Have you ever looked up at a bright sky or a white wall and seen tiny dots, strings, or cobwebs drifting across your vision? Or maybe you’ve caught a quick flicker of light out of the corner of your eye, like a camera flash that isn’t there? These aren’t hallucinations. They’re real - and for most people over 50, they’re completely normal. But they can also be a warning sign. Knowing the difference could save your sight.
What Are Floaters and Flashes?
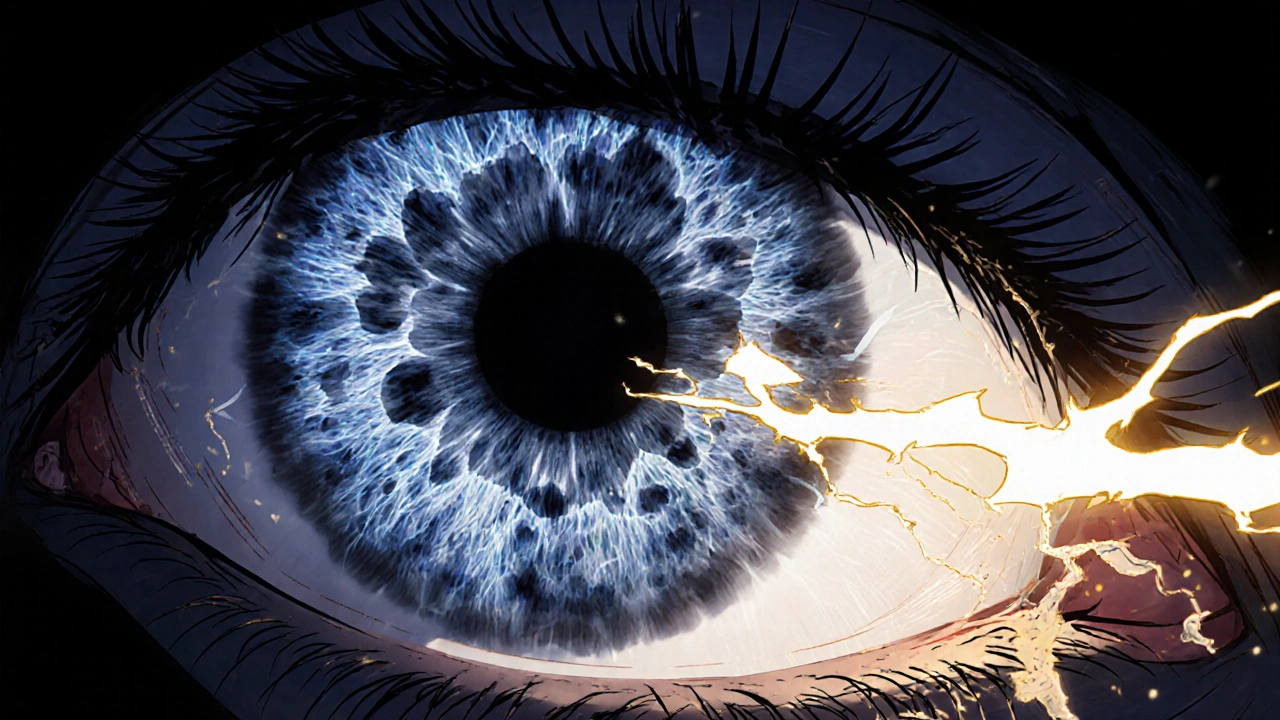
Floaters are those little shapes that seem to float when you move your eyes. They might look like specks, threads, or tiny spiders. They’re most noticeable against plain backgrounds - like a blue sky or a blank computer screen. They drift with your gaze but never quite land where you try to focus. Flashes are brief bursts of light, often seen in your peripheral vision. They can look like sparks, streaks, or lightning bolts - even when your eyes are closed. These aren’t problems with your eyesight itself. They’re caused by changes inside your eyeball, specifically in the vitreous. This is the clear, gel-like substance that fills the space between your lens and your retina. It’s mostly water, but it also contains a network of collagen fibers that give it structure. As you age, that gel starts to break down. It becomes more liquid, shrinks, and pulls away from the retina. This process is called posterior vitreous detachment (PVD).Why Do Floaters and Flashes Happen?
