Every year, more people die from lung cancer than from breast, colon, and prostate cancers combined. And for smokers, the risk isn’t just high-it’s urgent. But here’s the good news: if you’ve smoked for years, there’s a simple, proven way to catch lung cancer early, when it’s still treatable. That’s where low-dose CT (LDCT) screening comes in. It’s not a cure. It’s not a magic bullet. But for the right people, it can mean the difference between life and death.
Who Should Get Screened?
The rules changed in 2021, and they’re simpler now. If you’re between 50 and 80 years old, and you’ve smoked at least 20 pack-years, you qualify. A pack-year means smoking one pack a day for a year. So if you smoked a pack a day for 20 years, or two packs a day for 10 years-that’s 20 pack-years. It doesn’t matter if you quit. As long as you stopped within the last 15 years, you’re still eligible.That’s a big shift from the old guidelines, which required 30 pack-years and started screening at 55. Now, millions more people are included. In the U.S., the number of eligible smokers jumped from 8.2 million to 14.5 million. That’s not just a number. That’s your neighbor, your parent, your friend. And if they’re eligible, they should know.
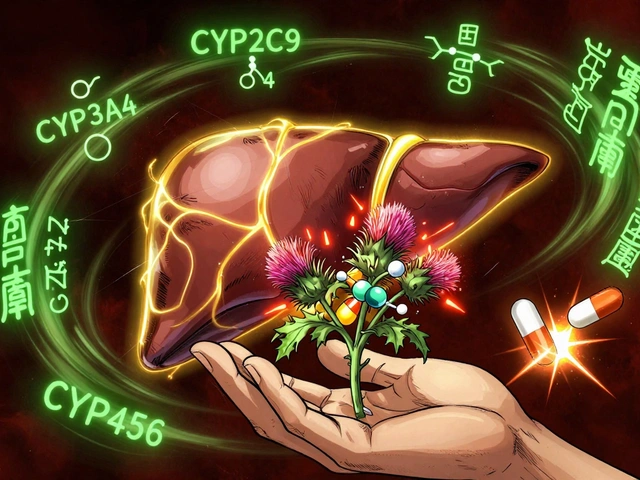
How Does Low-Dose CT Work?
It’s quick. You lie on a table. The machine spins around you. No needles. No fasting. No pain. The whole thing takes less than 10 minutes. The radiation dose is about 1.5 millisieverts-roughly the same as a mammogram, and far less than a regular CT scan, which can be five times higher.The scan doesn’t just take a picture. It gives doctors a detailed 3D view of your lungs. They look for tiny nodules-small spots that could be cancer. Most of the time, they’re harmless. But catching the dangerous ones early? That’s the goal.
What Are the Benefits?
The science is clear. The National Lung Screening Trial, published in 2011, showed that annual LDCT screening reduced lung cancer deaths by 20% compared to chest X-rays. That’s not a small win. That’s life-saving.Real people are living because of this. One woman in her early 50s, who smoked for 25 years, had a routine scan. It found a stage 1 tumor. She had surgery. Five years later, she’s cancer-free. That’s not rare. It’s repeatable. Studies estimate that expanding screening to the current guidelines could prevent up to 15,000 lung cancer deaths every year in the U.S. alone.
What Are the Risks?
It’s not perfect. About 1 in 7 people who get screened will get a false positive-meaning the scan shows something suspicious, but it turns out to be nothing. That can lead to more tests, biopsies, and anxiety. Some people report months of stress after a false alarm. And yes, there’s radiation. But the risk from a single scan is tiny. The bigger danger is waiting too long to get screened.There’s also overdiagnosis-finding cancers that would never have caused harm. But experts agree: the benefit outweighs the risk for those who qualify. The key is knowing what you’re signing up for.
