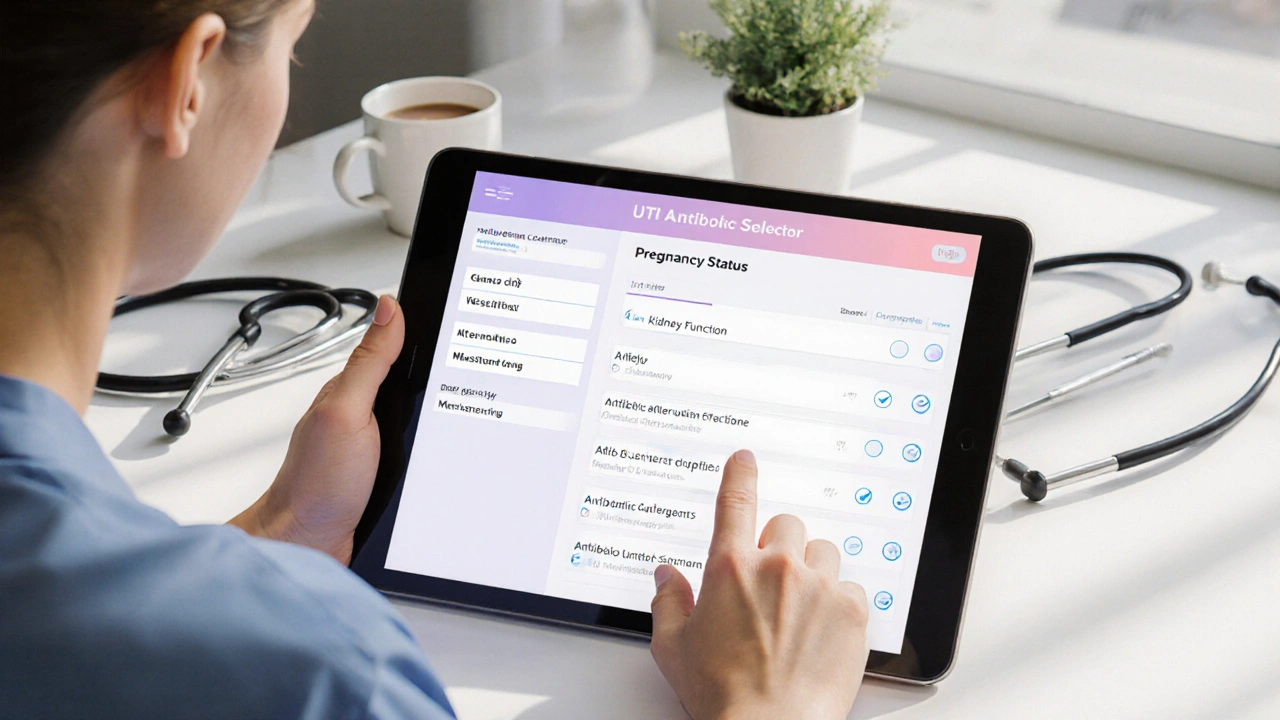
UTI Antibiotic Selector
Select Patient Profile
Choose the patient characteristics below to get personalized antibiotic recommendations.
Recommended Treatment
Click "Get Treatment Recommendation" to see personalized antibiotic suggestions based on patient profile.
This tool helps clinicians choose among fosfomycin, nitrofurantoin, TMP-SMX, ciprofloxacin, amoxicillin-clavulanate, and cephalexin based on key patient factors.
Fosfomycin has become a go‑to option for many clinicians handling uncomplicated urinary tract infections, but how does it really stack up against the older drugs on the shelf? This article breaks down the science, dosing quirks, resistance trends, and safety profiles so you can decide when a single‑dose regimen makes sense and when another antibiotic might be a better fit.
TL;DR
- Fosfomycin is a single‑dose, broad‑spectrum oral antibiotic with low resistance in most regions.
- It’s safe in pregnancy and has minimal drug‑interaction risk.
