TCA Therapeutic Drug Monitor
Tricyclic Antidepressant Monitoring Tool
This calculator determines if your TCA blood levels are within the therapeutic range. Enter the measured concentration and select the specific TCA medication to check for potential toxicity risks.
Therapeutic Range
Your level is within the safe therapeutic window.
Tricyclic antidepressants (TCAs) like amitriptyline and nortriptyline aren’t just old-school meds-they’re dangerous if not handled with care. A single extra pill can send someone into cardiac arrest. Even at prescribed doses, these drugs sit on a razor’s edge between helping and harming. That’s why therapeutic drug monitoring isn’t optional-it’s life-saving.
Why TCAs Are So Risky
TCAs work by boosting serotonin and norepinephrine in the brain, which helps lift depression. But they don’t stop there. They also block receptors in the heart, gut, and nervous system. That’s why side effects like dry mouth, blurred vision, and constipation are common. In overdose, they become lethal. They slow down the heart’s electrical signals, widening the QRS complex on an ECG. When that number hits over 100 milliseconds, you’re looking at ventricular arrhythmias, seizures, or sudden death.Unlike newer antidepressants like SSRIs, TCAs have a tiny window between a therapeutic dose and a toxic one. For amitriptyline, the safe range is 80-200 ng/mL. Go above 500 ng/mL, and the risk of death spikes. And here’s the scary part: some people reach toxic levels just by taking their normal dose. Why? Because their body processes the drug too slowly.
How Therapeutic Drug Monitoring Works
Therapeutic drug monitoring (TDM) means checking blood levels to make sure the drug stays in the safe zone. It’s not about guessing based on symptoms-it’s about hard numbers.To get an accurate reading, blood must be drawn right before the next dose-that’s called the trough level. This tells you the lowest concentration in the bloodstream, which reflects steady-state levels. It takes about 5 to 7 days of consistent dosing to reach that point. If you draw blood too early, the number is meaningless.
Lab tests use high-performance liquid chromatography (HPLC) or mass spectrometry to measure the exact concentration of the drug and its metabolites. For example:
- Amitriptyline: 80-200 ng/mL
- Nortriptyline: 50-150 ng/mL
- Desipramine: 100-300 ng/mL
These aren’t arbitrary numbers. They’re based on decades of clinical data showing what levels correlate with symptom relief versus toxicity. But even within these ranges, some people react badly. That’s why TDM isn’t just about the number-it’s about pairing it with what the patient is actually experiencing.
Who Needs TDM the Most
Not everyone on TCAs needs regular blood tests. But certain groups are at much higher risk:- Elderly patients (especially over 65): Their liver and kidneys clear drugs slower. They’re also more sensitive to anticholinergic effects like confusion and urinary retention. About 40% of TCA users are seniors.
- People on multiple medications: Drugs like fluoxetine, paroxetine, or even some antibiotics can block the enzymes (CYP2D6, CYP2C19) that break down TCAs. This can cause levels to spike without any dose change.
- Patients with liver disease: Reduced metabolism means drugs build up faster.
- Those with genetic variations: About 5-10% of people are poor metabolizers-they process TCAs extremely slowly. Others are ultrarapid metabolizers and need much higher doses. Genetic testing can now identify this before a single pill is taken.
