Ever felt a sudden tightness in your chest that makes it hard to breathe? That’s a bronchospasm. It happens when the muscles around your airways squeeze shut, cutting the flow of air. The result can feel like an asthma attack, even if you don’t have asthma. Knowing the basics helps you stay calm and act fast.
Many things can set off the spasm. Common culprits are cold air, strong smells, dust, smoke, and even intense exercise. Allergens like pollen or pet dander also play a part, especially for people with allergic asthma. Some medicines, such as beta‑blockers, can provoke a reaction too. If you notice a pattern – say, shortness of breath after cleaning with harsh chemicals – you’ve probably found a trigger.
The first thing to do is stay as relaxed as possible. Panic makes the muscles tighten more. Sit upright, not flat, and try slow, steady breaths through your nose. If you have a rescue inhaler (usually a short‑acting beta‑agonist like albuterol), take one or two puffs right away. Use a spacer if you have one; it delivers the medicine deeper into the lungs.
After the inhaler, wait a minute and see if your breathing improves. If you still feel tight, you can repeat the dose after five minutes, but no more than the amount your doctor prescribed. Keep sipping small sips of water – it helps keep the throat moist and may ease the feeling of a lump.
If symptoms don’t get better within 10‑15 minutes, or if you notice wheezing, bluish lips, or severe shortness of breath, call emergency services. A bronchospasm can become life‑threatening fast, and professional help may be needed.
Beyond the emergency, there are long‑term steps to lower the risk. Regular use of a controller inhaler (if prescribed) keeps the airway muscles from over‑reacting. Avoid known irritants – wear a mask when exposed to dust or strong odors, and keep your home free of mold and pet hair if they bother you.
Staying fit also helps. Gentle cardio, like walking, builds lung capacity without pushing the airways to the edge. If you plan intense workouts, warm up slowly and keep a rescue inhaler handy. Some people find that breathing techniques, like pursed‑lip breathing, reduce the chance of a spasm during activity.
Keep a symptom diary. Write down when a bronchospasm occurs, what you were doing, and any smells or foods nearby. This record is gold for doctors trying to pinpoint triggers and adjust treatment.
Finally, talk to your health provider about a personalized action plan. Knowing exactly which medicines to use, when to use them, and when to call for help removes guesswork and gives you confidence the next time your chest tightens.
Bronchospasm can feel scary, but with the right knowledge and quick steps, you can control it. Remember: stay upright, use your inhaler, breathe slowly, and don’t hesitate to get professional help if things don’t improve fast.
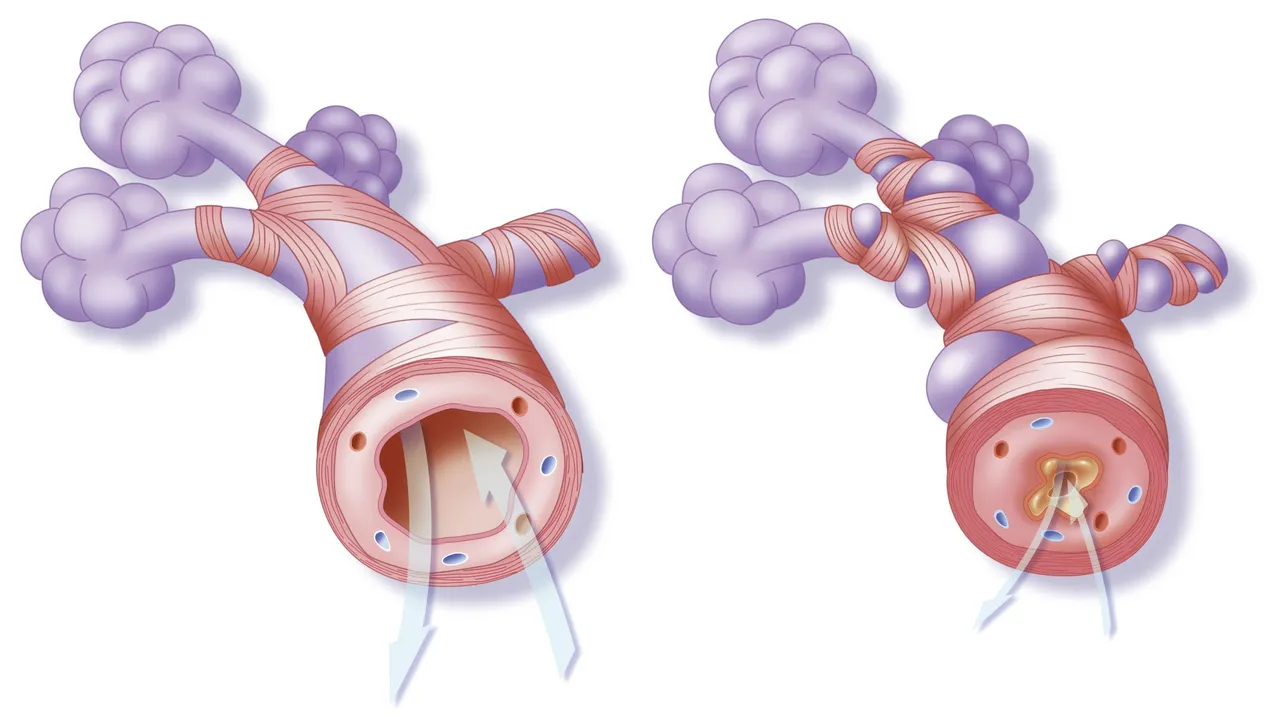
Hey there, folks! Today, we're going to have a chat about something quite significant in our health journey - the connection between Asthma and Bronchospasm. In this post, I'll be dissecting what Asthma and Bronchospasm are, why they happen, and importantly, how they are related. It's crucial for us to understand the ties between these two conditions to help manage our health better. So buckle up, it's going to be an insightful ride!
Read More