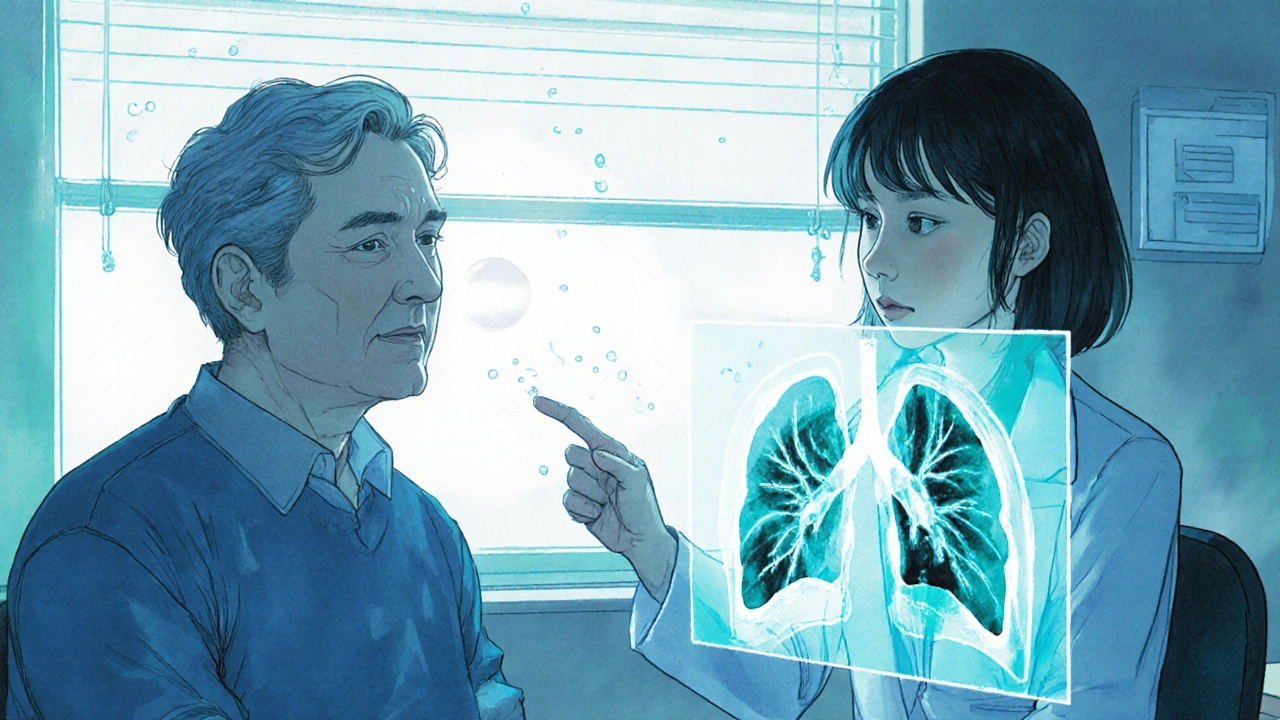
What Happens Before the Scan?
You can’t just walk in and get a scan. Medicare and most insurers require a shared decision-making visit. That means a 20- to 30-minute conversation with your doctor. No rush. No script. You talk about:- How much screening can reduce your risk (about a 1.5% to 2% absolute drop in dying from lung cancer)
- What false positives mean and how often they happen
- Whether you’re healthy enough to handle treatment if cancer is found
- What happens if you quit smoking now-screening still helps, but quitting is the best move
This isn’t paperwork. It’s a real conversation. If your doctor skips this step, ask why. You deserve to understand the pros and cons before you say yes.
What Happens After the Scan?
Results come back using a system called Lung-RADS. It grades findings from 1 to 4:- 1 (Negative): No nodules. Come back next year.
- 2 (Benign): Clear, harmless spots. Still annual screening.
- 3 (Probably Benign): Small nodule. Follow-up in 6 months.
- 4 (Suspicious): Needs faster follow-up-3 months or biopsy.
Most people fall into categories 1 or 2. But if you get a 3 or 4, don’t panic. Follow-up doesn’t mean cancer. It means caution. The system is designed to catch real threats without overtreating harmless ones.
Why Isn’t Everyone Getting Screened?
Here’s the hard truth: only about 8% of eligible smokers in the U.S. are actually getting screened. That’s not because they don’t know. It’s because:- Doctors don’t always bring it up
- People don’t realize they qualify
- Transportation or cost gets in the way
- There aren’t enough accredited centers nearby
Medicare covers it with no out-of-pocket cost if you meet the criteria. But if your doctor doesn’t know the guidelines, you won’t hear about it. A 2022 study found that 42% of eligible patients never got a recommendation. That’s on the system. Not on you.
Where Can You Get Screened?
Not every imaging center is qualified. Look for facilities accredited by the American College of Radiology (ACR). As of late 2023, there are about 1,842 of these centers across the U.S. They follow strict rules on equipment, staff training, and reporting. You can find one near you through the ACR website or by asking your doctor.Some people drive over 100 miles to get screened. That’s a barrier. But if you’re eligible, it’s worth it. Some community health centers and hospitals now have dedicated screening programs with nurse navigators who help schedule, explain, and follow up. Ask your provider if they offer one.
What’s New in 2025?
The field is evolving. AI tools are now being used to help radiologists read scans. In 2023, the FDA cleared the first AI software for LDCT analysis. Early results show it cuts false positives by over 15%. That means fewer unnecessary biopsies and less anxiety.Researchers are also building better risk models. Instead of just counting pack-years, new tools now consider family history, lung disease, and even education level. The PLCOm2012 model is already being tested in clinics. In the future, screening might not be one-size-fits-all. It could be personalized.