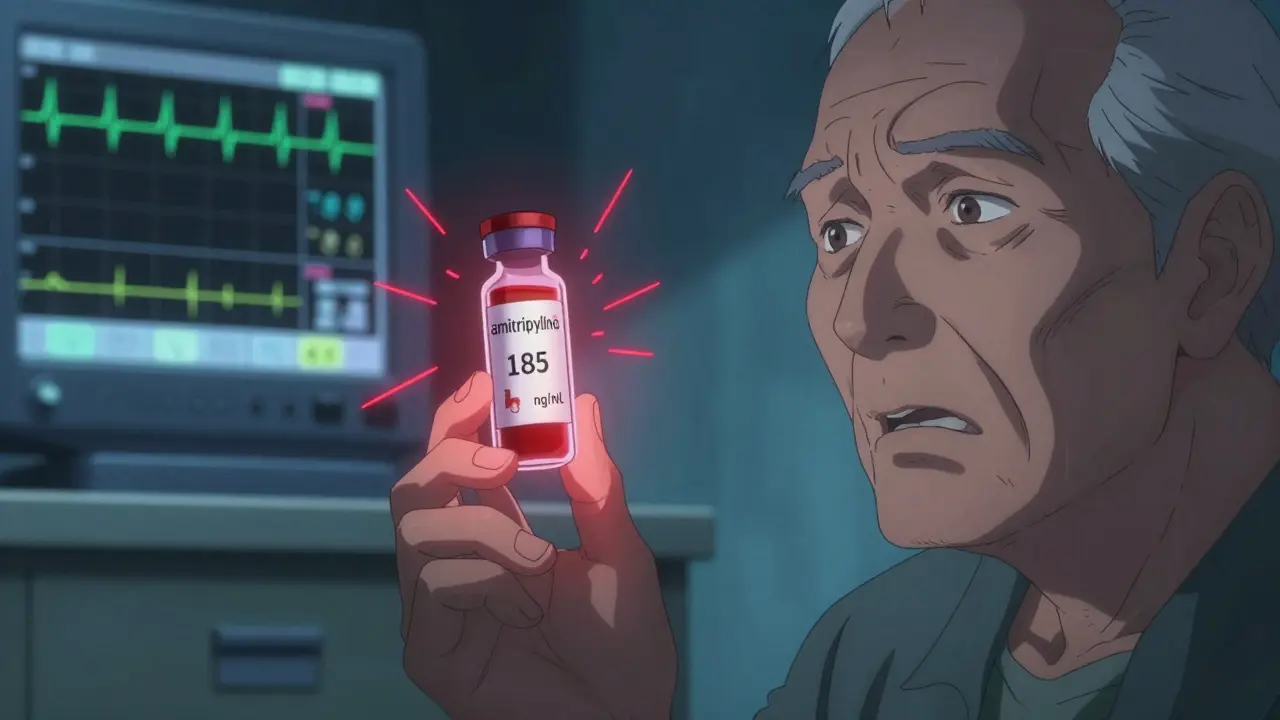
One case from Johns Hopkins involved an 82-year-old man on 150 mg of nortriptyline daily. His blood level hit 185 ng/mL-above the safe limit. He had no symptoms yet. But because his TDM result was reviewed, his dose was cut in half. A week later, his level dropped to 110 ng/mL. He stayed stable. Without that test, he might have slipped into a fatal arrhythmia.
What Happens When TDM Is Ignored
In the Victorian Poisons Information Centre, which handles over 13,000 poisoning cases a year, 65% of severe TCA poisonings involved patients whose TDM was either never done or misread. Doctors saw a "therapeutic" level and assumed safety. But the patient had an ECG showing a QRS width of 140 ms-clearly toxic. The blood level was within range, but their body reacted like it was way over. That’s the problem with relying only on numbers.Another issue: timing. Many labs take 24-48 hours to return results. By then, if a patient is crashing, it’s too late. That’s why clinical signs matter more than lab reports in emergencies. If someone has a wide QRS, seizures, or low blood pressure, you treat immediately-don’t wait for the test.
And here’s a hidden problem: incomplete paperwork. A study across European clinics found that 37.5% of TDM requests didn’t list what other drugs the patient was taking. Without that, the lab can’t explain why levels are high. One patient’s nortriptyline level was 220 ng/mL-way above normal. Turns out, they were on an antibiotic that blocked their liver enzyme. The doctor didn’t know. The dose was increased again. The patient ended up in ICU.
How TDM Saves Lives
Despite the challenges, TDM reduces hospitalizations by 35% compared to dosing based on symptoms alone. A 2020 American Psychiatric Association guideline calls TDM for TCAs a "Level 1" recommendation-meaning the evidence is strong enough to make it standard practice.Psychiatrists in real-world settings report similar results. One provider on Reddit, u/NeuroChemMD, said they’ve prevented at least three ICU admissions this year just by checking levels in elderly patients. Another nurse practitioner noted the biggest hurdle isn’t the test-it’s getting patients to come back for blood draws when they feel fine. But skipping the test because "they’re doing okay" is like driving without a speedometer.
There’s also data showing that when TDM is used correctly, patients are more likely to stick with their medication. They trust the process. They know their doctor isn’t just guessing. That builds adherence-and adherence saves lives.
What’s Changing Now
The field is evolving. New tools are making TDM faster and smarter:- Point-of-care devices: Siemens Healthineers launched a handheld TCA monitor in Europe that gives results in 20 minutes instead of two days.