- Choose nitrofurantoin for patients with reduced kidney function (eGFR >30mL/min).
- Trimethoprim‑sulfamethoxazole remains cheap but resistance can exceed 20 % in many locales.
- Fluoroquinolones (e.g., ciprofloxacin) are powerful but should be reserved for complicated cases due to safety warnings.
What is Fosfomycin?
When treating uncomplicated urinary tract infections, Fosfomycin is a broad‑spectrum oral antibiotic administered as a single 3g dose of fosfomycin trometamol. It inhibits the early stage of bacterial cell‑wall synthesis by targeting the enzyme MurA, a mechanism that differs from beta‑lactams and fluoroquinolones.
Pharmacokinetically, the drug reaches peak urine concentrations within 2-3hours and remains above the minimum inhibitory concentration (MIC) for up to 48hours, which is why a one‑time dose is usually sufficient for Escherichia coli, the most common uropathogen.
Key Alternatives
Below are the most frequently prescribed oral agents for uncomplicated UTIs, each with its own strengths and limitations.
Nitrofurantoin is a nitrofuran‑derived antibiotic that concentrates in urine and is effective against many Gram‑negative and Gram‑positive uropathogens. It is given as 100mg twice daily for 5days.
Trimethoprim‑sulfamethoxazole (TMP‑SMX) combines two agents that block sequential steps in folate synthesis, typically dosed 160mg/800mg twice daily for 3days.
Ciprofloxacin is a fluoroquinolone that interferes with bacterial DNA gyrase, administered 250-500mg twice daily for 3days in uncomplicated cases.
Amoxicillin‑clavulanate pairs a beta‑lactam with a beta‑lactamase inhibitor, usually 500mg/125mg three times daily for 5-7days.
Cephalexin is a first‑generation cephalosporin given 500mg four times daily for 5days.

Direct Comparison
| Attribute | Fosfomycin | Nitrofurantoin | Trimethoprim‑SMX | Ciprofloxacin | Amoxicillin‑clavulanate | Cephalexin |
|---|---|---|---|---|---|---|
| Mechanism | MurA inhibition (cell‑wall synthesis) | Reduced bacterial metabolism (nitrofuran) | Folate pathway blockade | DNA gyrase inhibition | Beta‑lactam (PBP) + beta‑lactamase inhibition | Beta‑lactam (PBP) inhibition |
| Typical Dose | Single 3g dose | 100mg BID ×5days | 160/800mg BID ×3days | 250-500mg BID ×3days | 500/125mg TID ×5‑7days | 500mg QID ×5days |
| Spectrum | E. coli,K. pneumoniae,Enterococcus spp. | E. coli,Staphylococcus saprophyticus | E. coli,Streptococcus spp. | Broad Gram‑negative, some Gram‑positive | Broad Gram‑positive, some Gram‑negative | Gram‑positive, limited Gram‑negative |
| Resistance Rate * | ≈5% (varies by region) | ≈10% (higher in patients with prior use) | 20‑30% in many US regions | 5‑10% but rising globally | 15‑20% (beta‑lactamase producers) | 10‑15% (ESBL‑producing strains) |
| Pregnancy Safety | Category B (widely used) | Category B (avoid in 1st trimester if possible) | Category C (avoid near term) | Category C (avoid unless needed) | Category B | Category B |
| Common Side Effects | Diarrhea, mild nausea | GI upset, pulmonary toxicity (rare) | Rash, hyper‑K, GI upset | Tendonitis, QT prolongation | Diarrhea, hepatic enzyme rise | Diarrhea, allergic rash |
*Resistance rates are based on surveillance data up to 2024 and can differ locally. Always check your regional antibiogram.
When Fosfomycin Is the Right Choice
- Patient prefers a single dose to improve adherence.
- Pregnant woman (any trimester) where safety is paramount.
- History of fluoroquinolone or nitrofurantoin adverse reactions.
- Local resistance to TMP‑SMX exceeds 20%.
- Kidney function is adequate (eGFR>30mL/min) - drug requires urinary excretion.