What If You Quit Smoking?
Quitting is the best thing you can do. But even if you quit 10 years ago, you still qualify for screening as long as it’s been less than 15 years. And if you quit, your risk drops-but it doesn’t disappear. Screening still helps. The damage from decades of smoking doesn’t vanish overnight. That’s why screening is still critical for former smokers.What If You’re Not Eligible?
If you’re under 50, or you’ve smoked less than 20 pack-years, screening isn’t recommended. That doesn’t mean you’re safe. If you have symptoms-coughing up blood, chest pain, unexplained weight loss, or a persistent cough-see your doctor. Don’t wait for a screening program. Those symptoms need attention now.What About Other Groups?
Black Americans have higher lung cancer rates but are 20% less likely to get screened. That’s a gap. People in rural areas have less access. Low-income groups are less likely to be referred. These aren’t just statistics. They’re real people missing out. If you’re in one of these groups and you qualify, push harder. Ask for the screening. Bring a friend. Call your local health department. You deserve the same chance.Final Thought: This Isn’t About Fear. It’s About Control.
Lung cancer doesn’t care if you’re rich or poor, young or old. But you can care about your risk. If you’re a smoker or former smoker who meets the criteria, this screening is your best tool. It’s not a guarantee. But it’s the most powerful one we have right now.Don’t wait for symptoms. Don’t wait for your doctor to bring it up. If you’re 50 or older and have a 20-pack-year history, call your provider today. Ask: "Am I eligible for low-dose CT screening?" That one question could save your life.
Who qualifies for lung cancer screening with low-dose CT?
You qualify if you’re between 50 and 80 years old, have smoked at least 20 pack-years (for example, one pack a day for 20 years), and currently smoke or quit within the past 15 years. Screening stops after 15 years of not smoking or if you have serious health problems that make treatment unlikely.
Is low-dose CT the same as a regular CT scan?
No. A low-dose CT uses much less radiation-about 1.5 millisieverts-compared to a standard CT, which can be 7 to 8 millisieverts. It’s designed to find lung nodules without exposing you to high radiation levels. It’s faster, safer, and just as effective for screening purposes.
Does Medicare cover low-dose CT screening?
Yes. Medicare covers annual low-dose CT screening for people aged 50 to 77 who meet the smoking history criteria. You need a doctor’s order after a shared decision-making visit. There’s no copay or deductible if you use an accredited facility.
What if my scan shows a nodule?
Most nodules aren’t cancer. If one is found, it’s graded using Lung-RADS. A category 1 or 2 means no action needed beyond next year’s scan. Category 3 means a follow-up in 6 months. Category 4 means further testing-like a biopsy-within weeks. Don’t panic. Follow-up doesn’t mean cancer. It means being careful.
Can I get screened if I’ve never smoked?
No. Current guidelines only recommend screening for current or former smokers with a 20-pack-year history. People without smoking history have much lower risk, and screening isn’t proven to help them. If you have symptoms like coughing up blood or chest pain, see a doctor regardless of smoking history.
How often should I get screened?
Once a year. Annual screening is the standard. Stopping or delaying increases your risk of missing early cancer. If you’re eligible, make it part of your yearly health routine-like a mammogram or colonoscopy.
What if I can’t find a screening center near me?
Look for ACR-accredited facilities. You can search on the American College of Radiology’s website. Some hospitals and university medical centers have dedicated lung cancer screening programs. If transportation is an issue, ask your doctor or local health department for help. Community outreach programs sometimes offer transportation or mobile screening units.
Does quitting smoking make screening unnecessary?
No. Even after quitting, your risk remains elevated for years. Screening is still recommended if you quit within the last 15 years. Quitting reduces your risk long-term, but screening helps catch cancer early during that higher-risk window.
Can AI replace radiologists in reading LDCT scans?
Not yet. AI tools are now used to help radiologists by flagging potential nodules and reducing false positives. The FDA approved the first AI software for LDCT in 2023. But human experts still review every scan. AI is a tool, not a replacement.
What’s the biggest mistake people make with lung cancer screening?
Waiting for symptoms. Lung cancer often has no signs until it’s advanced. The whole point of screening is to catch it before you feel anything. If you’re eligible, don’t wait for coughing, pain, or weight loss. Get screened now.




Liam Strachan
November 21, 2025 AT 01:04Really appreciate this breakdown. I’ve been telling my dad to get screened for months-he’s 62, smoked a pack a day for 28 years, quit 8 years ago. He kept saying ‘I’m fine, no cough’-until I showed him this. He’s booked his scan next week. Thanks for making it feel doable, not scary.