When the vitreous gel shrinks and pulls away, it can tug on the retina. That tug sends a signal to your brain - and your brain interprets it as a flash of light. That’s why you see flashes. The collagen fibers that clump together as the gel breaks down cast shadows on your retina. Those shadows are the floaters. This isn’t something that happens overnight. It’s a slow process that begins in your 40s but becomes common after 50. By age 65, about 75% of people have experienced floaters. By 70, nearly two out of three people have had a posterior vitreous detachment. It’s a normal part of aging - like gray hair or needing reading glasses. But here’s the catch: sometimes, when the vitreous pulls away, it doesn’t do so gently. If it’s stuck to the retina in certain spots, it can tear the retina as it detaches. That’s when things get serious.When Are Floaters and Flashes Dangerous?
Most of the time, floaters and flashes are harmless. But there are red flags that mean you need to see an eye doctor right away:- Sudden increase in floaters - like a shower of new spots appearing all at once
- Flashes that keep coming - especially if they happen in clusters or repeatedly over minutes or hours
- A dark curtain or shadow moving across your vision
- Loss of side vision - like something’s blocking part of your view
- Blurry or distorted vision that doesn’t go away
Who’s at Higher Risk?
Not everyone is equally likely to develop complications. Some people are more vulnerable:- People over 65 - the older you are, the more likely you are to have PVD
- Nearsighted individuals - people with myopia often develop PVD 10 to 15 years earlier because their eyes are longer, putting more stress on the vitreous-retina connection
- Those who’ve had eye surgery - cataract surgery increases the risk of vitreous changes
- People with diabetes - high blood sugar can damage blood vessels in the eye, leading to bleeding into the vitreous, which looks like sudden floaters
- Anyone who’s had eye trauma - even an old injury can cause changes years later
What Happens at the Eye Doctor?
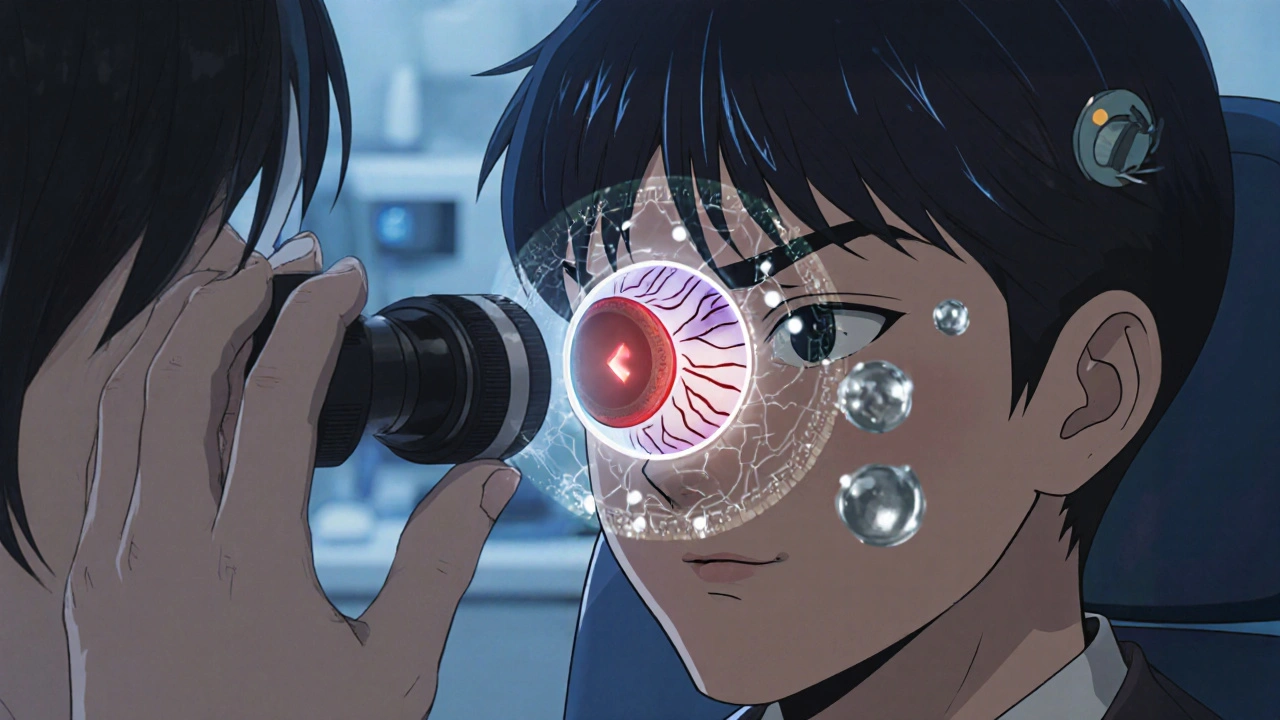
If you’re worried, your eye doctor won’t just glance at your eyes. They’ll dilate your pupils with drops. That lets them see the back of your eye clearly - including the retina and the vitreous. Using a special lens, they’ll look for signs of tears, detachment, or bleeding. This exam takes about 20 minutes. It’s not uncomfortable. The drops might make your vision blurry for a few hours, and you’ll be sensitive to light. But it’s the only way to know for sure whether you’re dealing with a harmless PVD or something that needs treatment. Most people don’t need surgery. If it’s just PVD, the doctor will tell you to wait. Over time, your brain learns to ignore the floaters. They don’t disappear - but they often settle below your line of sight and become less noticeable. Within six months, most people barely notice them anymore.What About Treatments for Floaters?