Because Fosfomycin reaches high urinary concentrations and maintains activity for 48hours, it often clears the infection without the need for a multi‑day regimen. This can be a game‑changer for elderly patients who struggle with pill burden.
Scenarios Favoring Alternatives
- Nitrofurantoin is preferred when creatinine clearance falls between 30-60mL/min; it retains activity in low‑volume urine.
- Trimethoprim‑SMX remains the cheapest option and works well in regions with low resistance, especially for cost‑sensitive patients.
- Ciprofloxacin should be reserved for patients with allergies to first‑line agents or for suspected complicated infections needing deeper tissue penetration.
- Amoxicillin‑clavulanate and Cephalexin are useful when the pathogen is known to be beta‑lactam susceptible, such as in post‑procedural prophylaxis.
Always consider drug-drug interactions; fosfomycin has minimal impact on warfarin or oral contraceptives, while fluoroquinolones can potentiate QT‑prolonging meds.
Practical Checklist for Clinicians
- Check local antibiogram for current resistance patterns.
- Confirm patient’s renal function (eGFR>30mL/min for fosfomycin).
- Ask about pregnancy status and drug allergies.
- Discuss adherence: single dose vs multi‑day course.
- Choose the agent that balances efficacy, safety, and cost for the individual.

Frequently Asked Questions
Can I use fosfomycin for recurrent UTIs?
Yes, many guidelines recommend a single 3g dose after each symptomatic episode. For prophylaxis, a low‑dose (1g) regimen taken every 10‑14days has shown benefit, but it should be reserved for patients with documented multidrug‑resistant infections.
Is fosfomycin effective against ESBL‑producing bacteria?
In vitro, fosfomycin retains activity against many ESBL‑producing Enterobacteriaceae, especially when urinary concentrations exceed the MIC. Clinical data support its use as an oral step‑down after initial IV therapy.
What are the main side effects to watch for?
The most common are mild gastrointestinal upset (diarrhea, nausea). Rarely, patients experience hypersensitivity reactions or elevated liver enzymes. Severe toxicity is uncommon compared with fluoroquinolones.
Can I take fosfomycin together with my birth control pills?
Fosfomycin does not induce hepatic enzymes, so it does not reduce the effectiveness of hormonal contraceptives. However, always double‑check any new medication with the patient’s pharmacist.
How do I handle a fosfomycin allergy?
Allergic reactions typically present as rash, pruritus, or, rarely, anaphylaxis. In such cases, switch to nitrofurantoin (if renal function permits) or TMP‑SMX, guided by susceptibility testing.




Katheryn Cochrane
October 1, 2025 AT 16:16Analyzing the data presented, the single‑dose claim for fosfomycin looks appealing on paper, but the devil is in the resistance trends. The table’s resistance rate of ~5% may be outdated in regions with heavy ESBL prevalence. Moreover, the safety profile for pregnant patients is often glossed over, yet teratogenic studies are limited. In practice, clinicians should cross‑reference local antibiograms before defaulting to the ‘convenient’ option.
Bottom line: convenience cannot outweigh evidence‑based stewardship.
Michael Coakley
October 2, 2025 AT 20:03Sure, becuz a single dose totally solves everything, right?
ADETUNJI ADEPOJU
October 3, 2025 AT 23:50From a pharmacodynamic standpoint, the MurA inhibition mechanism of fosfomycin is indeed novel, yet the discourse often neglects the emergent plasmid‑mediated resistance genes. One must consider the selective pressure imposed by widespread single‑dose usage, especially in low‑resource settings where surveillance is scarce. Ethical prescribing mandates that we preserve this agent for truly refractory cases, not as a blanket first‑line.
Janae Johnson
October 5, 2025 AT 03:36While many champion fosfomycin for its simplicity, I remain skeptical of its blanket recommendation without nuanced renal function assessment. The literature certainly supports its safety, yet a contrarian view reminds us that guidelines evolve.