Michael Fessler
November 21, 2025 AT 18:37LDCT sensitivity is ~90% for nodules >4mm, but specificity drops to ~70% due to granulomas, fibrosis, and benign hamartomas. The Lung-RADS system helps stratify, but radiologist experience still matters-especially in high-prevalence populations. AI tools like Lunit INSIGHT and Quantib are reducing inter-reader variability by 18-22% in recent trials. Just don’t let the algorithm override clinical context.
Nosipho Mbambo
November 22, 2025 AT 18:53Okay, but… why are we screening smokers? Shouldn’t we be pushing harder for smoking cessation programs instead of just… finding cancer later? Like, isn’t this just enabling the behavior? I mean, I get it, but… it feels like putting a bandaid on a bullet wound.
daniel lopez
November 24, 2025 AT 05:55They’re lying about the radiation. 1.5 millisieverts? That’s what they want you to think. The machines are calibrated to hide the real dose. And who’s paying for all these scans? Big Pharma. They profit from biopsies, chemo, surgery. You think they want you to quit? No. They want you scanned. Year after year. Watch the ads. They never say ‘quit smoking.’ They say ‘get screened.’ Coincidence? I think not.
King Over
November 24, 2025 AT 07:03My uncle got screened last year. Found a 3mm nodule. Went in for a follow-up. Turned out to be a scar from an old pneumonia. He spent 3 months thinking he was dying. The anxiety was worse than the scan. I get it helps, but man… it’s a mental toll.
Johannah Lavin
November 25, 2025 AT 09:09I’m a nurse in rural Ohio. We’ve got one ACR-accredited center 90 miles away. Last month, a 58-year-old woman drove 4 hours with her granddaughter because she didn’t want to miss her appointment. She cried when she got her result: Lung-RADS 1. I told her, ‘You just gave yourself the gift of time.’ That’s why this matters. Not the stats. The people.
Ravinder Singh
November 26, 2025 AT 11:23Bro, if you're 50+ and smoked even a little, just do it. No excuses. I quit 12 years ago after 25 pack-years. My scan found a tiny nodule-turned out benign. But if I hadn't gone, who knows? Life’s too short to gamble with your lungs. Get it done. You got this 💪
Destiny Annamaria
November 27, 2025 AT 10:29My mom’s a former smoker. She’s 65. Her doctor never mentioned screening. She found out from a Facebook ad. That’s messed up. Why is it on us to Google this? Why isn’t it automatic? Like a mammogram? We need better systems, not just more awareness.
Russ Bergeman
November 28, 2025 AT 01:22Wait. So you’re telling me… if I smoked two packs a day for 10 years… and quit 14 years ago… I still qualify? But if I quit 16 years ago? I’m out? That’s arbitrary. Why not 20? Why not 25? This feels like a loophole. Who decided this? What’s the science behind 15?
Jeremy Samuel
November 28, 2025 AT 05:30Low dose ct? Sounds like a fancy way to say xray with more bills. I got a cousin who got scanned, got a false positive, ended up with a biopsy, then a scar, then a $12k bill. He still smokes. So… what did we really win here?
Matthew Peters
November 29, 2025 AT 08:23AI is already outperforming radiologists on nodule detection in blinded trials. The FDA cleared it, but hospitals are dragging their feet because they don’t want to change workflows. The tech is here. The data’s solid. The only thing holding us back is inertia. We’re not behind on science-we’re behind on bureaucracy.
Alyssa Torres
November 29, 2025 AT 16:24My grandma got screened last year. She’s 72. Never thought she’d qualify. She smoked 15 years, quit 18 years ago. Her doctor said no. We appealed. Found out the guidelines changed. She got the scan. Nodule was 2mm. Follow-up in 12 months. She’s now telling every friend she knows. That’s the power of information. Don’t let a doctor’s outdated memory be your barrier.
Gerald Cheruiyot
November 30, 2025 AT 08:50It’s not about fear. It’s about responsibility. We don’t wait for heart attacks to check cholesterol. We don’t wait for blindness to test for diabetes. Why do we wait for coughing to check lungs? Screening isn’t punishment. It’s prevention with pixels. The scan doesn’t judge. It just sees. And sometimes… seeing is saving
Katie Magnus
November 30, 2025 AT 11:46Okay but what if I’m a non-smoker with a family history? My dad died of lung cancer at 58. He never smoked. Shouldn’t I get screened? This feels like classist science. Only the smokers get help. What about the rest of us? It’s not fair.
Ron and Gill Day
November 30, 2025 AT 21:10They say 20 pack-years. But what if I smoked cigars? Or vape? Or used chewing tobacco? Are those excluded? This system is outdated. It’s based on 1980s data. Modern smoking isn’t just cigarettes. Why are we still using this? It’s lazy. And it’s leaving people behind.