There are procedures that claim to remove floaters - like laser treatment (vitreolysis) or surgery (vitrectomy). But they’re not for everyone. Laser vitreolysis uses a YAG laser to break up large floaters. It’s not widely covered by insurance in the U.S. because studies haven’t proven it’s consistently safe or effective. It can cause side effects like increased eye pressure or retinal damage if done incorrectly. Vitrectomy is surgery to remove the vitreous gel and replace it with a saline solution. It’s only recommended for extreme cases - like when floaters are so thick they block vision completely, or when there’s a lot of bleeding. The risks include cataracts, retinal detachment, and infection. For 95% of people, the best treatment is time and patience. Your brain adapts. The floaters settle. And you learn to live with them.What Should You Do If You Notice New Symptoms?
Here’s a simple guide:- If you get one or two new floaters with no flashes - schedule an appointment within 24 to 48 hours.
- If you get many new floaters or repeated flashes - go to the eye doctor the same day.
- If you see a dark curtain or loss of side vision - go to the emergency room or call your eye doctor immediately. Don’t wait.
- If you’ve had PVD before and notice a change in your symptoms - get checked again. Something new could be developing.
Can You Prevent Floaters and Flashes?
No - you can’t stop aging. And PVD is just part of it. But you can reduce your risk of complications:- Control your blood sugar if you have diabetes
- Manage your blood pressure
- Wear sunglasses outdoors - UV exposure may speed up vitreous degeneration
- Avoid heavy lifting or sudden head movements if you’ve recently had PVD - this reduces pressure on the eye
What Happens After Diagnosis?
If your doctor confirms it’s just PVD, you’ll probably be told to come back in a few months for a check-up. That’s standard. Even if you feel fine, they want to make sure nothing developed in the meantime. If you have a retinal tear, they’ll treat it with laser or freezing therapy (cryopexy) to seal the tear and prevent detachment. It’s quick, outpatient, and highly effective. Most people don’t even need painkillers afterward. If it’s a detachment, surgery is needed - but the sooner it’s done, the better the outcome. Studies show that when treated within 24 hours, over 90% of retinal detachments can be repaired with good vision restored.Final Thoughts
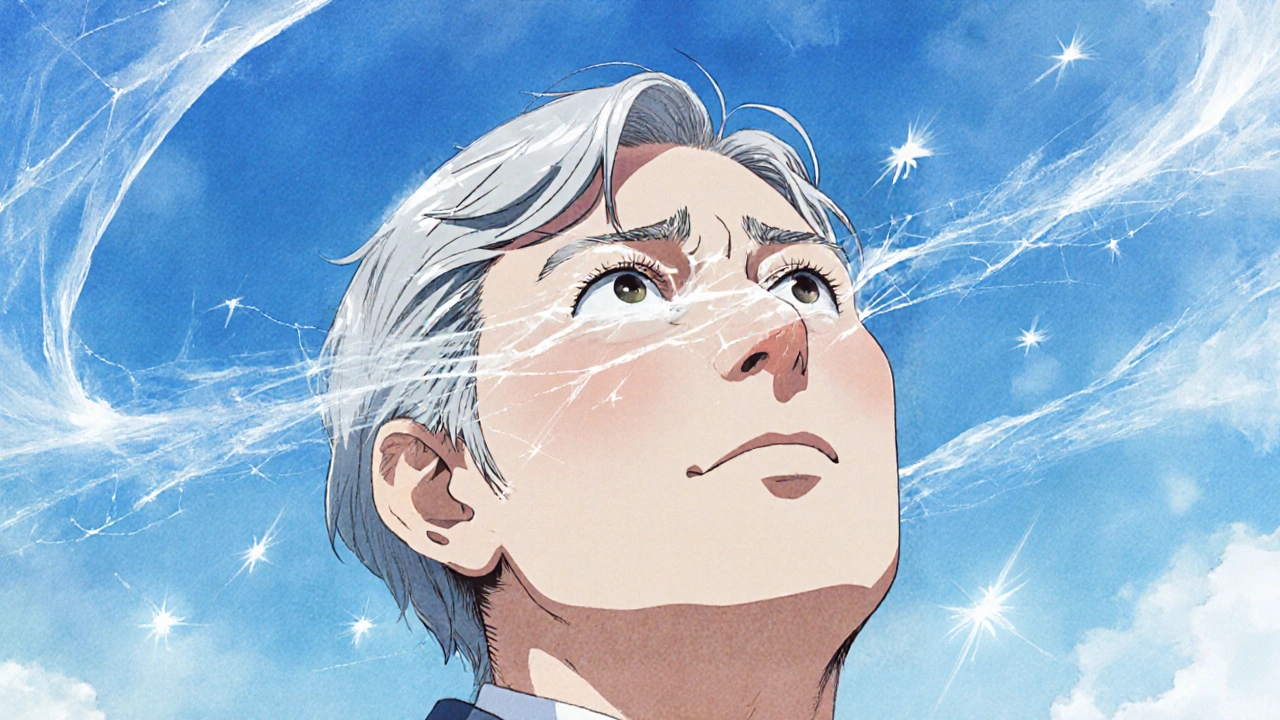