- AI platforms: The FDA-cleared PsychX Analytics system now combines TDM results with ECG data, age, weight, and other meds to predict toxicity risk before symptoms appear.
- Genetic testing: Testing for CYP2D6 and CYP2C19 variants lets doctors start with the right dose from day one. Mayo Clinic found this cuts the number of TDM tests needed by 40%.
Even though TCA prescriptions have dropped 80% since 2000, they’re still used for treatment-resistant depression and chronic pain. In neuropathic pain, nortriptyline is first-line for 68% of specialists. And for older adults with depression who didn’t respond to SSRIs, TCAs remain one of the few options.
That’s why TDM isn’t going away. It’s becoming more precise.
What You Should Do
If you or someone you know is on a TCA:- Ask if TDM has been ordered. Don’t assume it’s automatic.
- Make sure the blood draw happens at the right time-right before your next dose.
- Bring a full list of all medications, including supplements and OTC drugs.
- Ask for your results. Don’t just take the doctor’s word that it’s "fine."
- Know the warning signs: fast heartbeat, confusion, trouble walking, chest pain, fainting.
If you’re a clinician: Always pair TDM with clinical assessment. A level within range doesn’t mean safety. A wide QRS means danger-even if the level is "normal."
TCAs aren’t obsolete. But they’re not safe without oversight. TDM turns guesswork into precision. It’s the difference between managing a patient and saving their life.
How often should TCA blood levels be checked?
The first test should be done after 5-7 days of consistent dosing to reach steady state. After that, check every 3-6 months if stable, or sooner if there’s a change in dose, symptoms, or other medications. Elderly patients or those with kidney/liver issues may need checks every 2-3 months.
Can I stop taking my TCA if I feel better?
Never stop abruptly. Even if you feel fine, stopping suddenly can cause withdrawal symptoms like nausea, dizziness, or rebound depression. Always taper under medical supervision. TDM helps guide safe tapering by showing how your body is clearing the drug over time.
Why do some people need lower doses than others?
Genetics play a big role. Some people have variations in the CYP2D6 or CYP2C19 genes that make them poor metabolizers-they break down TCAs very slowly. Others are ultrarapid metabolizers and clear the drug too fast. That’s why two people on the same dose can have wildly different blood levels. Genetic testing can help predict this before starting treatment.
Is TDM covered by insurance?
Most insurance plans in the U.S. and Australia cover TDM for TCAs when ordered for clinical reasons, especially in high-risk groups like the elderly or those on multiple drugs. The cost is typically $150-$250 per test. Some clinics offer bundled pricing with genetic testing. Always check with your provider before the test.
What if my TCA level is normal but I still feel awful?
A normal level doesn’t mean the drug is working-or that it’s not causing side effects. Some people are hypersensitive to TCAs even at low levels. Others may have other conditions mimicking side effects, like thyroid issues or vitamin deficiencies. Your doctor should review your full clinical picture-not just the number. An ECG, mental status exam, and medication review are just as important as the blood test.
Are there alternatives to TCA monitoring?
For many people, SSRIs or SNRIs are safer first-line options with no need for routine blood monitoring. But for treatment-resistant depression or neuropathic pain, TCAs are still effective. If you can’t tolerate TDM, discuss alternatives with your doctor. But don’t assume you can skip monitoring just because you feel okay-TCAs are silent killers until it’s too late.





Gray Dedoiko
December 23, 2025 AT 13:09Man, I had no idea TCAs were this dangerous. My uncle was on amitriptyline for years and never got tested. He just said he felt 'fine.' Guess that’s what makes it so sneaky.
Katie Taylor
December 24, 2025 AT 10:18This is the kind of post that makes me want to hug my psychiatrist. So many people think if you're not crying on the floor, you're 'doing fine.' But with TCAs, 'fine' can mean your heart’s about to throw a tantrum.
Payson Mattes
December 25, 2025 AT 17:09Wait… so you’re telling me Big Pharma doesn’t want you to get blood tests because it cuts into their profit? They’d rather you OD on a 'normal' dose so you come back for more meds? I’ve seen this before with opioids. They’re not saving lives-they’re selling fear with a lab coat.
