If you or someone you know has been told they have type 2 diabetes, the first thought is usually “what next?”. The good news is that most of the things that raise blood sugar can be changed with clear steps. Below you’ll find the basics: what to look for, how doctors usually treat it, and simple daily habits that really work.
Type 2 diabetes often sneaks in slowly, so you might not notice anything at first. The most common clues are drinking more water, needing to pee a lot, feeling extra tired, and having blurry vision. Some people also report itching around the belly button or unexplained weight loss. If you notice any of these signs, especially together, it’s worth getting a blood test.
Blood‑sugar tests are quick. A fasting glucose over 126 mg/dL or an A1C of 6.5% or higher usually confirms diabetes. Don’t wait for symptoms to get worse – early detection makes management a lot easier.
Doctors often start with lifestyle changes and add medication if needed. Metformin is the most common first‑line drug because it helps the liver use less sugar and improves how the body responds to insulin. If metformin isn’t enough, doctors may add a second medication like a GLP‑1 agonist or a SGLT2 inhibitor.
Food is a huge part of the puzzle. Focus on whole foods: veggies, lean protein, whole grains, and healthy fats. Cutting back on sugary drinks, white bread, and processed snacks lowers spikes. A simple rule is to fill half your plate with non‑starchy veggies, a quarter with protein, and a quarter with whole carbs.
Exercise doesn’t have to be a marathon. Even a brisk 30‑minute walk five times a week can boost insulin sensitivity. If you’re short on time, try short bursts like 10 minutes of climbing stairs or a quick bike ride. Consistency beats intensity for most people.
Keeping track helps you stay on course. Use a free app or a notebook to log meals, activity, and blood sugar readings. When you see a pattern, you can adjust food portions or timing of medication with your doctor’s guidance.
Stress and sleep matter too. High stress releases hormones that raise blood sugar, and poor sleep disrupts insulin. Simple habits like a short meditation, deep‑breathing, or a regular bedtime can make a real difference.
Remember, type 2 diabetes is a chronic condition, but it’s manageable. By knowing the signs, following your doctor’s plan, and making steady lifestyle tweaks, you can keep blood sugar in a healthy range and feel better every day.
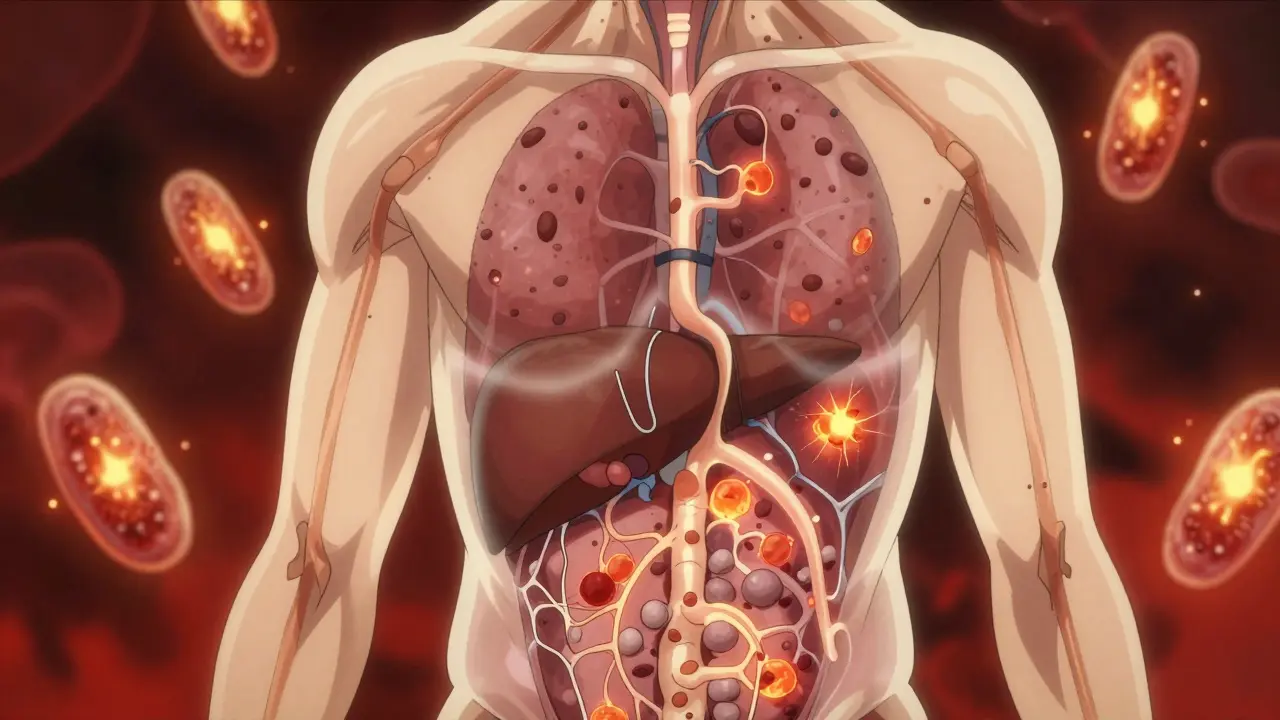
Type 2 diabetes isn't caused by sugar alone - it starts with insulin resistance and metabolic syndrome. Learn how these silent conditions develop, why they're linked to heart disease, and what actually works to reverse them.
Read More
GLP-1 agonists and metformin get compared a lot when it comes to type 2 diabetes treatment. This article unpacks how they stack up on effectiveness, side-effects, and cost. We’ll sift through clinical data, real-world experiences, and financial realities, with practical advice for anyone making choices about diabetes care. Try a look at stats, expert takes, and real-life scenarios to get the clearest answers possible.
Read More