Floaters and flashes aren’t something to panic about - but they’re not something to ignore, either. For most people, they’re just a quiet reminder that your body is aging. For a small number, they’re a signal that something urgent is happening. If you’ve noticed new floaters or flashes, don’t wait. Don’t assume it’s nothing. Don’t wait until your next routine eye exam. Make the call. Get checked. Your vision is worth it.Are floaters and flashes always a sign of a serious eye problem?
No. Most floaters and flashes are caused by posterior vitreous detachment (PVD), a normal part of aging. About 75% of people over 65 experience them. They’re usually harmless and become less noticeable over time as your brain adapts. But sudden changes - like a flood of new floaters or repeated flashes - can signal a retinal tear or detachment, which requires immediate care.
How long do floaters last?
Floaters from PVD typically settle within six months. The debris moves forward in the eye, out of your central vision, and your brain learns to ignore them. Some people notice them for a year or longer, but they rarely get worse. If floaters suddenly increase in number or change shape after months of stability, it’s a sign to get checked again.
Can eye drops or vitamins get rid of floaters?
No. There are no eye drops, supplements, or vitamins proven to eliminate floaters. Claims about lutein, omega-3s, or antioxidants helping floaters are not backed by clinical evidence. The only effective treatments are laser vitreolysis or vitrectomy - and those are reserved for rare, severe cases. For most people, time and adaptation are the only solutions.
Why do flashes happen more often at night or in dim light?
Flashes occur when the vitreous pulls on the retina. In dim light, your pupils are wider, letting in more peripheral light. This makes you more aware of the brief sparks caused by vitreous traction. Also, in low light, your eyes are more sensitive to movement and contrast, so flashes stand out more against dark backgrounds. They’re not happening more often - you’re just noticing them more.
Can floaters cause permanent vision loss?
Floaters themselves don’t cause vision loss. But they can be a symptom of something that does - like a retinal tear or detachment. If the retina detaches and isn’t treated quickly, permanent blindness can occur. That’s why sudden new floaters, especially with flashes, need urgent evaluation. The floaters are the warning sign, not the cause.
Should I avoid exercise if I have floaters?
Not unless you’ve been told otherwise by your eye doctor. Normal activities like walking, swimming, or lifting light weights are fine. But if you’ve recently had a retinal tear or detachment, your doctor may advise avoiding heavy lifting, intense cardio, or activities that involve sudden head movements. Always ask your doctor for personalized advice based on your diagnosis.