Isaac Bonillo Alcaina
December 27, 2025 AT 14:48Let’s be clear: if your doctor isn’t ordering TDM for TCAs, they’re either negligent or lazy. There is no excuse. The data is 40 years old, the guidelines are Level 1, and the mortality risk is well-documented. You’re not 'being cautious'-you’re gambling with a human life. And if you say 'they felt fine,' you’re the reason people die in their sleep.
Pankaj Chaudhary IPS
December 28, 2025 AT 09:04As a medical professional from India, I’ve witnessed firsthand how underutilized therapeutic drug monitoring remains in low-resource settings. Many patients are prescribed TCAs without baseline ECGs or liver function tests. The cost of monitoring is often prohibitive, yet the consequences of omission are catastrophic. We need policy interventions-not just clinical awareness-to make this standard of care accessible to all, not just those in affluent clinics.
Additionally, cultural stigma around mental health often prevents patients from returning for follow-ups. A simple blood draw becomes a symbol of 'being broken,' rather than a tool of empowerment. We must reframe TDM not as surveillance, but as self-advocacy.
At our hospital, we now integrate TDM education into our initial psychiatric consultations. We show patients their own lab ranges on a printed chart. That visual cue transforms compliance. Knowledge is the first antidote to fear.
Genetic testing is still out of reach for most, but even basic pharmacokinetic education-like avoiding grapefruit or certain antibiotics-can prevent disaster. Empowerment through information is not a luxury; it’s a right.
Let us not romanticize 'old-school' medicine. TCAs are not relics-they are precision tools. And like any scalpel, they demand respect, not nostalgia.
Aurora Daisy
December 28, 2025 AT 09:22Oh wow, so now we’re treating depression like it’s rocket science? Next they’ll be requiring a PhD to take an antidepressant. In the UK, we used to just give people pills and tell them to 'cheer up.' Now it’s blood draws, genetic tests, AI predictions-what’s next, a therapist with a drone?
Meanwhile, actual mental health crises go ignored because we’re too busy running lab reports on people who ‘feel fine.’
Bhargav Patel
December 30, 2025 AT 03:01The paradox of modern psychiatry lies in its simultaneous reverence for biological reductionism and its dismissal of the existential dimensions of suffering. TCAs, in their crude pharmacological precision, force us to confront the materiality of the mind-how a molecule, invisible and silent, can alter the architecture of consciousness and the rhythm of the heart.
Yet, in our obsession with quantification-the ng/mL, the QRS width, the CYP2D6 allele-we risk mistaking measurement for meaning. The patient who feels numb, not because their nortriptyline is too high, but because their soul has been hollowed by years of isolation-can a lab report heal that?
TDM saves lives, yes. But it does not answer the deeper question: Why do we need such dangerous tools in the first place? Why is the only path to relief for so many still a chemical that can kill them if they breathe wrong?
Perhaps the real therapeutic intervention is not the blood draw, but the society that makes such interventions necessary.
Sidra Khan
December 30, 2025 AT 07:32siddharth tiwari
December 30, 2025 AT 18:40Jeffrey Frye
January 1, 2026 AT 05:12Let’s be real-most of these 'TDM saves lives' stats are from academic hospitals with 24/7 psych teams. In the real world? Most docs just prescribe and forget. I’ve seen patients on 200mg amitriptyline for 3 years with zero labs. And yeah, they’re 'fine' until they’re not. Then it’s too late. The system’s broken. We’re just papering over it with fancy acronyms.
Also, who’s paying for these $200 tests when you’re on Medicaid? Huh? Exactly.
Andrea Di Candia
January 2, 2026 AT 20:16I think this is one of those rare moments where medicine actually gets it right. It’s not about control-it’s about care. TCAs are like a powerful engine: if you don’t check the oil, you’re just one twist away from total failure. But when you do? You’re not just surviving-you’re living.
I’ve watched patients who were on the edge of giving up find stability because someone took the time to look at their numbers, not just their mood. That’s not overmedicalizing. That’s honoring someone’s humanity.
And yeah, it’s inconvenient. But so is burying someone because we were too rushed to ask, 'Have you had your levels checked?'
Raja P
January 2, 2026 AT 22:47Thanks for this. My dad’s on nortriptyline and I’ve been nagging him to get his levels checked. He said, 'I don’t feel sick, why bother?' Now I’ve got the whole article to show him. He’s gonna roll his eyes, but maybe… just maybe… he’ll go.