Kayla Charles
October 7, 2025 AT 11:10Let me walk you through why an inclusive, patient‑centered approach matters when choosing a UTI antibiotic. First, consider the patient’s daily routine; a single 3 g dose of fosfomycin can dramatically improve adherence for someone juggling work, childcare, and limited pharmacy access.
Second, pregnancy safety is a genuine concern; fosfomycin’s Category B status offers reassurance, though clinicians should still discuss any uncertainties with obstetric partners.
Third, local resistance patterns cannot be ignored. If your regional antibiogram shows <5 % resistance, fosfomycin shines, but in areas where ESBL producers are rampant, you may need to combine it with an IV step‑down strategy.
Fourth, cost plays a role. Although fosfomycin can be pricier per dose than generic TMP‑SMX, the single‑dose regimen eliminates the hidden costs of missed doses and follow‑up visits.
Fifth, drug‑drug interactions are minimal, making it a safe choice for patients on anticoagulants or hormonal contraceptives.
Sixth, for patients with eGFR > 30 mL/min, fosfomycin’s renal excretion ensures high urinary concentrations, but if the kidney function dips below that threshold, nitrofurantoin becomes a more reliable alternative.
Seventh, the side‑effect profile of fosfomycin-mainly mild GI upset-is generally better tolerated than the tendon‑related warnings tied to fluoroquinolones.
Eighth, the single‑dose nature reduces the risk of developing secondary resistance that can arise from multiday courses.
Ninth, for recurrent UTIs, evidence supports a low‑dose prophylactic schedule of 1 g every 10–14 days, yet this should be reserved for documented multidrug‑resistant cases.
Tenth, patient education is crucial; explaining why a one‑time pill is sufficient can alleviate anxieties about ‘under‑treatment.’
Eleventh, always verify that the pathogen is susceptible; if cultures show resistance, switch promptly to an agent like nitrofurantoin or a tailored beta‑lactam.
Twelfth, remember to document the decision-making process in the EMR for future stewardship audits.
Thirteenth, interdisciplinary collaboration-pharmacy, nursing, and primary care-optimizes the selection and follow‑up.
Fourteenth, stay updated on emerging data; resistance trends shift, and what’s low today may climb tomorrow.
Fifteenth, consider patient preferences; some may prefer a short course despite higher out‑of‑pocket costs.
Finally, the overarching principle is to match the antibiotic to the individual’s clinical picture, not the other way around. By integrating these factors, you empower both clinician and patient toward a successful, evidence‑based outcome.
Paul Hill II
October 9, 2025 AT 18:43Great rundown on the pharmacology, and I’d add that checking for prior antibiotic exposure can help avoid unnecessary resistance pressure. A quick review of the patient’s medication list often points toward a safer choice.
Stephanie Colony
October 12, 2025 AT 02:16Patriotic physicians often tout the “American‑made” fosfomycin as the ultimate solution, yet they ignore that overseas manufacturers dominate the supply chain. Colorful marketing can’t replace solid data, and we must stay vigilant against hype.
Abigail Lynch
October 14, 2025 AT 09:50Some say fosfomycin is just a corporate push, but evidence shows it works-though I’m always skeptical of the pharma narrative.
David McClone
October 16, 2025 AT 17:23Honestly, the single‑dose miracle feels a bit too tidy; real‑world infections love to surprise us, and relying on a one‑off pill can backfire if the pathogen hides a hidden resistance mechanism.
Jessica Romero
October 19, 2025 AT 00:56I appreciate the thoroughness of the article, yet I’d caution against over‑generalizing fosfomycin’s safety without acknowledging its limited data in specific subpopulations. For instance, patients with chronic kidney disease stage 4 require dose adjustments, and the lack of robust trials there remains a gap. Additionally, while the drug‑interaction profile is favourable, clinicians should still monitor hepatic enzymes in patients on concurrent hepatotoxic agents. Ultimately, a balanced, evidence‑based approach-anchored in regional susceptibility data and individual patient factors-will serve best.