Joe Durham
November 20, 2025 AT 21:20I used to think floaters were just my brain playing tricks, especially after staring at my laptop all day. Then I got one of those sudden showers of them last year-like a snowstorm in my eye. Scared the hell out of me. Went to the doc right away, turned out it was just PVD, no tear. Still see ‘em sometimes, but now I know they’re not the enemy. Just old age giving me a visual glitch.
Don’t panic, but don’t ignore it either. Your eyes don’t yell-they whisper. Listen before it’s too late.
Derron Vanderpoel
November 22, 2025 AT 01:27OMG YES I THOUGHT I WAS GOING BLIND ONE NIGHT LMAO. One minute i’m watching netflix, next minute my left eye is full of floating spiders and lightning. Called my mom screaming, she’s a nurse, told me to GTFO to the ER. Turns out i had a tiny retinal tear. Got lasered the next day. No big deal now, but if i’d waited? Could’ve lost that eye. Don’t be dumb like me. If it feels weird-GO. NOW.
Timothy Reed
November 23, 2025 AT 13:48This is one of the most clinically accurate and accessible explanations of posterior vitreous detachment I’ve seen outside of an ophthalmology textbook. The distinction between benign PVD and retinal pathology is critical, and the timeline for intervention is clearly laid out.
It’s worth emphasizing that while floaters are common, their sudden onset-especially when accompanied by photopsia-demands prompt evaluation. The 70% increased risk of retinal tear in acute presentations is not a statistical footnote; it’s a clinical imperative.
Primary care providers should be routinely screening for these symptoms in patients over 50, particularly those with myopia or prior ocular surgery. Prevention isn’t about avoiding aging-it’s about recognizing its warning signs.
Christopher K
November 24, 2025 AT 18:11Of course it’s normal. Everything’s normal now. You’re not supposed to feel your body aging-you’re supposed to drink kale smoothies and meditate until your floaters disappear. Meanwhile, the FDA lets Big Pharma sell $200 eye drops that do nothing while real medicine gets buried under 12 pages of ‘trust your body’ nonsense.
They don’t want you to know the truth: your eyes are falling apart, and the system doesn’t care unless you’re rich enough to get a vitrectomy. Go ahead. Wait until your vision’s gone. Then complain on Twitter.
Nick Lesieur
November 26, 2025 AT 03:55lol u guys act like this is some deep mystery. i had floaters since i was 30 and i’m 47 now. they got worse after i did a bunch of heavy lifting. guess what? i didn’t go to the doctor. i just blinked harder. still see ‘em. still see. still alive. still typing. stop being drama queens.
also-why is everyone so scared of eye doctors? it’s just drops and a bright light. not a damn autopsy. u think your retina’s gonna jump out and scream?
Angela Gutschwager
November 27, 2025 AT 11:14My mom lost 40% of her vision because she waited 3 weeks. Don’t be her.
Go. Now. 💔
Andy Feltus
November 28, 2025 AT 05:56Isn’t it funny how we treat our bodies like machines we’re supposed to maintain, but when they start breaking down in quiet, natural ways, we panic like we’ve been betrayed?
Floaters aren’t a failure. They’re a conversation-your eye saying, ‘Hey, I’ve been here 70 years. I’m tired. I’m changing.’
We don’t need to fix everything. We just need to listen. And sometimes, listening means going to the doctor-not because you’re broken, but because you care enough to know what’s happening.
It’s not about fighting aging. It’s about honoring the vessel that carried you this far.
Brian Rono
November 28, 2025 AT 10:19Let’s be real-this whole ‘PVD is normal’ narrative is just the medical-industrial complex’s way of selling you peace of mind so you don’t sue them when your retina detaches because you were told to ‘wait and see.’
And don’t get me started on the ‘brain adapts’ bullshit. Your brain doesn’t adapt-it ignores. Like how you ignore the ticking clock until it explodes. And then? You’re blind.
They’ll tell you laser vitreolysis is risky. Sure. But so is waiting. So is ignoring. So is pretending your eyes aren’t made of glass.
There’s no ‘safe’ path here. Only informed choices. And most people aren’t even given the full picture. They’re handed a pamphlet and a smile. That’s not medicine. That’s management.
seamus moginie
November 28, 2025 AT 11:59My grandad had this exact thing at 72. Went to the doc, got the laser, lived another 15 years with perfect vision. Told him he was lucky. He said, ‘I didn’t get lucky-I got smart.’
Don’t be the guy who regrets not going.