
Nikhil Chaurasia
November 26, 2025 AT 02:39I’m from a small town in Uttar Pradesh. We don’t have genetic counselors. My cousin got a VUS result last year and just… stopped talking. I wish someone had explained it to her. This article? It’s the first thing that made sense.
Holly Schumacher
November 26, 2025 AT 22:36Let me be crystal clear: 23andMe is a marketing gimmick wrapped in a DNA kit. It doesn't test for Lynch, PALB2, CHEK2, or even 97% of BRCA variants outside Ashkenazi Jews. And if you think a $99 saliva swab replaces clinical-grade testing with counseling? You're not just misinformed-you're endangering your life. The NCCN guidelines exist for a reason. Stop trusting consumer tech with your biology.
Michael Fitzpatrick
November 27, 2025 AT 19:44I’ve been thinking about this since my mom passed from endometrial cancer at 41. I didn’t know Lynch was a thing until last year. I got tested last month-turned out I’m positive for MSH2. I’m not scared anymore. I’m just… ready. I started colonoscopies every two years, and I’m taking low-dose aspirin like they said. It feels weird to say this, but I feel more in control than I have in years. Honestly? I wish I’d done this ten years ago. You don’t need to be a scientist to get this done. Just be brave enough to ask your doctor.
Shawn Daughhetee
November 28, 2025 AT 02:38my grandma had breast cancer at 40, my mom got it at 43, i’m 35 and i’ve been putting off testing because i’m scared of what i might find… but reading this made me realize i’m not being careful, i’m being cowardly. going to call my doctor tomorrow
Justin Daniel
November 29, 2025 AT 00:34Love how this breaks down the science without the jargon. Also, big shoutout to the part about insurance gaps-life insurance discrimination is the silent epidemic nobody talks about. I got denied coverage after my BRCA+ result, even though I’ve never had cancer. It’s not just medical-it’s financial trauma. But hey, at least we’re talking about it now. Progress.
Melvina Zelee
November 30, 2025 AT 02:57my mom got a vus and we all freaked out for months… then last year they reclassified it as benign. i still cry thinking about how much stress we went through over nothing. please, if you get a vus-breathe. talk to your counselor. don’t google. and don’t rush into surgery. it’s not a sentence. it’s a question. and questions get answered.
ann smith
December 1, 2025 AT 17:41This is exactly the kind of information we need to spread. 🙏 Genetic testing isn’t scary-it’s a gift. A gift of time, of choice, of life. Thank you for writing this with such clarity and heart. You’ve given people hope, not fear.
Julie Pulvino
December 2, 2025 AT 10:31Just got my multigene panel results back-no mutations found. But I’m still getting annual MRIs because my mom had triple-negative at 39. Sometimes the absence of a mutation doesn’t mean absence of risk. Family history still matters. This article nailed it.
Danny Nicholls
December 3, 2025 AT 00:14so i took the 23andme test because it was cheap… and got a ‘negative’ for BRCA. then i went to my doctor and got the full panel. turns out i had a pathogenic BRCA2 variant. 23andme missed it. don’t be me. get real testing. 💯